Abstract
Cesarean scar pregnancy is the one of the rarest forms of ectopic pregnancy and is associated with severe complications, such as uncontrollable bleeding and uterine rupture. However optimal treatment has not been established. We present here a case of ectopic pregnancy in the previous Cesarean scar treated successfully by uterine artery embolization in combination with subsequent intra-cardiac potassium chloride and intra-sac methotrexate injection without surgical or invasive intervention at 9+3 weeks' gestational age.
Cesarean scar pregnancy is a rare form of ectopic pregnancy implanted in the myometrium at the site of a previous Cesarean section scar [1,2]. These conditions are challenging to diagnose and have higher risk of bleeding and uterine rupture [3,4]. Due to the severity of complications and possibility of hysterectomy, early diagnosis is critical [5]. However, there is still no standard treatment modality. We report here a case of viable Cesarean scar pregnancy successfully treated with uterine artery embolization followed by local injection of potassium chloride (KCl) and methotrexate (MTX) under sonographic guidance at 9+3 weeks' gestational age which was advanced compared with those of previous reported cases.
in Seoul National University Hospital for suspected Cesarean scar pregnancy. She had been naturally pregnant and underwent Cesarean delivery due to placenta previa on 2004. The next pregnancy was on December, 2006. But she was diagnosed with hydatidiform mole and treated with curettage and systemic methotrexate injection. After 1 year of treatment and follow-up, she was diagnosed with a cure. After that, she was failed to get pregnant during 2 years and underwent infertility examination. On hysterosalpingogram, right hydrosalpinx was noted and pelviscopic right salpingectomy was done on 2009.
She underwent 3 times of in vitro fertilization cycle which were all failed. And then, she got taken thawing embryo transfer on 5, November, 2010 and conceived successfully. The β-subunit of serum human chorionic gonadotropin (β-hCG) values had been elevated as in normal pregnancy, and there were no signs or symptoms of an ectopic pregnancy. At eight weeks' gestational age, the gestational sac was noted to be located into the previous Cesarean scar with normal fetal heart beat and appropriate crown-rump length.
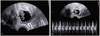
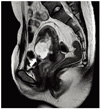
On December 17, she was referred to our hospital. The levels of serum hemoglobin and β-hCG were 13.3 g/dL and 152,760 mIU/mL, respectively. Transvaginal ultrasound showed thinning of uterine myometrium which was estimated about 3.3 mm on the axial view (Fig. 1A). Well-defined gestational sac contained a fetal pole with normal heart beat (Fig. 1B). Crown lump length was checked about 1.94 cm which was appropriate for 8+4 weeks' gestation. The images of pelvis magnetic resonance imaging (MRI) showed the gestational sac embedded in the anterior lower uterus (Fig. 2). And we decided to terminate the pregnancy after counseling with the patient.
On December 23 (at 9+3 weeks' gestation), she was admitted. Before medical treatment, bilateral uterine artery embolization was done for reducing the risk of hemorrhage. And then, under transvaginal ultrasound guidance, a 17-gauge needle was introduced into the gestational sac. An intra-cardiac injection of 0.6 mL (1.2 mEq) of potassium chloride was given to the fetus followed by aspiration of sac contents and intra-sac injection of 50 mg methotrexate. After procedure, no fetal heart beat was noted on ultrasonography. Repeat transvaginal ultrasound done on the forth post-treatment day showed an about 3.1×1.3 cm sized distorted gestational sac and absence of fetal heart activity. Serum β-hCG declined to a level of 28,630 mIU/ml on the first post-treatment day and 4,263 mIU/ml on the third day. The patient was discharged without complication. Seventeen days after treatment, the serum level of β-hCG was checked within normal range and there was no remnant gestational material in endometrial cavity on transvaginal ultrasonography.
Implantation of a pregnancy within a Cesarean fibrous tissue scar is considered to be the rarest form of ectopic pregnancy and constitutes a life-threatening condition [1]. A recent case series estimates that the incidence of Cesarean scar pregnancy was 1:2216 of all pregnancies [6]. The exact cause and mechanism is not well understood. Although many hypotheses have been proposed to account for this rare condition, the most reasonable seems to be that the conceptus enters into the myometrium through a microscopic dehiscent tract generated between the prior Cesarean scar and the endometrial canal [3].
