Abstract
Vulvar epithelioid hemangioendothelioma as primary site is extremely rare tumor that may be confused with other mesenchymal tumors due to their rarity and its histologic features. We report a case of 46-year-old woman who presented to hospital with left vulvar mass. The mass was located in subcutaneous area of vulva, and well marginated contrast enhanced on radiologic examination. Local excision was performed. After surgery, she has remained free of disease without recurrence for 6 months. Here we report a case of primary vulvar epithelioid hemangioendothelioma as very rare site and this is the first case in Korea.
Epithelioid hemangiendothelioma is a relatively rare soft tissue tumor, and intermediate malignant vascular tumor. This epithelioid angicentric vascular tumor can occur at almost any age, especially middle-aged patients, but rarely occurs in childhood [1,2]. Epithelioid hemangiendothelioma is mainly solitary, arising in superficial or deep soft tissue, and also occurs in the lung, bone, pleura, liver, peritoneum, lymph node, etc. [3], but case in the vulva is extremely rare. Only one case has been reported in the literature [4]. Here we report a case of primary vulvar hemangioendothelioma as very rare site in 46-year-old women and discuss the clinical and histologic features.
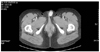
A 46-year-old female was admitted to our hospital because of left vulvar mass that had developed during approximately 1.5 years. The patient had no specific other history including the familial history, and good general status. Computerized tomography (CT) scan showed well marginated contrast enhanced mass, measuring 2.2×1.5 cm, on vulva, and the mass was not adhered and infiltrative around surrounding tissue (Fig. 1).
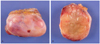
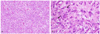
Local excision was performed. The mass was well circumscribed nodular lesion in the subcutis (Fig. 2A), and showed yellow soft cut surface with focally myxoid areas. Because the mass resembled lipoma grossly, we could not offer hint of its vascular origin on gross inspection (Fig. 2B). On light microscopic examination, the tumor had two different intermingled patterns by high cellularity and myxoid area. Epithelioid cells were prominent in high cellular area (Fig. 3A). Intracytoplasmic lumina were sometimes present (Fig. 3B). These findings supported the notion that histologically epithelioid soft tissue tumor arising from vessel. Surgical resected margin involvement was present, but currently evidence of tumor recurrence is not shown during 6 months.
The hemangioendothelioma has become a designation for those was vascular tumors which histologic intermediate in appearance between a hemangioma and a conventional angiosarcoma [5]. Currently, its preferred use is for vascular tumors of an endothelial nature that occupy intermediate position between the benign hemangioma and the full-brown angiosarcoma [6].
The case of epithelioid hemangioendothelioma is relatively rare and, furthermore, has reported only one case arising in vulva as primary site at previous literature. da Silva et al. [4] have reported the first case of vulvar epithelioid hemangioendothelioma, and not reported any case in Korea.
Epithelioid hemangioendothelioma shows typically infiltrative growth pattern. However, purely cutaneous tumors often consist of a fairly circumscribed dermal tumor [2]. Our case also consists of well-circumscribed mass, and shows yellow soft cut surface. This gross finding presents no information of vascular nature, rather requires the discrimination of lipoma and does not offer the hint of vascular originated tumor.
Differential diagnosis includes metastatic carcinoma or melanoma as well as various mesemchymal tumors because of cytologic morphology of epithelioid features. Metastatic carcinomas or melanoma can be distinguished with far more nuclear atypia and mitotic activity than the epithelioid hemangioendothelioma and rarely angiocentric. Epithelioid forms of angiosarcoma may occasionally give rise to confuse diagnosis too. The low mitotic activity (<5/50 HPF), minimal pleomorphism, lack of necrosis and the presence of intracytoplasmic vascular lumen formation should distinguish epithelioid hemangioendothelioma from epithelioid sarcoma [7]. Epithelioid hemangioma should be considered in differential diagnosis [2,7,8]. Epithelioid hemangioma often has a lobular architecture, prominent inflammation, and numerous well-formed blood vessels.
The stroma of epithelioid hemangioendothelioma may have a prominent myxoid appearance. The mesenchymal tumors of myxoid appearance from vulva must be contained as differential diagnosis; aggressive angiomyxoma, angiomyofibroblastoma, fibroepithelial polyp (so-called pseudosarcoma botryoides) and superficial angiomyxoma [9,10].
