Abstract
Primary ovarian leiomyoma is a rare benign ovarian tumor. Ovarian leiomyoma accompanied with atypical Meigs' syndrome is extremely rare. A 13-year-old woman had underlying primary lymphedema and visited our clinic due to associated vulvar edema. During a gynecologic examination, we detected a right ovarian tumor with large amounts of ascites on transrectal ultrasonography. The tumor size increased from 4 to 7 cm during 6 months follow-up. After laparoscopic right ovarian tumorectomy, the final pathology of the tumor was primary ovarian leiomyoma. Ovarian leiomyomas are not typically suspected before surgery due to their extreme rarity and because they are easily misdiagnosed as fibroma during frozen biopsy due to similarities between both diseases. Here we introduce the case of a primary ovarian leiomyoma accompanied with atypical Meigs' syndrome.
Ovarian leiomyomas, either primary or parasitic in origin, account for about 0.5% to 1% of all benign ovarian tumors [1]. In previous reported cases, most ovarian leiomyomas were unilateral, asymptomatic, of relatively small size and occurred in premenopausal women. Primary ovarian leiomyomas originate from ovarian tissues, including intraovarian blood vessels, smooth muscle fibers, or similar tissues within the ovarian stroma and tunica albuginea [2,3]. In contrast, parasitic ovarian leiomyomas originate from extraovarian tissues [4]. Due to their rarity, about 70 cases of primary ovarian leiomyomas have been reported worldwide [1]. Primary ovarian leiomyoma with Meigs' syndrome is extreme rare case and previously reported only 4 cases [5]. The purpose of this report is to present a patient with a primary ovarian leiomyoma with atypical Meigs' syndrome.
A 13-year-old, para 0-0-0-0, virgin woman was referred to our clinic for evaluation of right vulvar edema. She had right leg edema due to underlying primary lymphedema and lymphaticovenular anastomosis and no improvement in leg edema. She complained of right vulvar area edema and was referred to our clinic due to the vulvar edema. We examined the external genitalia and detected right majora and minora edematous changes. Then, we performed routine transrectal ultrasonography. We detected a 4 cm ovarian tumor on transrectal sonography incidentally. She had no abdomino-pelvic discomfort and we decided to observe at regular intervals.
Six months later, the ovarian tumor had increased to about 7 cm and we decided to perform a laparoscopic operation. The sonographic images showed a 7.59 × 4.66 cm heterogeneous echogenic solid mass of the right ovary. The tumor was smooth mass with round contour and was suspected to be a benign solid tumor. We detected fairly large amounts of fluid collection in posterior cul de sac, but did not think abnormal fluid collections.
We performed abdomino-pelvic computed tomography (CT) preoperatively and the abdomino-pelvic CT showed an 8 cm enhancing solid mass with central low-attenuation from the right ovary. Poor delineation of the right margin of the mass was observed (Fig. 1). There were moderate amounts of ascites in pelvic cavity and it was thought as hemoperitoneum because of the high attenuation. And there were small amounts of omental infiltration which was considered as peritoneal seeding. Also there were multiple small lymph nodes along the mesenteric root. Finally, radiologist recommended differentiation of malignant germ cell tumor and juvenile granulosa cell tumor. In addition, subcutaneous soft tissue swelling on right side lower abdomen and pelvis was detected and was thought as involvement of lymphedema.
Laboratory findings such as complete blood cell count, urinalysis, chest X-ray and electrocardiography were normal. Because cliniLaboratory findings such as complete blood cell count, urinalysis, chest X-ray and electrocardiography were normal. Because clinician was not consider the ovarian tumor as malignancies, tumor markers were not checked.
