Abstract
Tubo-ovarian abscess in pregnancy is extremely rare. In this report, we present a patient who had asymptomatic tubo-ovarian abscess during pregnancy. It was diagnosed incidentally immediately after vaginal delivery. Emergency laparotomy was followed and surgical findings included a 4 cm-sized, right, ruptured tubo-ovarian abscess with massive purulent contamination of the whole pelvic cavity. Right salpingo-oophorectomy and massive irrigation were performed.
Cervical mucus plug and intact amniotic membrane protect against ascending infection; therefore, tubo-ovarian abscess (TOA) is an uncommon complication in pregnant women. This complication not only increases maternal morbidity and mortality, but also increases the risk of fetal jeopardy [1]. Proposed pathogeneses of TOA during pregnancy are variable and include hematogenous spreading, lymphatic spreading from contiguous organ, infection in a previously existing ovarian cyst, and flare-up of an old infection [2]. Pelvic inflammatory disease, previous laparotomy, structural genital anomalies, gonococci attached to motile spermatozoa, and the use of assisted reproductive technology are known risk factors for pelvic abscess during pregnancy [3-5]. Review of the case reports in the literature have revealed only a few cases of pregnancy reaching term [6-8]. In this report we present a case who had tubo-ovarian abscess which was incidentally detected after spontaneous abortion of pregnancy at 19 weeks of gestation because of placenta previa with severe bleeding.
Menarche was at 16, menstrual cycle is 30 days and each for 5 days regularly and menstrual amount was moderate.
The patient's expected date of delivery was July 10th, 2012, and she was 18 weeks and 5 days of gestation. She was transferred to our delivery unit with complaints of severe vaginal bleeding with placenta previa totalis and without complaints of abdominal pain.
On admission the patient's vital signs were unremarkable including normal body temperature. There was no sign of rupture of membranes.
At blood test leukocyte was 19,800/mm3, hemoglobin was 8.3 g/dL, platelet was 295,000/mm3 and C-reactive protein was 12.9. Urinalysis, liver function test and renal function test was within normal limit.
Ultrasonography showed a single male fetus of 18 weeks of gestation. Lower edge of the posteriorly located placenta, with the appearance of placenta previa totalis, was covering the whole internal os of cervix (Fig. 1). No adnexal mass was noted on ultrasonography.
Empirical intravenous antibiotics therapy with 3rd cephalosporin and magnesium sulfate and ritodrine therapy for tocolysis were begun immediately. On the seventh day of hospitalization at pregnancy 19 weeks and 4 days, continuous vaginal bleeding was noted. Pelvic examination revealed a cervical os with 3 cm dilation with protruding placenta through the cervix and a 280 g male fetus was delivered spontaneously. We underwent blood test and hemoglobin was 5.4 g/dL. She got transfusion of packed red cell and fresh frozen plasma.
After delivery of the fetus we could find about 15 cm-sized mixed echogenic mass around uterine fundus by ultrasonography (Fig. 2). She underwent abdominal computed tomography and not only abscess in lower abdominal and pelvic cavity but also right tuboovarian abscess were detected (Fig. 3).
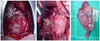
We decided to perform an emergency laparotomy. Laparotomy was performed with a median incision. There was severe adhesion between great omentum and both ovaries covered by pus like material with old inflammation. After adhesiolysis we could find huge abscess around uterus and small bowel. General surgery team came in and omentectomy, appendectomy, adhesiolysis was done. Recovering normal anatomy we found ruptured right tuboovarian abscess and right salpingo-oophorectomy was carried out; the operation was completed with complete irrigation and suction of the entire abdominopelvic cavity. Pus culture which was done during surgery detected Staphylococcus hominis (Fig. 4).
Intravenous antibiotic treatment with 3rd cephalosporin and metronidazole were administered after the operation. The patient recovered well and was discharged 10 days later. Histologic examination confirmed a tubo-ovarian abscess with periappendiceal abscess.
The development of a tubo-ovarian abscess during pregnancy is uncommon. Although a patient with a pelvic abscess in pregnancy usually shows symptoms of infection ranging from fever, lower abdominal pain to sepsis and acute abdomen, tubo-ovarian abscess has rarely been considered as the cause of fever and abdominal pain because of its rare occurrence. Thus, a pelvic abscess during pregnancy must be differentiated from various other conditions. Abdominal pain encountered during pregnancy should be differentiated from various possible causes, including physiologic effects of pregnancy and pathologic conditions related or not related to pregnancy [9]. Physiologic conditions in pregnancy include round ligament pain, uterine torsion and Braxton-Hicks contraction. Pathologic conditions related to pregnancy include spontaneous miscarriage, ischemic uterine leiomyoma, placental abruption, chorioamnionitis, preterm labor, ectopic pregnancy, ovarian hemorrhagic cyst, acute fatty liver of pregnancy, and severe gestational hypertension. Pathologic conditions not related to pregnancy include appendicitis, intestine obstruction, cholecystitis, ovarian torsion, TOA, inflammatory bowel disease, peptic ulcer, acute pancreatitis, urinary tract pathology, sickle cell crisis, porphyria, malaria, arteriovenous hemorrhage, and tuberculosis. Unlike most reported cases, no signs or symptoms attributable to pelvic abscess throughout the pregnancy were observed in our patient.