Diagnosis is usually made by ultrasound sonographic examination, but laparoscopy [7], hysteroscopy [4] or even magnetic resonance imaging [3] can also be helpful. Ultrasound imaging criterias to diagnose Cesarean scar pregnancy are as follows: 1) the trophoblast must be mainly located between the bladder and the anterior uterine wall; 2) no fetal parts must be visible in the uterine cavity; and 3) on a sagittal view of the uterus running though the amniotic sac, a discontinuity in the anterior wall of the uterus should be demonstrated [8]. In this case, we had a difficulty in distinction between previous Cesarean scar pregnancy and a lowly implanted intrauterine pregnancy on ultrasound. The images of pelvis MRI were a great help to confirm the diagnosis.
With limited experience of Cesarean scar pregnancies, it is difficult to decide on optimal management in individual cases [9]. The choice of management includes transvaginal surgical evacuation, laparoscopic removal, laparotomy, medical treatment with local injection of methotrexate or embryocides and expectancy [4,6,10]. We chose the medical treatment with local injection of potassium chloride and methotrexate rather than surgical treatment. Jurkovic et al. [11] recommended this combination therapy in cases with detectable embryonic cardiac activity. This case had a high risk of the complication such as uterine bleeding due to high initial β-hCG level and advanced fetal gestational age. Therefore, the patient underwent uterine artery embolization before the medical treatment. In addition, we expected that the bleeding risk after secondary procedure, such as uterine curettage, would be reduced by embolization. The efficacy of uterine artery embolization before the management of Cesarean scar pregnancy was already reported in previous studies [5,12]. Sugawara et al. [5] reported a case of scar pregnancy treated with selective transarterial embolization in combination with subsequent dilatation and curettage and local or systemic injections of MTX. Recently, Seok et al. [13] reported a case which was treated with uterine artery embolization at 13 weeks of gestation.
The combination therapy of uterine artery embolization, local injection of potassium chloride and methotrexate had not been reported and firstly tried in our case. It took seventeen days until the gestational material was disappeared and serum β-hCG was normalized. And there was no complication and no need of further management. In conclusion, the combination therapy of artery embolization and subsequent intra-cardiac KCl and intra-sac MTX injection can be considered as a first line treatment in the cases of viable Cesarean scar pregnancy.
Figures and Tables
References
1. Fylstra DL. Ectopic pregnancy within a cesarean scar: a review. Obstet Gynecol Surv. 2002. 57:537–543.
2. Ash A, Smith A, Maxwell D. Caesarean scar pregnancy. BJOG. 2007. 114:253–263.
3. Godin PA, Bassil S, Donnez J. An ectopic pregnancy developing in a previous caesarian section scar. Fertil Steril. 1997. 67:398–400.
4. Lee CL, Wang CJ, Chao A, Yen CF, Soong YK. Laparoscopic management of an ectopic pregnancy in a previous Caesarean section scar. Hum Reprod. 1999. 14:1234–1236.
5. Sugawara J, Senoo M, Chisaka H, Yaegashi N, Okamura K. Successful conservative treatment of a cesarean scar pregnancy with uterine artery embolization. Tohoku J Exp Med. 2005. 206:261–265.
6. Seow KM, Huang LW, Lin YH, Lin MY, Tsai YL, Hwang JL. Cesarean scar pregnancy: issues in management. Ultrasound Obstet Gynecol. 2004. 23:247–253.
7. Roberts H, Kohlenber C, Lanzarone V, Murray H. Ectopic pregnancy in lower segment uterine scar. Aust N Z J Obstet Gynaecol. 1998. 38:114–116.
8. Vial Y, Petignat P, Hohlfeld P. Pregnancy in a cesarean scar. Ultrasound Obstet Gynecol. 2000. 16:592–593.
9. Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R, Elson CJ. Cesarean scar pregnancy. Ultrasound Obstet Gynecol. 2003. 21:310.
10. Maymon R, Halperin R, Mendlovic S, Schneider D, Vaknin Z, Herman A, et al. Ectopic pregnancies in Caesarean section scars: the 8 year experience of one medical centre. Hum Reprod. 2004. 19:278–284.
11. Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R, Elson CJ. First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 2003. 21:220–227.
12. Ghezzi F, Lagana D, Franchi M, Fugazzola C, Bolis P. Conservative treatment by chemotherapy and uterine arteries embolization of a cesarean scar pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002. 103:88–91.
13. Seok JM, Moon MJ, Chang SW, Lee YM, Jang JH, Baek MJ. Successful management of cesarean scar pregnancy at 13 weeks of gestation by uterine artery embolization: a case re port. Korean J Obstet Gynecol. 2010. 53:934–939.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download