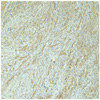
On laparoscopy, 5 cm sized solid tumors were observed and the tumors were surrounded by fragmented whitish tissues (Fig. 2). The tumor was sent to frozen biopsy and suspected to be a fibroma or leiomyoma arising from the ovary. The ovary mass looked like two divided masses: a round solid mass and surrounding whitish fragile tissues. The total size of the ovarian mass was about 5 cm. The vulvar mass looked like a mass arising vulvar subcutaneous layer and was suspected to be a lymphangioma, considering the patient's underlying primary lymphedema. The uterus and left ovary were grossly normal and bilateral tubes were in hydrosalpinxes. No adhesion between ovary and salpinx was seen. We only did a right ovary tumorectomy on laparoscopy considering the patient's age and further fertility. After a laparoscopic right ovary tumorectomy, we excised the right 4 cm vulvar mass which had been occured due to vulvar edema. The vulvar mass was easily removed without hematoma or other complications.
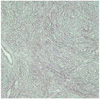
On microscopy, a round ovarian mass and surrounding whitish friable tissues were noted. Sections from the round solid mass revealed a tumor, composed of interlacing bundles of fusiform cells. Spindle-shaped cells had wavy nuclei and extensive hyalinization was seen in the tumor (Fig. 3A). On a high power view of the tumor, there was no significant nuclear atypia or pleomorphism (Fig. 3B). The fragile whitish mass was also compatible with leiomyoma. Immunohistochemically, the tumor cells were strongly positive for smooth muscle actin (SMA) (Fig. 4). The tumor cells were strongly positive for reticulin and the tumor was confirmed as leiomyoma (Fig. 5) [6-8].
The patient had normal postoperative care and was discharged 2 days postoperatively without any other complications.
A primary leiomyoma of the ovary is a very rare case and approximately 70 cases are reported in the literature since Sangalli first described this tumor in 1862. Even though the cases were reported that primary ovary leiomyoma occurred in postmenopausal women, most primary ovarian leiomyomas were reported in premenopausal women as seen in our case [2]. The size of primary ovarian leiomyoma was usually <3 cm, the size of the tumor was relatively large in our case.
Because of the rarity of the condition, primary ovarian leiomyomas are not diagnosed initially by ultrasonography or radiography. Ultrasound has been well documented as the best diagnostic modalities for pelvic organ masses, but in ovarian leiomyomas, it is difficult to distinguish ovarian leiomyomas from other ovarian tumors. Even on abdominopelvic CT, it is difficult to distinguish ovarian leiomyomas from other ovarian masses, and in some cases, the ovarian mass is reported as malignancy [8]. In addition, there were some cases misdiagnosed as an ovarian fibroma even though it will be revealed as an ovarian myoma on final pathology as our case showed.
Immunohistochemistry was stated to be useful in establishing the diagnosis in this case, since the results of frozen section was confusing between fibroma with leiomyoma. The diffuse positive staining for desmin and SMA are characteristic of a leiomyoma, whereas the negative staining for inhibin makes the diagnosis of a sex cord/stromal tumor unlikely. Because only focal stromal staining of SMA was observed in fibroma, we did reticulin immunohistochemistry staining for differentiation of leiomyoma and fibroma instead of inhibin staining [2].
We experienced an ovarian leiomyoma associated with ascites but not hydrothorax which is called Meigs' syndrome; an benign ovarian tumor associated with ascites and/or hydrothorax. Approximately 1% of benign ovarian tumors are associated with Meigs' syndrome. Atypical Meigs' syndrome is characterized by an ovarian tumor and ascites, but no pleural effusion, as in our case. Meigs' syndrome caused by ovarian leiomyoma is extremely rare. We found only one reported case in English and another in Japanese, which presented with both ascites and pleural effusion and two additional cases of ovarian leiomyoma presenting only ascites without pleural effusion as atypical Meigs' syndrome [5,9]. As a rule, resolution of ascites and pleural effusions occurs after removal of the ovarian lesion. We followed up the patient 6 months later and confirmed the resolution of ascites wirh on transrectal ultrasonograpy.
