Abstract
Endometrial osseous metaplasia is a very rare disease related to secondary infertility. A 42-year-old woman, a North Korean defector, visited for gynecological exam. She presented with a history of secondary infertility. She had two previous pregnancies and both were voluntarily terminated at 14 and 16 years ago. Vaginal delivery at about 20 weeks in the first gestation 16 years ago; and dilatation and curettage at about 14 weeks 14 years ago were done in a medical facility of North Korea. Vaginal ultrasonography showed an intrauterine structure described as a hyperechogenic image suggesting calcification. Hysteroscopy revealed multiple coral-like white spicules about 1 cm in length in the uterine cavity. The lesion was treated by hysteroscopic removal without complications. Histology established the diagnosis of endometrial osseous. In our case, hysteroscopy was effective in the diagnosis and treatment of endometrial osseous metaplasia.
Osseous metaplasia is a very rare disorder of endometrium that usually leads to secondary infertility. Endometrial ossification is frequently associated with a history of recurrent abortions. Its clinical presentation may include vaginal bleeding or discharge, menometrorrhagia, dysmenorrhea, and pelvic pain [1].
Although the etiology of this rare condition is unknown, the most widely accepted hypothesis is that ossification is related to retained fetal bones, following abortion suggesting endochondral ossification. It also may be related to transformation of mesenchymal tissue to osseous tissue in response to inflammation and the reparative process induced by abortion. Some cases of endometrial ossification arise after abortion at an early age of gestation or even without abortion, suggesting a phenomenon of true heterotopias with metaplasia of mature endometrial stromal cells [2].
In this report, we present a patient with endometrial osseous metaplasia after previous termination of pregnancy. To our knowledge, this is the second case that the patient was successfully treated by hysteroscopic operation in Korea.
A 42-year-old woman, a North Korean defector, visited our hospital to take health gynecological screening. She fled from the North to South Korea a year ago. She had menarche at the age of 13 years followed by regular menstrual cycles. She had no history of endocrine abnormalities. Her obstetric history was notable for two pregnancies. Both of which were electively terminated in a medical facility of North Korea. Her first pregnancy was a vaginal delivery at about 20 weeks of gestation 16 years ago. Her second pregnancy showed dilatation and curettage at about 14 weeks of gestation 14 years ago. She has been infertile and failed to conceive since then. She had a regular menstrual cycle and had no menstrual disorders. She, however, presented with symptoms of intermittent vaginal discharge and chronic pelvic pain.
The pelvic examination revealed a normal size, anteverted uterus and normal adnexa. There was white colored leucorrhea, but no cervical motion tenderness. Laboratory studies included blood count, chemistry including serum calcium, and urine analysis, all of which were within the normal limits. Vaginal culture revealed infection of Mycoplasma hominis and Chlamydia trachomatis (Later she was treated with doxycycline and 3rd generation cephalosporin. The repeated culture demonstrated that there was no more infection).
On transvaginal ultrasound examination, about 2 cm sized highly echogenic and linear endometrial cavity was noted (Fig. 1). It appeared as an intrauterine device, but she denied any experience of having a procedure of intrauterine device insertion. We performed dilatation and curettage but failed to get the whole pathologic tissue except a piece of endometrial tissue. Computerized tomography showed amorphous high density lesion suggesting calcification in the uterus (Fig. 2).
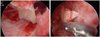
Diagnostic and operative hysteroscopy was performed under spinal block anesthesia. It revealed a wide endometrial cavity and proliferative endometrium with multiple coral-like white spicules, about 1 cm in length, on the internal wall of the uterus (Fig. 3). The lesion was completely removed using the grasping forcep under hysteroscopic control. There were no operative complications. Pathological examination showed endometrial tissue with osseous metaplasia in the stroma (Fig. 4).
Two weeks after the operation, a transvaginal ultrasound examination showed no abnormal ultrasound findings (Fig. 5). The patient resumed attempts to conceive spontaneously.
