Laparoscopic approach is more advantageous over laparotomy, considering better cosmetic results, lesser blood loss, lesser pain and analgesic requirement, faster recovery, and shorter hospitalization time [1]. Laparoscopic approach to giant ovarian cyst, in cases when the cysts' sizes exceed to the umbilicus, may be difficult regarding the risk of cyst rupture and limited working space [2]. However, if the laparotomy is chosen as the operative treatment, a larger incision is required to excise the cyst. We present a case of laparoscopic extirpation of a giant ovarian cyst.
Case Report
A 26-year-old woman was referred to our department for a giant abdominal mass in July 2011. She was single and nulliparous female who presented with a gradually increasing abdominal swelling first noticed 4 years ago. Due to the huge mass she was unable to walk and had anorexia and weight gain. At admission, the emaciated patient weighted 120 kg, had a body height of 177 cm and abdominal girth at the level of the umbilicus was 190 cm (Fig. 1). There was no history of colicky pain fainting attacks, vomiting or other gastrointestinal attacks. She had no previous history of any illnesses, allergies or operations.
On abdominal examination, abdomen was grossly distended engorged veins present, fluid thrill was present. There were no abnormalities in hematologic and biochemical data including cancer biomarkers CA-125, CA 19-9, and carcinoembryonic antigen.
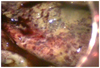
On ultrasonography, a huge, multilocular cystic tumor with low echogenic content was found (Fig. 2). There were no papillary or solid parts of associated with the wall or septa, and no ascites. She could not fit into the computed tomography machine due to the giant abdominal mass. After consultation with the anesthesiology and cardiology teams, the patient was placed in a semi-Fowler's position in the operating room due to dyspnea, general anesthesia and endotracheal tube intubation was performed. After induction of general endotracheal anesthesia, 10 mm trocar was inserted through the midline using a Hasson technique. Two additional 5 mm trocars were placed on the upper abdominal quadrants bilaterally. A 0° scope was placed through the midline port after 10 mm Hg pneumoperitoneum was established. On laparoscopic examination (Fig. 3), the omentum and the surfaces of the liver, stomach, and bowel were normal. The cyst was found to be slightly adherent to the abdominal cavity. There was no free fluid in the pouch of Douglas. A large cyst arising from the left ovary was found and left salpingo-oophorectomy was performed for the ovarian mass. The mass was removed piece by piece through the umbilical trocar, widening the incision up to 2 cm. The resected specimen weighted 3.8 kg and gross examination revealed a whitish tumor. The total weight of the cyst and its contents, including the fluid removed during surgery was 58 kg. Frozen section was suspicious for a mucinous cystadenoma, but diagnosis of borderline mucinous tumor was confirmed by histology (Fig. 4). During the surgery, the patient experienced no signs of hypotension and hypoxemia, with oxygen saturation more than 99%.
The postoperative course was uneventful. There were no complications, such as pneumonia, urinary tract infection, or surgical wound infection. The patient was discharged in a stable condition on postoperative day 16. Postoperative weight of the patient was 63.5 kg.
DISCUSSION
Giant ovarian cyst is rare finding. They have become rarer as imaging modalities improve and diagnoses are made earlier [3]. The largest ovarian tumor ever documented weighed 149 kg and was removed by Spohn [4] in 1905. The majority of the giant ovarian cysts which have been reported have had a mucinous histology. M⊠ucinous cystadenomas of the ovary are known for their potential to grow to massive proportions and are often incidentally diagnosed. They are typically benign tumors accounting for 15% of ovarian neoplasms and up to 80% of all mucinous tumors [5]. Ovarian mucinous cystadenomas are characteristically unilateral, only 5% presenting bilaterally, and occur principally in middle adult life and are extremely rare prior to menarche.
Increased intraabdominal pressure compromised cardiac and respiratory functions and caused supine hypotension secondary to compression of the inferior vena cava (IVC) and aorta. Supine hypotensive syndrome has been noted in pregnant women and patients with giant abdominal mass compressing the IVC to varying degrees [6]. Various clinical indicators were present, which helped identify the pathophysiologic process, including peripheral edema, dyspnea, orthopnea, decreased exercise tolerance, abdominal distension, hypotension, worsening oliguria. This syndrome is sometimes compensated for by homeostatic mechanisms, primarily appropriate intravascular volume status and sympathetic drive. Under general anesthesia, endogenous sympathetic activity is decreased, which may result in a symptomatic IVC syndrome and hypoxemia. In addition to giant abdominal cyst, positive pressure ventilation may likely contribute to the decreased venous return from chest and abdomen.
Management of giant intraabdominal cysts has traditionally required a full midline laparotomy [7]. Once the abdomen is entered and the large mass is isolated, the tumor can be resected. This can be accomplished by en bloc removal of the tumor, with or without controlled drainage of the tumor fluid. Removal of the tumor en bloc is thought by some to decrease the risk of spilling potentially malignant cells [8].
In recent years, with the minimal invasive approach becoming a widespread practice, laparoscopic excision is preferred in management of giant ovarian cyst that exceed to the umbilicus [9], but only few cases have been reported. Giant ovarian cysts that are exceeding to the umbilicus and filling the abdomen may limit the working space during laparoscopy. To establish enough working space, giant ovarian cysts can be drained before laparoscopic approach. Controlled drainage, while it may increase the risk of spillage, is thought to be a superior technique to improve exposure and prevent the phenomenon of supine hypotension syndrome [10]. In our case, the giant ovarian cyst was removed by salpingo-oophorectomy with laparoscopy after aspiration of intra-cystic fluid.
The most important potential hazard of drainage is the possibility of cell spillage into the abdominal cavity or drainage site with the potential for subsequent seeding [11]. Although several authors stated that giant ovarian cysts are usually benign, there have been reports of malignant tumors or tumors of low malignant potential [12]. The excision of giant ovarian cysts by laparotomy requires lager incision. Laparoscopic excision of giant ovarian cyst carries a risk of perforation during trocar insertion and intraabdominal spillage of the cyst content.
However, laparoscopic excision after drainage of giant ovarian cysts seems to be a safe and applicable treatment modality.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download