Abstract
We present the case of a 42-year-old woman who had undergone laparoscopic hysterectomy for uterine myoma three years prior to diagnosis with trocar site endometriosis. The patient was observed to suffer endometrial implant exclusively at the suprapubic trocar site. This case demonstrated that trocar site endometriosis can occur, even in a patient without a uterus and without previous endometriosis. The etiopathogenesis of this condition was likely attributed to the dissemination of endometrial tissue during laparoscopic surgery, resulting in subsequent microscopic endometriosis cell implantation in the trocar site.
Endometriosis is a condition whereby functional endometrial tissue is present outside the uterine cavity. The disease commonly affects the pelvis with the most common locations being the ovaries, urine ligaments, rectovaginal septum and peritoneum. Unusual endometriosis outside the pelvis has been reported to include the bladder, intestines, appendix, hernia sacs, lungs, kidneys and other extremities. It well known that endometriosis may migrate and implant in various anatomic locations including surgical scars [1]. Herein, we report the rare case of a patient who had undergone a laparoscopic hysterectomy for uterine myoma three years prior to a diagnosis of trocar site endometriosis.
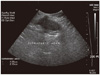
A 42 year old woman presented an approximately 3 cm sized mass in the suprapubic region at the site of trocar insertion, accompanied by cyclic pain which had commenced eight months prior to her visit. The patient had undergone two Cesarean sections, ten and twelve years prior to her visit, as well as a laparoscopic subtotal hysterectomy which was applied at a private clinic in order to treat a large uterine myoma three years prior to her visit. According to the private clinic, she did not report pelvic pain, dysmenorrhea or dyspareunia prior to the hysterectomy. And besides the uterine myoma, no other abnormal operative findings were observed during the hysterectomy. Our physical examination revealed an approximately 5 cm sized, non-tender mass, accompanied with slight swelling, located in the suprapubic region just beneath the suprapubic trocar site scar. Ultrasonography revealed a 5.5 × 2.2 cm, oval-shaped, hypoechoic mass in the abdominal wall of the suprapubic region. No abnormal findings were observed in the pelvis or ovaries (Fig. 1). Routine clinical laboratory test results were all within normal limits except for CA-125, which was slightly above normal range at 45.4 IU/mL. Based on these findings and symptoms, granulomas due to surgical wounds or endometriosis was suspected. Surgical exploration was conducted with the patient under general anesthesia. A sharp dissection was carried down to the palpable mass, which was firmly attached to the fascia. Intraoperatively, an approximately 5 cm sized hard mass was found between the subcutaneous tissue and the fascia. The mass was completely removed and the defect primarily closed. Histopathological examination revealed hyperplastic cicatic fibrosis with regions of scattered stromal tubular and cystic glandular endometrial tissues (Fig. 2). The patient's postoperative course was uneventful. She was treated with gonadotropin releasing hormone agonist with add-back therapy for 6 months with no resulting complications. Her serum CA-125 level returned to a normal range after one month. After 19 months, she reported no abdominal pain or other specific complaints.
Surgical scar endometriosis is a rare condition and is always iatrogenic. It can be observed after Cesarean section [2,3] and after episiotomy at the perineal site [4]. Surgical scar endometriosis at the trocar site has been described to be associated with the use of laparoscopic surgery as a method for treatment [5,6]. In our case, a symptomatic lesion was observed to develop three years after her laparoscopic hysterectomy, yet there was no endometriosis lesion noted at that time. As our knowledge, there is no case with scar endometriosis developed after hysterectomy for myoma such as our patient. This raises the question of how endometriosis implantation could occur three years after a laparoscopic hysterectomy in a patient without any previous evidence of an endometriotic lesion?
The etiopathogenetic mechanism by which endometriosis develops at a surgical wound site is evidently linked to endometrial tissue dissemination during the course of gynecological surgery. Subsequent to surgery, and under the stimulus of therapeutic estrogen, such tissues tend to grow until becoming symptomatic [1]. The influence of surgical tumor manipulation and the resultant shedding of tumor cells has been observed [7]. It has also been suggested that localized tissue ischemia renders that tissue conductive to implantation [6]. Several authors have hypothesized that the practice of insufflating CO2 into the peritoneal cavity causes cell aerosolization and may promote tumor cell shedding [5-8]. A higher probability of tumor growth on the peritoneum has been associated with gas laparoscopy as opposed to gasless laparoscopy procedures [7,8]. In the case of our patient, we suggest that microscopic endometriosis or otherwise undetected endometrial tissue, disseminated to the trocar site during laparoscopic surgery. Because microscopic endometriosis tissue or endometrial cell implantation likely occurred within the laparoscopy trocar site, secondary to manipulation or instrument interference, our case supports the hypothesis that the pneumoperitoneum influences the mechanism of free intraperitoneal cell implantation within the abdominal cavity.
In conclusion, endometriosis in the trocar site is not a common complication but may occur in a patient without a uterus due to hysterectomy, even in a patient without previous endometriosis. This can occur because microscopic endometriosis may implant at the trocar site during hysterectomy. In light of the fact that the use of the laparoscopic procedure in the treatment of numerous gynecological pelvic conditions is increasingly common, surgeons who perform laparoscopy must utilize procedural caution to protect the trocar site and surgical wound in order to prevent the dissemination of endometrial cells.
Figures and Tables
References
1. Koger KE, Shatney CH, Hodge K, McClenathan JH. Surgical scar endometrioma. Surg Gynecol Obstet. 1993. 177:243–246.
2. Firilas A, Soi A, Max M. Abdominal incision endometriomas. Am Surg. 1994. 60:259–261.
3. Luisi S, Gabbanini M, Sollazzi S, Calonaci F, Razzi S, Petraglia F. Surgical scar endometriosis after Cesarean section: a case report. Gynecol Endocrinol. 2006. 22:284–285.
4. Gordon PH, Schottler JL, Balcos EG, Goldberg SM. Perianal endometrioma: report of five cases. Dis Colon Rectum. 1976. 19:260–265.
5. Wakefield SE, Hellen EA. Endometrioma of the trocar site after laparoscopy. Eur J Surg. 1996. 162:523–524.
6. Martínez-Serna T, Stalter KD, Filipi CJ, Tomonaga T. An unusual case of endometrial trocar site implantation. Surg Endosc. 1998. 12:992–994.
7. Murthy SM, Goldschmidt RA, Rao LN, Ammirati M, Buchmann T, Scanlon EF. The influence of surgical trauma on experimental metastasis. Cancer. 1989. 64:2035–2044.
8. Hubens G, Pauwels M, Hubens A, Vermeulen P, Van Marck E, Eyskens E. The influence of a pneumoperitoneum on the peritoneal implantation of free intraperitoneal colon cancer cells. Surg Endosc. 1996. 10:809–812.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download