Osseous metaplasia results from the transformation of nonosseous connective tissue into mature bone. It is not applicable to the persistence of embryonic or fetal bone, resulting in calcification or ossification [1]. Osseous metaplasia is very rare, with about 100 cases described in reports. The incidence is estimated approximately 0.3 per 1,000 [3]. In 1884, Virchow attributed the formation of bone in the endometrium to spontaneous differentiation of fibroblasts into osteoblasts. Then, in 1923, Thaler linked the formation of this osseous metaplasia to a previous abortion [4]. It has been reported that the period of time between the abortion and diagnosis of osseous metaplasia can vary from 8 weeks to 23 years [2].
Although there are several theories that explain the etiology of osseous metaplasia of the endometrium, two main hypotheses have been advanced. One is spontaneous metaplastic transformation of the endometrial multipotential stromal cells (usually fibroblasts) into osteoblasts, and the other is the direct implantation of fetal parts persisting and growing as a homograft after incomplete abortion [2,5]. In the first theory, metaplastic transformation of stromal cell can occur in conditions of long-term endometrial estrogenic stimulation, chronic endometrial inflammation, or metabolic disorders such as hypercalcemia, hypervitaminosis D or hyperphosphatemia. In our case, the patient was found to have Mycoplasma and Chlamydia infection as well as history of abortions may stimulate formation of endometrial osseous metaplasia. Meanwhile, in the second theory, fetal tissues may lead to osteogenesis by three mechanisms. One possible mechanism is that retention of fetal bones secondarily promote osteogenesis in the surrounding endometrium. Fetal bones may supply a source of calcium for ossification [6]. Another mechanism is that implantation of embryonic parts without pre-existing bone after early stage abortions induces endometrial osseous metaplasia. There are a few cases in the literature of patients in whom abortion occurred in the very early gestational weeks, when no fetal bony tissue has been formed [7]. The other mechanism is that dystrophic calcification of retained and necrotic conceptual tissues causes chronic endometrial inflammation, which in turn may lead to secondary osseous metaplasia, as mentioned before [8]. The mechanism is thought to involve the stimulation of undifferentiated stromal mesenchymal cells to undergo metaplasia to an osseous type, via a superoxide radical superoxide dismutase system, which plays an important role in changes in cytokines, tumor necrosis factor, growth factors and extracellular matrix components. These factors may give rise to mature marrow [9]. For this reason, these two theories may not be clearly distinguishable. Thus, doubts have come up whether the osseous tissue results from fetus or patient. DNA analysis of the osseous tissue can be compared to determine its origin. Recently, Tulandi et al. reported on a case in which the osseous tissue was genetically stemmed from fetus [5]. On the contrary, Cayuela et al. [3] analyzed DNA and mentioned that the origin of osseous metaplasia is not a fetus, but a patient [2]. Nevertheless, it is sure that the most important risk factor for this unique pathology is the presence of recurrent abortions.
Secondary infertility is the most common symptom of endometrial osseous metaplasia, which may cause secondary infertility by assimilating intrauterine synechiae or an intrauterine device. It may prevent implantation of a blastocyst as a result of obliteration of the uterine cavity and it also may increase endometrial prostaglandins [8]. Other associated symptoms are pelvic pain, menometrorrhagia, dysmenorrhea, abnormal vaginal bleeding or discharge, and expulsion of bony particles from the vagina [7]. The diagnosis is suspected at ultrasonography and confirmed by hysteroscopy and histopathologic examination [10]. Ultrasonography may play a primary role in the diagnosis of osseous metaplasia. The hyperechogenic linear structures with acoustic shadowing filling the endometrial cavity, suggest of osseous tissue within the endometrial cavity of uterus. Most patients with osseous metaplasia also reported having sonographic appearance similar to that of an intrauterine device [7]. In our case, ultrasonography also showed appearance similar to an intrauterine device, but she denied of having intrauterine device insertion procedure; therefore, other diagnostic tools must be accompanied to confirm this disease. In some reports, hysterosalpingogram was used to diagnose this disease as bony spicules, which may create filling defects on hysterosalpingogram. However, its role has been reported having limitation on diagnose osseous metaplasia [7]. Meanwhile, hysteroscopy helps in the evaluation of the endometrial cavity and is accepted to be the gold standard for the diagnosis. Common hysteroscopic finding is a white meshwork of osseous tissue, arising from the uterine wall and extending perpendicularly into the uterine cavity. Fetal bones, such as skull, ribs, iliac bones, or long bones are found in rare cases [4]. Therefore, histological examination is essential for the definite diagnosis. Osseous metaplasia can be distinguished from fetal bone retention by the absence of surrounding tissue reaction and of enchondrial ossification microscopically [11].