Because the cytology prior to the surgical treatment cannot always confirm the malignant character, the treatment of choice is the complete local excision of the tumor with or without regional lymphadenectomy [11]. However, as epithelioid hemangioendothelioma is rare and almost always discovered after surgical excision for a supposed benign cause, few patients have undergone complete preoperative investigation to detect the presence of possible metastasis [12]. In addition, it has been reported that possible metastasis might not become evident for many years because of the slow growth of this tumor [12]. Our patient also was thought as probably benign tumor and so underwent local excision only. Furthermore, at microscopic discriptions, resected margin involvement was present. She is currently free from recurrence for 6 months, but further prognosis cannot be known. We will continuously follow up and observe our patient because of uncertain prognosis and presence of resected margin involvement. The role of adjuvant chemotherapy remains unclear. Läuffer et al. [13] and Makhlouf et al. [14] performed adjuvant chemotherapy with hepatic intraarterial 5-fluorouracil, radiotherapy, and/or treatment with interferon-α-2 in cases of epithelioid hemangioendothelioma of the liver. However, the result remained unclear, since the small number of treated cases and the unpredictable evolution of epithelioid hemangioendothelioma does not permit conclusions to be drawn [13,14].
In conclusion, epithelioid hemangioendothelioma is a very rare mesemchymal tumor as primary site of vulva. On gross inspections, it is difficult of doubting vascular-originated tumor, and due to epithelioid feature and myxoid stroma, many other mesenchymal tumors can be included as differential diagnosis. If pathologic confirmation is done appropriately, regular follow-up must be performed after wide resection.
Figures and Tables
Fig. 1
Computerized tomography shows well marginated contrast enhanced mass, measuring 2.2×1.5 cm in sized, on subcutaneous portion of left vulvar area.
References
1. De Young BR, Wick MR, Fitzgibbon JF, Sirgi KE, Swanson PE. CD31: an immunospecific marker for endothelial differentiation in human neoplasm. Appl Immunohistochem. 1993. 1:97–100.
2. Elder DE, Elentitsas R, Johnson BL, Murphy GF, Xu X. Lever's histopathology of the skin. 2005. 9th ed. Philadelphia (PA): Lippincott Williams & Wilkins.
3. Yousem SA, Hochholzer L. Unusual thoracic manifestations of epithelioid hemangioendothelioma. Arch Pathol Lab Med. 1987. 111:459–463.
4. da Silva BB, Lopes-Costa PV, Furtado-Veloso AM, Borges RS. Vulvar epithelioid hemangioendothelioma. Gynecol Oncol. 2007. 105:539–541.
5. Enzinger FM, Weiss SW. Soft tissue tumors. 1995. 3rd ed. St. Louis (MO): Mosby.
6. Angervall L, Kindblom LG, Karlsson K, Stener B. Atypical hemangioendothelioma of venous origin. A clinicopathologic, angiographic, immunohistochemical, and ultrastructural study of two endothelial tumors within the concept of histiocytoid hemangioma. Am J Surg Pathol. 1985. 9:504–516.
7. Naqvi J, Ordonez NG, Luna MA, Williams MD, Weber RS, El-Naggar AK. Epithelioid hemangioendothelioma of the head and neck: role of podoplanin in the differential diagnosis. Head Neck Pathol. 2008. 2:25–30.
8. Kabukçuoğlu F, Kabukçuoğlu Y, Livaoğlu A, Ozağari A, Armagan R, Kuzgun U. Epithelioid hemangioendothelioma of bone. Acta Orthop Traumatol Turc. 2006. 40:324–328.
9. Granter SR, Nucci MR, Fletcher CD. Aggressive angiomyxoma: reappraisal of its relationship to angiomyofibroblastoma in a series of 16 cases. Histopathology. 1997. 30:3–10.
10. Nucci MR, Granter SR, Fletcher CD. Cellular angiofibroma: a benign neoplasm distinct from angiomyofibroblastoma and spindle cell lipoma. Am J Surg Pathol. 1997. 21:636–644.
11. Gherman CD, Fodor D. Epithelioid hemangioendothelioma of the forearm with radius involvement: case report. Diagn Pathol. 2011. 6:120.
12. Al-Faky YH, Al Malki S, Raddaoui E. Hemangioendothelioma of the eyelid can mimic chalazion. Oman J Ophthalmol. 2011. 4:142–143.
13. Läuffer JM, Zimmermann A, Krähenbühl L, Triller J, Baer HU. Epithelioid hemangioendothelioma of the liver: a rare hepatic tumor. Cancer. 1996. 78:2318–2327.
14. Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999. 85:562–582.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download