Abstract
Objective
The purpose of this study was to evaluate the ability of the four malignancy risk indices for discrimination of a benign mass from a malignant pelvic mass.
Methods
This is a retrospective study of 547 women admitted to the Department of Obstetrics and Gynecology of Inha University College of Medicine, between January, 2007, and December, 2010, for surgical exploration of a pelvic mass. Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of four risk of malignancy indices (RMIs: RMI 1, RMI 2, RMI 3, and RMI 4) were obtained for diagnosis of a malignant pelvic mass.
Results
Results of receiver operating characteristic analysis of RMI 1-4, CA-125 serum levels, ultrasound score, menopausal status, and tumor size showed values of the area under the curve of 0.9233, 0.9151, 0.9132, 0.9263, 0.8472, 0.9007, 5870, and 0.7714, respectively. The four RMIs showed statistical significance with menopausal status (P=0.001) and tumor size (P=0.03), but not with CA-125 and ultrasound score (P>0.05).
Due to its bizarre and atypical behavior, accurate diagnosis of a pelvic mass prior to exploration of the pelvic cavity by laparotomy or laparoscopy is a challenge to the gynecologist. Pelvic mass is one of the most common clinical presentations, representing a number of benign and malignant conditions. Beforehand knowledge of whether an ovarian neoplasm is benign or malignant can allow for planning of optimal treatment. Appropriate first-line therapy may have a significant influence on the prognosis for women with ovarian cancer [1-6]. Performance of aggressive cytoreductive surgery demands specific skills and experience, which is often beyond the skill of general gynecologists [7,8]. Adoption of a method for better preoperative discrimination of a pelvic mass would result in more women receiving first-line therapy from adequately trained and experienced personnel. For such referrals to be efficient, specific and sensitive improved methods for diagnosis of ovarian cancer are needed.
For clinical use, the diagnostic accuracy of demographic, sonographic and biochemical variables alone is poor. The risk of malignancy index (RMI) was developed by Jacobs et al. [9] for use in referral of relevant patients to gynecologic oncologic centers. The RMI was the first diagnostic model to combine demographic, sonographic and biochemical data in assessment of patients with pelvic masses. The risk of malignancy index is the product of the ultrasound scores (U), the menopausal score (M), and the absolute value of serum CA-125 levels: RMI=U × M × CA-125.
The RMI, now termed RMI 1, was developed in the 1990s by Jacobs et al. [9]. Tingulstad et al. [10] developed their version of the RMI in 1996, which is now known as RMI 2. In 1999, Tingulstad et al. [11] modified the RMI, termed RMI 3. Yamamoto et al. [12], who created their own model of a malignancy risk index, added the parameter of tumor size (S) to the RMI, and have termed it RMI 4.
Retrospective and prospective validation of the four versions of the RMI have been conducted in different clinical studies [9-24], where a cutoff value of 200 for RMI 1-3 and 450 for RMI 4 showed the best discrimination between benign and malignant pelvic masses, with high levels of sensitivity and specificity (sensitivity 51%-90%, specificity 51%-97%).
The main advantage of four RMIs is that it is a simple scoring system that can be applied directly into clinical practice without the introduction of expensive or complicated methods (such as computed tomography scan, magnetic resonance imaging, and whole-body positron emission tomography). The RMIs can be applied in less specialized centers.
The purpose of this study was to evaluate the ability of the four malignancy risk indices for discrimination of a benign mass from a malignant pelvic mass.
This is a retrospective study. Clinical data were obtained from 547 women with a pelvic mass, who were scheduled to undergo laparotomy and laparoscopy at the Department of Obstetrics and Gynecology of Inha University hospital between January, 2007, and December, 2010. Patients' preoperative serum CA-125 levels, ultrasound findings, and menopausal status were noted. Ultrasound was performed transvaginally using a 7.5 MHz transducer (Acuvix XQ, Medison, Korea) in all cases; an abdominal scan was also conducted when indicated. A score was assigned for the following ultrasound features, which are suggestive of malignancy: presence of a multilocular cystic lesion, solid areas, bilateral lesions, ascites, and intraabdominal metastases, which each received a score of one point. Thus, a total ultrasound score (U) was calculated for each patient. Ultrasound was performed for measurement of tumor size (S) for each patient. The ultrasounds were performed by gynecologic oncologists, general gynecologists, or residents (under the supervision of gynecologist).