Concentrations of CA-125 can be raised in Meigs' syndrome [9]. Although the reason is unknown, benign solid ovarian tumors might secrete unknown factors that mediate the accumulation of fluid. Therefore preoperative diagnosis of the ovarian tumor was thought as ovarian malignancy in Meigs' syndrome and the surgical treatment can reach abdominal total hysterectomy plus bilateral salpingooophorectomy. We did not conduct the preoperative serum CA-125, because the clinician presumed that the ovarian tumor would be benign.
All cases of ovarian leiomyomas demonstrated an excellent prognosis without recurrence despite the active mitosis observed in the tumor [6]. Therefore the surgeon should make an effort to perform less invasive surgery, particularly in young women, to preserve fertility [10].
In conclusion, it is difficult to diagnose ovarian leiomyomas accurately due to their rarity and diagnostic difficulties. However, because primary ovarian leiomyomas occur in young women, the nature of the tumor is typically benign, prognosis is excellent and recurrence is rare, surgeons should consider ovary-preserving surgery as a first choice in surgical management.
Figures and Tables
Fig. 1
Poor delineation of the right ovarian mass measuring about 8cm
in length on computed tomography.

Fig. 2
Gross picture of 5cm sized solid tumors originating from right ovary. The ovarian tumor and the surrounding whitish fragile tissues are separated from right tube and is limited to the right ovary.
Fig. 3
(A) Spindle-shaped cells with wavy nuclei and extensive hyalinization was seen in the right ovarian tumor (H&E, ×100). (B) On the high powered magnititude, no significant nuclear atypia or pleomorphism was seen (H&E, ×200).

References
1. van Esch EM, van Wijngaarden SE, Schaafsma HE, Smeets MJ, Rhemrev JP. The diagnostic and therapeutic approach of a primary bilateral leiomyoma of the ovaries: a case report and a literature review. Arch Gynecol Obstet. 2011. 283:1369–1371.
2. Güney M, Ozsoy M, Oral B, Mungan T, Kapucuoğlu N. Unilateral primary ovarian leiomyoma in adolescent: a case report. Arch Gynecol Obstet. 2007. 275:507–510.
3. Koo YJ, Cho YJ, Kim JY, Lee JE, Kim ML, Kim JM, et al. Ovarian leiomyoma as a potential cause of compromised fertility. Fertil Steril. 2011. 95:1120.
4. Abdel-Gadir A, Francis ND, Oyawoye OO, Chander BP. Secondary amenorrhoea with high inhibin B level caused by parasitic ovarian leiomyoma. Gynecol Endocrinol. 2010. 26:93–95.
5. Kurai M, Shiozawa T, Noguchi H, Konishi I. Leiomyoma of the ovary presenting with Meigs' syndrome. J Obstet Gynaecol Res. 2005. 31:257–262.
6. Bucella D, Limbosch JF, Buxant F, Simon P, Fayt I, Anaf V, et al. Recurrence of mitotically active cellular fibroma of the ovary. Obstet Gynecol Int. 2009. 2009:803062.
7. Tomas D, Lenicek T, Tuckar N, Puljiz Z, Ledinsky M, Kruslin B. Primary ovarian leiomyoma associated with endometriotic cyst presenting with symptoms of acute appendicitis: a case report. Diagn Pathol. 2009. 4:25.
8. Paladini D, Testa A, Van Holsbeke C, Mancari R, Timmerman D, Valentin L. Imaging in gynecological disease (5): clinical and ultrasound characteristics in fibroma and fibrothecoma of the ovary. Ultrasound Obstet Gynecol. 2009. 34:188–195.
9. Shiau CS, Chang MY, Hsieh CC, Hsieh TT, Chiang CH. Meigs' syndrome in a young woman with a normal serum CA-125 level. Chang Gung Med J. 2005. 28:587–591.
10. Son CE, Choi JS, Lee JH, Jeon SW, Hong JH, Bae JW. Laparoscopic surgical management and clinical characteristics of ovarian fibromas. JSLS. 2011. 15:16–20.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download