Abstract
Objective
To estimate the absolute increase in the risk for adverse neonatal outcomes of fetal growth restriction between late preterm and term birth and to identify risk factors for neonatal morbidity among late preterm and term birth infants.
Methods
A retrospective review of 2,954 singleton infant between 34 and 42 weeks of gestation born at our hospital over the 5 years were enrolled and they were divided into four groups as late preterm small for gestational age (SGA), late preterm adequate for gestational age (AGA), term SGA and term AGA, respectively. The prenatal ultrasonographic findings between SGA and AGA in late preterm birth were assessed. Maternal and neonatal complications were compared with SGA and AGA between late preterm and term birth infants. The statistical analyses for frequencies and relative risks in each group were calculated by SPSS ver. 19.0.
Results
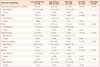
In prenatal evaluation between SGA and AGA in late preterm birth, amniotic fluid volume, abdominal circumference and umbilical artery Doppler resistance index value were different significantly (P<0.001). Preeclampsia and oligohydramnios were found more common in SGA of late preterm birth compared with AGA of term birth. Jaundice, respiratory distress syndrome, necrotizing enterocolitis, sepsis, congenital anomalies, hypoglycemia, and germinal matrix's hemorrhage, occurred more frequent in SGA of late preterm birth than in AGA of term birth.
Figures and Tables
Fig. 1
SGA and AGA in late preterm birth and term birth infants for 5 years. SGA, small for gestational age; AGA, adequate for gestational age; PT, (late) preterm; T, term.
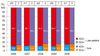
Table 2
Prenatal evaluation between SGA and AGA in late preterm birth
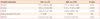
Values are presented as mean ± standard deviation or number.
SGA, small for gestational age; AGA, appropriate for gestation age; AFI, amniotic fluid index; AC, abdominal circumference; UmA, umbilical artery; RI, resistance index; EDF, end-diastolic flow; MCA, middle cerebral artery; N/A, not applicable.
aAbsent flow 2, reversed flow 1.
References
1. Morse SB, Zheng H, Tang Y, Roth J. Early school-age outcomes of late preterm infants. Pediatrics. 2009. 123:e622–e629.
2. Mathews TJ, MacDorman MF. Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl Vital Stat Rep. 2007. 55:1–32.
3. Soregaroli M, Bonera R, Danti L, Dinolfo D, Taddei F, Valcamonico A, et al. Prognostic role of umbilical artery Doppler velocimetry in growth-restricted fetuses. J Matern Fetal Neonatal Med. 2002. 11:199–203.
4. Lee GH, Kim YW, Lee KB, Seo EJ, Son MS, Ahn HG, et al. Change of birth weight-gestational age table. Korean J Obstet Gynecol. 2001. 44:1851–1856.
5. Hamilton BE, Martin JA, Ventura JS, Ventura JS. Births: preliminary data for 2006. Natl Vital Stat Rep. 2007. 56:1–18.
6. Mathews TJ, Macdorman MF. Infant mortality statistics from the 2006 period linked birth/infant death data set. Natl Vital Stat Rep. 2010. 58:1–32.
7. Reddy UM, Ko CW, Raju TN, Willinger M. Delivery indications at late-preterm gestations and infant mortality rates in the United States. Pediatrics. 2009. 124:234–240.
8. Laughon SK, Reddy UM, Sun L, Zhang J. Precursors for late preterm birth in singleton gestations. Obstet Gynecol. 2010. 116:1047–1055.
9. Joseph KS, Demissie K, Kramer MS. Obstetric intervention, stillbirth, and preterm birth. Semin Perinatol. 2002. 26:250–259.
10. Davidoff MJ, Dias T, Damus K, Russell R, Bettegowda VR, Dolan S, et al. Changes in the gestational age distribution among U.S. singleton births: impact on rates of late preterm birth, 1992 to 2002. Semin Perinatol. 2006. 30:8–15.
11. Alberry M, Soothill P. Management of fetal growth restriction. Arch Dis Child Fetal Neonatal Ed. 2007. 92:F62–F67.
12. Committee on Obstetric Practice. ACOG committee on Obstetric Practice. Intrauterine growth restriction. Int J Gynaecol Obstet. 2000. 1:67–75.
13. Ferrazzi E, Bulfamante G, Mezzopane R, Barbera A, Ghidini A, Pardi G. Uterine Doppler velocimetry and placental hypoxic-ischemic lesion in pregnancies with fetal intrauterine growth restriction. Placenta. 1999. 20:389–394.
14. Committee on Practice Bulletins--Gynecology, American College of Obstetricians and Gynecologists, Washington, DC 20090-6920, USA. Intrauterine growth restriction. Clinical management guidelines for obstetrician-gynecologists American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2001. 72:85–96.
15. Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008. 121:e223–e232.
16. Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatrics. 2004. 114:372–376.
17. McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol. 2008. 111:35–41.
18. Darcy AE. Complications of the late preterm infant. J Perinat Neonatal Nurs. 2009. 23:78–86.
19. Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R. The contribution of mild and moderate preterm birth to infant mortality. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. JAMA. 2000. 284:843–849.
20. Pulver LS, Guest-Warnick G, Stoddard GJ, Byington CL, Young PC. Weight for gestational age affects the mortality of late preterm infants. Pediatrics. 2009. 123:e1072–e1077.
21. Escobar GJ, Clark RH, Greene JD. Short-term outcomes of infants born at 35 and 36 weeks gestation: we need to ask more questions. Semin Perinatol. 2006. 30:28–33.
22. Swamy GK, Ostbye T, Skjaerven R. Association of preterm birth with long-term survival, reproduction, and next-generation preterm birth. JAMA. 2008. 299:1429–1436.
23. Loftin RW, Habli M, Snyder CC, Cormier CM, Lewis DF, Defranco EA. Late preterm birth. Rev Obstet Gynecol. 2010. 3:10–19.
24. Engle WA, Tomashek KM, Wallman C. Committee on Fetus and Newborn, American Academy of Pediatrics. "Late-preterm" infants: a population at risk. Pediatrics. 2007. 120:1390–1401.
25. Confidential Enquiry into Maternal and Child Health. Perinatal mortality surveillance 2004: England, Wales and Northern Ireland. 2006. London: CEMACH.
26. Khashu M, Narayanan M, Bhargava S, Osiovich H. Perinatal outcomes associated with preterm birth at 33 to 36 weeks' gestation: a population-based cohort study. Pediatrics. 2009. 123:109–113.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download