Postmenopausal status was defined as more than one year of amenorrhea or age older than 50 years in women who had undergone hysterectomy. All other women were considered premenopausal. Serum samples were collected preoperatively and measurement of serum CA-125 was performed using Electrochemiluminescence Immunoassaay (ECLIA). Based on the data obtained, RMI 1, RMI 2, RMI 3, and RMI 4 were calculated for all patients together with the sensitivity, specificity, diagnostic accuracy, and positive and negative predictive values of the four methods as follows:
1) RMI 1 (Jacobs et al. [9], 1990)=U×M×CA-125, where a total ultrasound score of 0 made U=0, a score of 1 made U=1, and a score of ≥2 made U=3; premenopausal status made M=1 and postmenopausal M=3. The serum level of CA-125 was applied directly to the calculation.
2) RMI 2 (Tingulstad et al. [10], 1996)=U×M×CA-125, where a total ultrasound score of 0 or 1 made U =1, and a score of ≥2 made U=4; premenopausal status made M=1 and postmenopausal M=4. The serum level of CA-125 was applied directly to the calculation.
3) RMI 3 (Tingulstad et al. [11], 1999)=U×M×CA-125, where a total ultrasound score of 0 or 1 made U=1, and a score of ≥2 made U=3; premenopausal status made M=1 and postmenopausal M =3. The serum level of CA-125 was applied directly to the calculation.
4) RMI 4 (Yamamoto et al. [12], 2009)=U×M×S (size in centimeters)×CA-125, where a total ultrasound score of 0 or 1 made U=1, and a score of ≥2 made U=4. Premenopausal status made M =1 and postmenopausal status made M=4. A tumor size (single greatest diameter) of <7 cm made S=1, and ≥7 cm made S=2. The serum level of CA-125 was applied directly to the calculation.
The histopathologic diagnosis was regarded as the definitive outcome. Gynecological cancers were found staged according to the International Federation of Gynecology and Obstetrics (FIGO) classification [25]. Sensitivity was defined as the percentage of patients with malignant disease showing a positive test result. Specificity was defined as the percentage of patients with benign disease showing a negative test result. The positive predictive value was defined as the percentage of patients with a positive test result who had malignant disease and the negative predictive value was defined as the percentage of patients with a negative test result who had benign disease. Accuracy was defined as the percentage of all patients who had malignant disease with a positive test result and benign disease with a negative test result.
The SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) was used in performance of statistical analyses. The χ2-test was used for determination of differences in distribution of age, menopausal status, tumor size, and ultrasound score. The Mann-Whitney U-test was applied when testing differences in distribution of CA-125 among women with benign and malignant pelvic masses. McNemar's test was used when testing differences in performance between RMI 1, RMI 2, RMI 3, and RMI 4. A receiver operating characteristic (ROC) curve was created for demonstration of the relationship between sensitivity and specificity of CA-125, menopausal status, ultrasound score, tumor size, and RMI 1-4 in discrimination between benign and malignant pelvic masses.
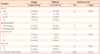
A total of 547 patients were included in the study; 434 patients (79.3%) were diagnosed with benign conditions, whereas 113 patients (20.7%) had malignant disease (Table 1). Malignant tumors included serous cystadenocarcinoma (n=35), mucinous cystadenocarcinoma (n=13), endometrioid carcinoma (n=6), clear cell carcinoma (n=6), transitional cell carcinoma (n=7), granulosa cell tumor (n=6), Yolk sac tumor (n=2), dysgerminoma (n=2), immature teratoma (n=1), Sertoli-Leidig cell tumor (n=1), malignant mixed mullerian tumor (n=2), mullerian adenosarcoma (n=1), Krukenberg's tumor (n=2), and borderline malignancy (n=29). Benign gynecological conditions included mature cystic teratoma (n=184), mucinous cystadenoma (n=85), serous cystadenoma (n=93), endometriosis (n=27), fibroma (n=12), fibrothecoma (n=5), tubo-ovarian abscess (n=5), paratubal cyst (n=6), functional follicle (n=6), struma ovarii (n=3), actinomycosis (n=2), brenner tumor (n=2), sclerosing stromal tumor (n=1), and leiomyoma (n=1).
