Abstract
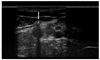
Implanon, a single-rod subdermal contraceptive implant is usually located around the insertion site, Implanon has been usually known to migrate within less than 2 cm of the insertion site and the true migration over 2 cm has been rarely reported. We found a patient whose implanon was located near the brachial neurovascular bundle of left axillary fossa which is about 15 cm upward from the insertion site. We removed it successfully without complication and report the case with literature review.
Figures and Tables
References
1. Hohmann H, Creinin MD. The contraceptive implant. Clin Obstet Gynecol. 2007. 50:907–917.
2. Implanon [Internet]. c2011. cited 2012 Apr 24. Kenilworth, NJ: Merck & Co., Inc;Available from: http://www.implanon.com.
3. Lipetz C, Phillips CJ, Fleming CF. The cost-effectiveness of a long-acting reversible contraceptive (Implanon) relative to oral contraception in a community setting. Contraception. 2009. 79:304–309.
4. Sinofsky FE, Pasquale SA, Levine JP, Christ MF, Alexander NJ. Assessment of ease of Implanon insertion and removal. Obstet Gynecol. 2003. 101:S13.
5. Zheng SR, Zheng HM, Qian SZ, Sang GW, Kaper RF. A randomized multicenter study comparing the efficacy and bleeding pattern of a single-rod (Implanon) and a six-capsule (Norplant) hormonal contraceptive implant. Contraception. 1999. 60:1–8.
6. Kim SY, Huh JS, Chang MY, Hong Y, Choi BR, Baek JH, et al. Removal of non-palpable Implanon(TM) by ultrasound guidance. Korean J Obstet Gynecol. 2010. 53:506–511.
7. Wong RC, Bell RJ, Thunuguntla K, McNamee K, Vollenhoven B. Implanon users are less likely to be satisfied with their contraception after 6 months than IUD users. Contraception. 2009. 80:452–456.
8. Gillies R, Scougall P, Nicklin S. Etonogestrel implants: case studies of median nerve injury following removal. Aust Fam Physician. 2011. 40:799–800.
9. Gun M, Gluis D, Andrews T. Ultrasound appearance and removal of Implanon under ultrasound guidancea pictorial essay. ASUM Bull. 2002. 5:10–12.
10. Lantz A, Nosher JL, Pasquale S, Siegel RL. Ultrasound characteristics of subdermally implanted Implanon contraceptive rods. Contraception. 1997. 56:323–327.
11. Funk S, Miller MM, Mishell DR Jr, Archer DF, Poindexter A, Schmidt J, et al. Safety and efficacy of Implanon, a single-rod implantable contraceptive containing etonogestrel. Contraception. 2005. 71:319–326.
12. Edwards JE, Moore A. Implanon. A review of clinical studies. Br J Fam Plann. 1999. 24:3–16.
13. Evans R, Holman R, Lindsay E. Migration of implanon: two case reports. J Fam Plann Reprod Health Care. 2005. 31:71–72.
14. Phase III clinical trial with Norplant II (two covered rods): report on five years of use. Contraception. 1993. 48:120–132.
15. Oloto EJ, Bromham DR. Norplant removal: a review. Br J Fam Plann. 1995. 21:21–24.
16. Ismail H, Mansour D, Singh M. Migration of Implanon. J Fam Plann Reprod Health Care. 2006. 32:157–159.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download