Abstract
Mesenteric cysts are usually not considered in the differential diagnosis of pelvic cystic masses. The more common considerations for pelvic cystic masses include ovarian cysts such as, endometrioma, dermoid cyst, and other neoplasm. Here we report a case of 15-year-old girl with pelvic cystic mass; it was initially thought to be ovarian endometrioma, but the operative and histologic findings revealed a mesenteric cyst.
Mesenteric cysts are rare disease and usually not considered in the differential diagnosis of pelvic cystic masses. Since most mesenteric cysts are usually asymptomatic, they tend to be diagnosed incidentally during imaging tests or surgery [1]. In order to exclude malignant transformation and prevent further complications, large mesenteric cysts are recommended to be removed. Complete surgical resection is the treatment of choice with the excellent long-term prognosis [2].
Here we report a case of incidental mesenteric cyst, which was confused with ovarian endometrioma in preoperative assessment.
A 15-year-old girl presented with history of irregular menstruation and an incidental pelvic cystic mass. The patient did not complain of dysmenorrhea, and denied sexual activity. The past medical history was unremarkable.
Laboratory tests including complete blood cell count and renal and liver function tests were all normal, except slightly increased alanine aminotransferase (ALT) (68 IU/L). The level of CA-125, CA-19-9, and carcinoembryonic antigen were 20.6 IU/mL, 0.6 IU/mL, and 1.9 ng/mL, respectively (all were within normal range).
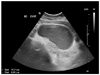
In computed tomographic scan (CT), the cystic mass was 10.5 × 7.9 × 7.6 cm sized, unilocular shaped, and had relatively thick and prominent wall. It was supposed that the cyst doesn't contain fat component or calcified materials. The origin of cystic mass was supposed to be her right ovary (Fig. 1). In addition, considering its homogeneously hypoechoic cyst fluid and thick wall in ultrasonogram (Fig. 2), the cystic mass was thought to be right ovarian endometrioma.
Based on the clinical impression of an ovarian endometrioma, laparoscopic approach was planned to perform right ovarian cystectomy. During the operation, it was confirmed that the origin of the cystic mass was not ovary, but mesentery (Fig. 3A). Both ovaries were intact (Fig. 3B).
To define and make delicate resection, surgical approach was changed into laparotomy. Examining bowel and mesentery, it was confirmed that the cystic mass was originated from mesentery which was 50 cm above ileocecal valve. It was surgically removed, clearly. Exploration of jejunum, ileum, cecum, and appendix was followed, and intactness was confirmed. The postoperative recovery was uneventful.
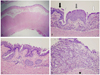
Examination of the specimen showed a cyst filled with mucoid fluid. The cyst was lined by respiratory epithelium and focal squamous epithelium with glandular structure. Disoriented smooth muscle wall was also observed (Fig. 4). Combining these features, the cyst was consistent with enterogenous cyst, and the diagnosis of mesenteric cyst was made.
Mesenteric cysts are rare intra-abdominal disease, identified in about 1 out of 100,000 admissions in adults and 1 out of 20,000 in children [1]. Mesenteric cysts are known to occur in every part of mesentery, and the most common site is small bowel mesentery (ileum in 60%) and next is mesocolon (ascending colon in 40%). Although etiology and classifications are still controversial, mesenteric cysts are clinically divided into 6 groups based on histopathological features: lymphatic origin; mesothelial origin; enteric origin; urogenital origin; mature cystic teratoma; nonpancreatic pseudocysts with traumatic or infectious origin [2].
Most mesenteric cysts are asymptomatic; therefore correct diagnosis is difficult and incidentally diagnosed during imaging tests or surgery in many cases. Disease-related symptoms include abdominal distension, pain, and/or palpable abdominal lumps [3]. Some patients can develop acute abdomen in case of complicated cysts, such as infection, hemorrhage, torsion, rupture, or bowel obstruction [4-6].