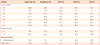
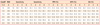
Distribution of benign and malignant cases according to age, menopausal status, ultrasound score, tumor size, and CA-125 is shown in Table 2. Results of univariate analysis showed a significant linear trend for malignancy according to increasing age, postmenopausal state, increasing ultrasound score, large tumor size, and increasing CA-125, respectively. When compared with women with benign disease, a significantly higher mean serum level of CA-125 was observed among women with (507 U/mL vs. 35 U/mL). Data for sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of different levels of serum CA-125, ultrasound score, tumor size, and menopausal status are reported in Table 3. The best performance was obtained for a serum CA-125 level of 40 U/mL. At a serum level of CA-125 40 U/mL, sensitivity for detection of malignancy was 73.4% and specificity was 83.1%, positive and negative predictive values were 53.2% and 92.3%, and diagnostic accuracy was 81.1%, respectively. Data on performance of RMI 1, RMI 2, RMI 3, and RMI 4 at different cutoff values are shown in Table 4. For RMI 1 and RMI 3, the overall best performance was obtained at a cutoff level of 150, and at 200 for RMI 2, and 400 for RMI 4. Direct comparison of the four indices revealed no statistically significant difference in performance of the four methods (McNemar's test, P>0.05). ROC analysis of RMI 1, RMI 2, RMI 3, and RMI 4 showed significantly high values for area under the curve, were significantly high with a value of 0.9233, 0.9151, 0.9132, and 0.9263, respectively. Values for area under the curve for menopausal status, serum CA-125, ultrasound score, and tumor size were 0.5870, 0.8472, 0.9007, and 0.7714, respectively. The four RMIs showed statistical significance with menopausal status (P=0.001) and tumor size (P=0.03), but not with CA-125 and ultrasound score (P>0.05). Data on diagnostic performance of ultrasound score, CA-125, menopausal status, tumor size, RMI 1, RMI 2, RMI 3, and RMI 4 are shown in the receiver-operating characteristic curves (Fig. 1).
Management of the pelvic mass is a common and controversial clinical problem [26]. Malignant tumors should be referred to specialized centers for gynecologic oncologic surgery; therefore, differential diagnosis of benign from malignant tumors is essential in order to decide on the optimal approach in each case. The lack of screening tests for early diagnosis of ovarian cancer is an important determinant of the mortality rate from this disease. Due to the absence or subtlety of early symptoms, more than 70% of patients are diagnosed with advanced-stage ovarian cancer [27]. Four RMIs had some different characteristics. RMI 1 was the first version as developed by Jacobs et al. [9] and gave an ultrasound score (U) of 0 when none of the ultrasound features were present, resulting in an RMI 1 of 0 regardless of the CA-125 level. But, RMI 2-4 had not ultrasound score (U) of 0. Yamamoto et al. [12] have published their study in which RMI 4 was created, that includes tumor size as an additional parameter.
Results of this study demonstrated the ability of four RMIs, ultrasound score, and serum CA-125 to correctly identify benign and malignant pelvic masses. The RMI was originally developed by Jacobs et al. [9], and, subsequently, the same group reproduced the results in a new group of patients, establishing the superiority of RMI over the individual parameter [13]. However, in the present study, four RMIs showed statistical significance with menopausal status and tumor size, but not with CA-125 and ultrasound score. This study has not established the superiority of the four RMIs over the use of CA-125 and ultrasound score, and there was no necessity for using four RMIs instead of CA-125 and ultrasound score.
Findings from the present study demonstrated that the overall best performance in RMI 1 and RMI 3 was obtained at a cut-off level of 150, and at 200 for RMI 2, and 400 for RMI 4. Many authors have suggested a cut-off value for RMI 1-3 of 200 [9-11,16,18]. Using tumor size, Yamamoto et al. [12] developed their own RMI, and named it RMI 4 (using a cutoff level of 450). Using a cut-off of 120, Clarke et al. [28] reported a sensitivity of 72% and a specificity of 87% for RMI 1; RMI 2 showed a sensitivity of 76% and a specificity of 81%; RMI 3 showed a sensitivity of 74% and a specificity of 84%. The lower cut-off values for RMI 1, RMI 3, and RMI 4, obtained in our study may be associated with the higher number of malignant cases in the premenopausal group-56.6% versus 19% [9], and 20% [10].
In our study, we found no statistically significant difference in performance of these four different RMIs for identification of malignancy. However, other investigators have reported that RMI 2 is more reliable in discriminating between benign and malignant disease [10,14]. Tingulstad et al. [10] developed their RMI in 1996 and named it RMI 2. In a direct comparison of their RMI with that developed by Jacobs et al. [9], they found that, at a cut-off level of 200, RMI 2 was significantly better than RMI 1 for prediction of malignancy (McNemar test, P=0.001). Morgante et al. [14] also reported a similar observation that for all cut-off values between 80 and 250, RMI 2 showed better performance than RMI 1 (P=0.0001). In our study, we observed sensitivity and specificity of 79.6% and 79.9% at a cut-off level of 200 for RMI 2.
