Abstract
A 17-year-old woman, who was hospitalized because of pelvic inflammatory disease due to Chlamydia trachomatis, developed emesis on 5th hospital day. On 7th day, vomiting and abdominal pain was aggravated. Plain radiography and contrast enhanced abdominopelvic computed tomography (CT) scan revealed small bowel obstruction with possible ischemic change at the level of the mid to distal ileum. Emergent exploratory laparotomy wad done and revealed adhesive band between small bowel mesentery and omentum, which resulted in closed loop and small bowel obstruction. Partial omentectomy, adhesive band adhesiolysis and incidental appendectomy was done. After surgery, the symptom was completely resolved with no further recurrence after outpatient department follow-up for 11 months. The present case calls for inclusion of abdominopelvic CT scan as well as plain radiography of the abdomen in the evaluation of pelvic inflammatory disease (PID) associated with emesis to detect bowel obstruction, rare sequlela of PID.
Figures and Tables
Fig. 1
Plain abdominal radiography. Upright (A) and supine (B) abdominal radiographs showed focal ileus in right upper quadrant and pelvic cavity and there is no small bowel dilatation and normal transverse colon gas shadow is seen on day 1 of hospitalization, whereas on day 7 upright (C) abdominal radiograph shows multiple air-fluid level (arrows) in small bowel and supine (D) abdominal radiograph showed dilated small bowel with no gas seen in colon that it meaned developing small bowel obstruction.

Fig. 2
Contrast-enhanced computed tomography (CT) scan. Axial (A) and sagittal (B) CT scan show no evidence of dilated small bowel on day 1 of hospitalization, whereas on day 7 axial (C) and sagittal (D) CT scan show dilated, fluid-filled small bowel to the level of an adhesion in the ileum and note the collapsed segment of bowel (arrows) that it meaned transition zone.
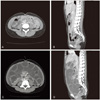
Fig. 3
The omentum shows multifocal abscess formation mixed with blood, fibrinous exudates (H&E, ×200) (A), areas of lymphoplasmacytic infiltration (H&E, ×400) (B), and the appendix shows lymphoplasmacytic infiltration predominantly along the subserosal layer (H&E, ×40) (C) H&E, ×400 (D).

Table 1
Cases of small bowel obstruction with pelvic inflammatory disease due to Chlamydia trachomatis

MIF, microimmunofluorescence; ELISA, enzyme-linked immunosorbent assay; N/A, not available (not described); PID, pelvic inflammatory disease; SBO, small bowel obstruction; RUQ, right upper quadrant; RLQ, right lower quadrant; LCR, liquid chain reaction; CT, computed tomography; PCR, polymerase chain reaction.
References
1. Lee JW, Cho HC, Choi KY, Bae DH, Kim HJ. Application of nested pcr for the detection of chlamydia trachomatis in diagnosis and monitoring the patients with pelvic inflammatory disease and vaginitis. J Soonchunhyang Med Coll. 2001. 7:301–305.
2. Bolton JP, Darougar S. Perihepatitis. Br Med Bull. 1983. 39:159–162.
3. Eschenbach D. Danforth DN, Scott JR, editors. Pelvic infections and sexually transmitted diseases. Danforth's obstetrics and gynecology. 1999. 8th ed. Philadelphia (PA): Lippincott Williams & Wilkins;594–595.
4. Harel Z, Tracy TF Jr, Bussey JG 3rd. Small bowel obstruction in an adolescent with pelvic inflammatory disease due to Chlamydia trachomatis. J Pediatr Adolesc Gynecol. 2003. 16:125–128.
5. Burton E, McKeating J, Stahlfeld K. Laparoscopic management of a small bowel obstruction of unknown cause. JSLS. 2008. 12:299–302.
6. Abul-Khoudoud OR, Khabbaz AY, Butcher CH, Farha MJ. Mechanical partial small bowel obstruction in a patient with Fitz-Hugh-Curtis syndrome. J Laparoendosc Adv Surg Tech A. 2001. 11:111–114.
7. Harris C, Lambrianides AL. Small bowel obstruction secondary to pelvic inflammatory disease. Am Surg. 2011. 77:E80–E81.
8. Pegg DJ, Owen AW. Gastrointestinal obstruction associated with Chlamydia trachomatis. Genitourin Med. 1990. 66:26–27.
9. De K, Essex-Cater AJ. Gastrointestinal obstruction associated with Chlamydia trachomatis. Genitourin Med. 1990. 66:408.
10. Baumgardner DJ, McCanse DE. Peritonitis and small bowel obstruction. IMJ Ill Med J. 1987. 171:75–78.
11. Oh SN, Rha SE, Byun JY, Kim JY, Song KY, Park CH. Chilaiditi syndrome caused by Fitz-Hugh-Curtis syndrome: multidetector CT findings. Abdom Imaging. 2006. 31:45–47.
12. Kim JO, Yun IY, Chung DY, Jo BC, Song SK. A clinical evaluation of chlamydia trachomatis infection in women. Korean J Obstet Gynecol. 2002. 45:1827–1834.
13. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010. 59:1–110.
14. Cook RL, Hutchison SL, Østergaard L, Braithwaite RS, Ness RB. Systematic review: noninvasive testing for Chlamydia trachomatis and Neisseria gonorrhoeae. Ann Intern Med. 2005. 142:914–925.
15. Delabrousse E, Lubrano J, Jehl J, Morati P, Rouget C, Mantion GA, et al. Small-bowel obstruction from adhesive bands and matted adhesions: CT differentiation. AJR Am J Roentgenol. 2009. 192:693–697.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download