The proposed mechanisms of tubo-ovarian abscess formation in pregnancy are hematogenous spread from a distant focus; lymphatic spread from an infected cervix; infection of an ovarian cyst; flare-up of a previous infection; an infection after fertilization and before fusion of the decidua parietalis and capsularis; or instrumentation and contiguous spread from adjacent organs [2,9]. All of these possible mechanisms have recently been discussed in a case of ruptured tubo-ovarian abscess in late pregnancy reported by Laohaburanakit and colleauges [6].
Ultrasonography might not be as useful in late gestation as in early gestation or the non-pregnant state for detection of adnexal pathologies because of an enlarged uterus. Tubo-ovarian abscess may not be detected on routine obstetric ultrasonography unless the diagnosis is suspected, as in our case. To ensure accurate diagnosis, laparotomy or laparoscopic intervention should be considered. In recent years, laparoscopy in pregnancy has been a feasible option. But its use is limited in the third trimester owing to an increased risk of injury to the enlarged uterus. It is advisable to make a midline laparotomy incision that can be extended more easily. If obvious abscess is found using radiographic modalities, image-guided percutaneous transcatheter drainage has potential advantages to avoid surgical drainage in some patients. In our case, we did not perform percutaneous transcatheter drainage because of the possible development of toxic signs of sepsis with further delay [10].
The pathogens of tubo-ovarian abscess are variable. It is known that tubo-ovarian abscesses are usually polymicrobial in origin; organisms isolated from tubo-obarian abscesses seem to belong to the facultative anaerobe Enterobacteriaceae family (Escherichia coli, Proteus, Klebsiella) and anaerobic Peptostreptococcus, Streptococcus or Actinomyces [11-14]. In present case, only Staphylococcus hominis was detected.
Most of the cases of tubo-ovarian abscess in pregnancy reported in the literature were managed conservatively as soon as they were recognized during surgery. Pregnant women with unilateral involvement managed with the preservation of the contralateral ovary and the tube had a favorable outcome [15]. In this case, we performed only right salpingo-oophorectomy to preserve reproductive organs as the patient was young and the contralateral adnexa seemed to be free of disease.
Tubo-ovarian abscess in pregnancy is an extremely rare condition. Delayed diagnosis and intervention may cause maternal death or fetal loss. Surgical intervention should be considered if the condition progresses or persists after conservative medical treatment [10]. In this report we have presented a case of tubo-ovarian abscess with no signs or symptoms which was diagnosed incidentally after delivery. This was treated with right salpingo-oophorectomy and antibiotics treatment.
Figures and Tables
Fig. 1
Transvaginal ultrasonography at pregnancy 18+5 weeks showed placenta previa totalis (arrow) covering the whole internal os of cervix (asterisk)

Fig. 2
Transabdominal ultrasonography after termination showed about 15 cm-sized echogenic mass around uterus fundus.

References
1. Jafari K, Vilovick-Kos J, Webster A, Stepto RC. Tubo-ovarian abscess in pregnancy. Obstet Gynecol Surv. 1977. 32:585–587.
2. Cummin RC. Ovarian abscess during pregnancy. J Obstet Gynaecol Br Emp. 1951. 58:1025–1027.
3. James AN, Knox JM, Williams RP. Attachment of gonococci to sperm. Influence of physical and chemical factors. Br J Vener Dis. 1976. 52:128–135.
4. Sherer DM, Schwartz BM, Abulafia O. Management of pelvic abscess during pregnancy: a case and review of the literature. Obstet Gynecol Surv. 1999. 54:655–662.
5. Sogaard Andersen E, Nielsen GL. The combination of pregnancy and acute salpingitis in a case of uterus didelphys. Acta Obstet Gynecol Scand. 1988. 67:175–176.
6. Laohaburanakit P, Treevijitsilp P, Tantawichian T, Bunyavejchevin S. Ruptured tuboovarian abscess in late pregnancy. A case report. J Reprod Med. 1999. 44:551–555.
7. Fuselier P, Alam A. Pregnancy complicated by pelvic abscess. J Reprod Med. 1978. 21:257–258.
8. Sukcharoen N, Witoonpanich P. Pelvic actinomycosis in pregnancy: a case report and review of the literature. J Med Assoc Thai. 1992. 75:66–71.
9. Blanchard AC, Pastorek JG 2nd, Weeks T. Pelvic inflammatory disease during pregnancy. South Med J. 1987. 80:1363–1365.
10. Chen YF, Hsu ST, Ho ES, Chou MM, Tseng JJ. Tuboovarian abscess in pregnancy. Taiwan J Obstet Gynecol. 2008. 47:370–371.
11. Myers SA, Benavides E, Alrenga DP, Freese U. Ovarian abscess in mid-trimester. Colo Med. 1980. 77:133–134.
12. Davey MM, Guidozzi F. Ruptured tubo-ovarian abscess late in pregnancy. A case report. S Afr Med J. 1987. 71:120–121.
13. de Clercq AG, Bogaerts J, Thiery M, Claeys G. Ovarian actinomycosis during first-trimester pregnancy. Adv Contracept. 1987. 3:167–171.
14. Dashow EE, Cotterill R, BeMiller D. Ruptured tuboovarian abscess in early gestation. A case report. J Reprod Med. 1990. 35:418–419.
15. Baydoun AB, Sarram M. Ovarian abscess in pregnancy. Obstet Gynecol. 1961. 18:739–743.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download