Tingulstad et al. [11], who modified the RMI (defined RMI 3), observed that, at a cut-off level of 200, sensitivity and specificity were 71% and 92%, respectively. In our study on application of this modified RMI (RMI 3), we observed a sensitivity and specificity of 77.9% and 81.1% at a cut-off level of 150, respectively, which is comparable with results reported by Tingulstad et al. [11].
Results of a study conducted by Manjunath et al. [16] in 2001, which compared RMI 1, RMI 2, and RMI 3, confirmed that there was no statistical difference in benign-malignancy discrimination between these three indices. Results of a study conducted by Aktürk et al. [24] in 2011, which compared RMI 1, RMI 2, RMI3, and RMI 4, confirmed that there was no statistical difference in benign-malignancy discrimination between these four indices. In 2009, Yamamoto et al. [12] developed their own RMI 4, and confirmed that, at a cut-off level of 450, the accuracy of RMI 4 was better than that of RMI 1, RMI 2, and RMI 3, with a cutoff level of 200. They reported that at a cutoff level of 450, sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 86.8%, 91.0%, 63.5%, 97.5%, and 90.4%, respectively [12]. In our study, we observed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 77.9%, 85.9%, 59.1%, 93.7%, and 84.3% at a cutoff level of 400 for RMI 4, respectively, which is comparable with results reported by Yamamoto et al. [12]. However, we also found that the other three indices showed reliable diagnostic performance, which differed from the results of Yamomoto et al. [12].
In assessment of the results of this study, some limitations should be considered. First, clinical data obtained retrospectively from a single institution. Second, training and skill of ultrasonologists should be taken into account.
In conclusion, four RMIs (cutoff level at 150 of RMI 1 and RMI 3, at 200 of RMI 3, and at 400 of RMI 4) were found to be statistically significant diagnostic criteria, compared with menopausal status and tumor size, which can discriminate between benign and malignant pelvic masses.
Figures and Tables
Fig. 1
Receiver operating characteristic (ROC) curves of the individual predictors showing the relationship between sensitivity and specificity of menopause score, ultrasound score, serum CA-125 level, tumor size, and risk of malignancy index (RMI) 1-4 in the discrimination between benign and malignant pelvic masses.

Table 2
The distribution of benign and malignant cases by age, menopausal status, ultrasound score, tumor size, and serum CA-125
References
1. Young RC, Decker DG, Wharton JT, Piver MS, Sindelar WF, Edwards BK, et al. Staging laparotomy in early ovarian cancer. JAMA. 1983. 250:3072–3076.
2. Gillis CR, Hole DJ, Still RM, Davis J, Kaye SB. Medical audit, cancer registration, and survival in ovarian cancer. Lancet. 1991. 337:611–612.
3. Engelen MJ, Kos HE, Willemse PH, Aalders JG, de Vries EG, Schaapveld M, et al. Surgery by consultant gynecologic oncologists improves survival in patients with ovarian carcinoma. Cancer. 2006. 106:589–598.
4. Earle CC, Schrag D, Neville BA, Yabroff KR, Topor M, Fahey A, et al. Effect of surgeon specialty on processes of care and outcomes for ovarian cancer patients. J Natl Cancer Inst. 2006. 98:172–180.
5. Kumpulainen S, Kuoppala T, Leminen A, Penttinen J, Puistola U, Pukkala E, et al. Surgical treatment of ovarian cancer in different hospital categories: a prospective nation-wide study in Finland. Eur J Cancer. 2006. 42:388–395.
6. Goff BA, Matthews BJ, Wynn M, Muntz HG, Lishner DM, Baldwin LM. Ovarian cancer: patterns of surgical care across the United States. Gynecol Oncol. 2006. 103:383–390.
7. McGowan L, Lesher LP, Norris HJ, Barnett M. Misstaging of ovarian cancer. Obstet Gynecol. 1985. 65:568–572.
8. Eisenkop SM, Spirtos NM, Montag TW, Nalick RH, Wang HJ. The impact of subspecialty training on the management of advanced ovarian cancer. Gynecol Oncol. 1992. 47:203–209.
9. Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990. 97:922–929.
10. Tingulstad S, Hagen B, Skjeldestad FE, Onsrud M, Kiserud T, Halvorsen T, et al. Evaluation of a risk of malignancy index based on serum CA125, ultrasound findings and menopausal status in the pre-operative diagnosis of pelvic masses. Br J Obstet Gynaecol. 1996. 103:826–831.
11. Tingulstad S, Hagen B, Skjeldestad FE, Halvorsen T, Nustad K, Onsrud M. The risk-of-malignancy index to evaluate potential ovarian cancers in local hospitals. Obstet Gynecol. 1999. 93:448–452.
12. Yamamoto Y, Yamada R, Oguri H, Maeda N, Fukaya T. Comparison of four malignancy risk indices in the preoperative evaluation of patients with pelvic masses. Eur J Obstet Gynecol Reprod Biol. 2009. 144:163–167.
13. Davies AP, Jacobs I, Woolas R, Fish A, Oram D. The adnexal mass: benign or malignant? Evaluation of a risk of malignancy index. Br J Obstet Gynaecol. 1993. 100:927–931.
14. Morgante G, la Marca A, Ditto A, De Leo V. Comparison of two malignancy risk indices based on serum CA125, ultrasound score and menopausal status in the diagnosis of ovarian masses. Br J Obstet Gynaecol. 1999. 106:524–527.
15. Aslam N, Tailor A, Lawton F, Carr J, Savvas M, Jurkovic D. Prospective evaluation of three different models for the pre-operative diagnosis of ovarian cancer. BJOG. 2000. 107:1347–1353.
16. Manjunath AP, Pratapkumar , Sujatha K, Vani R. Comparison of three risk of malignancy indices in evaluation of pelvic masses. Gynecol Oncol. 2001. 81:225–229.
17. Mol BW, Boll D, De Kanter M, Heintz AP, Sijmons EA, Oei SG, et al. Distinguishing the benign and malignant adnexal mass: an external validation of prognostic models. Gynecol Oncol. 2001. 80:162–167.
18. Torres JC, Derchain SF, Faundes A, Gontijo RC, Martinez EZ, Andrade LA. Risk-of-malignancy index in preoperative evaluation of clinically restricted ovarian cancer. Sao Paulo Med J. 2002. 120:72–76.
19. Andersen ES, Knudsen A, Rix P, Johansen B. Risk of malignancy index in the preoperative evaluation of patients with adnexal masses. Gynecol Oncol. 2003. 90:109–112.
20. Obeidat BR, Amarin ZO, Latimer JA, Crawford RA. Risk of malignancy index in the preoperative evaluation of pelvic masses. Int J Gynaecol Obstet. 2004. 85:255–258.
21. Bailey J, Tailor A, Naik R, Lopes A, Godfrey K, Hatem HM, et al. Risk of malignancy index for referral of ovarian cancer cases to a tertiary center: does it identify the correct cases? Int J Gynecol Cancer. 2006. 16:Suppl 1. 30–34.
22. van Trappen PO, Rufford BD, Mills TD, Sohaib SA, Webb JA, Sahdev A, et al. Differential diagnosis of adnexal masses: risk of malignancy index, ultrasonography, magnetic resonance imaging, and radioimmunoscintigraphy. Int J Gynecol Cancer. 2007. 17:61–67.
23. Ulusoy S, Akbayir O, Numanoglu C, Ulusoy N, Odabas E, Gulkilik A. The risk of malignancy index in discrimination of adnexal masses. Int J Gynaecol Obstet. 2007. 96:186–191.
24. Aktürk E, Karaca RE, Alanbay I, Dede M, Karasahin E, Yenen MC, et al. Comparison of four malignancy risk indices in the detection of malignant ovarian masses. J Gynecol Oncol. 2011. 22:177–182.
25. FIGO Cancer Committee. Staging announcement. Gynecol Oncol. 1986. 25:383–385.
26. Curtin JP. Management of the adnexal mass. Gynecol Oncol. 1994. 55:S42–S46.
27. Goff BA, Mandel L, Muntz HG, Melancon CH. Ovarian carcinoma diagnosis. Cancer. 2000. 89:2068–2075.
28. Clarke SE, Grimshaw R, Rittenberg P, Kieser K, Bentley J. Risk of malignancy index in the evaluation of patients with adnexal masses. J Obstet Gynaecol Can. 2009. 31:440–445.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download