In diagnosis of mesenteric cysts, ultrasonography is the first-line diagnostic method [7]. Other image modalities including plain abdominal radiographs, gastrointestinal study using barium, CT, and magnetic resonance imaging (MRI) could be used in selected patients. Especially, CT and MRI could be more informative in measuring the exact extension and association with bowels [8]. However, if a mesenteric cyst locates within the pelvic cavity, as like our case, it may be misdiagnosed as an ovarian cyst [9].
It has been recommended that large mesenteric cysts are removed in order to exclude malignant transformation and prevent further complications [2]. The treatment of choice is complete surgical resection, and sometimes it may need bowel resection. A relation of the mesenteric cyst with the major abdominal vessels should be considered, and if needed, careful and accurate dissection should be performed. Furthermore, there is one case report documenting successful excision of the mesenteric cyst by laparoscopic operations. Laparoscopy is regarded as a feasible method in selected patients [10].
Here we report a case of mesenteric cyst confused with ovarian endometrioma. The patient showed irregular menstruations only, and no other specific symptoms were noted. By the images, a pelvic cystic mass was founded incidentally. In practice, mesenteric cysts are usually not considered in the differential diagnosis of pelvic cystic masses. The more common considerations for pelvic cystic masses include ovarian cysts such as, endometrioma, dermoid cyst, and neoplasm. Thus we suggest that mesenteric cysts should also be considered in the differential diagnosis of pelvic cystic masses.
Figures and Tables
Fig. 1
Computed tomography images showed a unilocular shaped cystic mass without fat and/or calcification. Its origin was supposed to be right ovary.
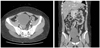
Fig. 3
Intra-operative findings. (A) The origin of cystic mass was mesentery. (B) Both ovaries were intact.

Fig. 4
Microphotographs. (A) Cyst wall on low grade magnification. (B-D) Lined by respiratory epithelium (black arrow and C) and focal squamous epithelium (gray arrow) with glandular structure (white arrow and D). Disoriented smooth muscle wall was also observed (star). (A, ×10; B-D, ×200, H&E stain).
References
1. Vanek VW, Phillips AK. Retroperitoneal, mesenteric, and omental cysts. Arch Surg. 1984. 119:838–842.
2. de Perrot M, Bründler M, Tötsch M, Mentha G, Morel P. Mesenteric cysts. Toward less confusion? Dig Surg. 2000. 17:323–328.
3. Egozi EI, Ricketts RR. Mesenteric and omental cysts in children. Am Surg. 1997. 63:287–290.
4. Fitoz S, Atasoy C, Ekim M, Yildiz S, Erden A, Aktug T. Torsion of a giant omental cyst mimicking ascites. J Clin Ultrasound. 2007. 35:85–87.
5. Ozdoğan M. Acute abdomen caused by a ruptured spontaneously infected mesenteric cyst. Turk J Gastroenterol. 2004. 15:120–121.
6. Kim EJ, Lee SH, Ahn BK, Baek SU. Acute abdomen caused by an infected mesenteric cyst in the ascending colon: a case report. J Korean Soc Coloproctol. 2011. 27:153–156.
7. Mihmanli I, Erdogan N, Kurugoglu S, Aksoy SH, Korman U. Radiological workup in mesenteric cysts: insight of a case report. Clin Imaging. 2001. 25:47–49.
8. Okur H, Küçükaydin M, Ozokutan BH, Durak AC, Kazez A, Köse O. Mesenteric, omental, and retroperitoneal cysts in children. Eur J Surg. 1997. 163:673–677.
9. Long CY, Wang CL, Tsai EM. Incidental diagnosis of a mesenteric cyst mimicking an ovarian cyst during laparoscopy. Taiwan J Obstet Gynecol. 2011. 50:388–389.
10. Tebala GD, Camperchioli I, Tognoni V, Noia M, Gaspari AL. Laparoscopic treatment of a huge mesenteric chylous cyst. JSLS. 2010. 14:436–438.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download