Treatment can be accomplished with dilatation and curettage, operative hysteroscopy or hysterectomy. Dilatation and curettage initially has been used for both the diagnosis and treatment of osseous metaplasia in many previous cases. However, sometimes complete removal of tissue is not possible [9]. In our case, we were also unable to eliminate whole pathologic lesion in uterus by curettage. Nowadays, hysteroscopic or resectoscopic operation is preferred over dilatation and curettage for the removal of osseous tissue from the uterus. Especially, the ultrasound-guided hysteroscopy may be applied to facilitate removal of osseous tissue. Hysteroscopic excision, indeed, may be inadequate in patients with extensive osseous metaplasia such as the osseous tissue penetrating into the myometrium. Satisfactory hysteroscopic removal is very difficult; however, it has been reported that laparoscopic guided hysteroscopy was helpful to prevent complications such as uterine perforation [4]. Without any other causes of infertility, pregnancy and birth can occur when the osseous metaplasia of the endometrium is removed [2].
It has been suggested that the incidence of osseous metaplasia has been underestimated in the literature due to the prevalence of abortions is not low and the symptoms of this disease are nonspecific. Except for secondary infertility, our patient also had nonspecific complaints such as intermittent vaginal discharge or pelvic discomfort. In conclusion, endometrial osseous metaplasia should be considered in the diagnosis of secondary infertility, especially when the ultrasonography demonstrates calcification in the endometrial cavity. Moreover, patients with secondary infertility after an abortion should be evaluated by hysteroscopy when sonographic features are significant.
Figures and Tables
Fig. 2
Computerized tomography shows amorphous high density lesion suggesting calcification in the uterus.

References
1. Lainas T, Zorzovilis I, Petsas G, Alexopoulou E, Lainas G, Ioakimidis T. Osseous metaplasia: case report and review. Fertil Steril. 2004. 82:1433–1435.
2. Polat I, Sahin O, Yildirim G, Karaman E, Erim A, Tekirdag AI. Osseous metaplasia of the cervix and endometrium: a case of secondary infertility. Fertil Steril. 2011. 95:2434.e1-4.
3. Cayuela E, Perez-Medina T, Vilanova J, Alejo M, Cañadas P. True osseous metaplasia of the endometrium: the bone is not from a fetus. Fertil Steril. 2009. 91:1293.e1-4.
4. Rosa-E-Silva JC, Barcelos ID, Navarro PA, Rosa-E-Silva AC, Nogueira AA, Ferriani RA. Osseous metaplasia of the endometrium associated with infertility: a case report and review of the literature. J Med Case Rep. 2009. 3:7427.
5. Tulandi T, Al-Sunaidi M, Arseneau J, Tonin PN, Arcand SL. Calcified tissue of fetal origin in utero. Fertil Steril. 2008. 89:217–218.
6. Torné A, Jou P, Pagano R, Sanchez I, Ordi J, Vanrell JA. Endometrial ossification successfully treated by hysteroscopic resection. Eur J Obstet Gynecol Reprod Biol. 1996. 66:75–77.
7. Onderoglu LS, Yarali H, Gultekin M, Katlan D. Endometrial osseous metaplasia: an evolving cause of secondary infertility. Fertil Steril. 2008. 90:2013.e9-11.
8. Kumar S, Gupta P, Subbaiah M. Left behind: the patient's secondary infertility was traced to a previous pregnancy. Am J Obstet Gynecol. 2010. 202:319.e1-2.
9. Basu M, Mammen C, Owen E. Bony fragments in the uterus: an association with secondary subfertility. Ultrasound Obstet Gynecol. 2003. 22:402–406.
10. Coccia ME, Becattini C, Bracco GL, Scarselli G. Ultrasound-guided hysteroscopic management of endometrial osseous metaplasia. Ultrasound Obstet Gynecol. 1996. 8:134–136.
11. Bolaji II, Saridogan E, Hasan N, Baithun S, Djahanbakhch O. Prolonged retention of fetal bones with osseous metaplasia of the endometrium. Int J Gynaecol Obstet. 1995. 50:65–66.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download