A sclerosing stromal tumor (SST) of the ovary is an extremely rare sex cord-stromal tumor. This tumor occurs predominantly in young females at an average age of 27 to 28 years old [1]. Since it was first described by Chavarjian and Scully in 1973, fewer than 100 cases have been described in the literature [2]. Moreover, a few cases of SST in pregnant women have been described [3-5].
SST should be distinguished from malignant tumors, but it is difficult to diagnose before surgery by imaging studies. It used to be diagnosed by pathological examination during surgery or after surgery. We report the ultrasonographic and histological findings of a SST of the right ovary during pregnancy with review of the literature.
Case Report
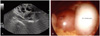
A 26-year-old woman presented to the hospital with nausea and amenorrhea that was reported to have started about 3 weeks ago. The patient did not have regular cytologic smears and pelvic ultrasonographic examination. Transvaginal ultrasound showed a single fetus was present in the uterine cavity and the size was 8th week. A 6.5 × 5.3 cm mass was demonstrated, lateral and posterior to the uterus, and was homogeneously hypoechoic (Fig. 1A). Power Doppler gave slow low-flow vascular signals. Also, the serum CA-125 level was high (96.72 UI/mL). There was no unusual symptoms such as pelvic pain, hypermenorrhea, and menstrual irregularities, due to SST.
When 10 weeks of gestation, surgery was performed because the pregnant women worried about tumor effects on the fetus. A right oophorectomy was performed. Under general anaesthesia, laparoscopy showed a normal uterus and left ovary with the right ovary replaced by a solid mass. On gross inspection, the removed right ovarian mass measured 7 × 5 × 6 cm and weighed 154 g. The mass was gray-white in color and had a smooth and well-encapsulated surface (Fig. 1B). The cut surface was a focally pale yellow solid and cystic fragment. The frozen section was not performed because pathology is not here. In microscopic findings there was an irregularly mixed pattern with hypercellularity and hypocellularity areas. Hypercellularity areas showed a pseudolobular structure, whereas hypocellularity areas showed an edematous structure (Fig. 2A). Hypocellularity and hypercellularity areas were divided by a hyalinized connective tissue. Many blood vessels were distributed in the boundary region. Polyhedral and spindle-shaped cells were mixed in the hypercellularity areas (Fig. 2B). The pathological diagnosis was SST of the right ovary. After surgery, the CA-125 level returned to normal. Pregnancy has been well maintained without any problems.
Discussion
Sclerosing stromal tumor is a rare benign ovarian tumor originating from granulosa-stromal cell tumor group. SST occurs most frequently in young females (average age at diagnosis 27, to 28 years) [6] and the most common signs and symptoms are a palpable pelvic mass, metrorrhagia, menstural irregularity, and pelvic pain. The histopathology of the SST shows a pseudolobular pattern of cellular areas and hypocellular, edematous or collagenous areas. It has a prominent vasculature and prominent sclerosis around clusters of individual cells as well as cellular heterogeneity of the vacuolated luteinized theca-like cells and spindle shaped fibroblast-like cells in the cellular areas [7]. Immunohistochemically, the cells of SSTs are positive for vimentin, smooth muscle actin, α-inhibin, and CD99; and are negative for S-100 protein and epithelial markers [2]. In early pregnancy, the most common masses are corpus luteum cysts, whereas after the first trimester, benign cystic teratomas and cystadenomas are more frequently observed. Surgery is in most cases performed during pregnancy, since 2% to 5% of lesions are malignant, and large benign masses can cause complications during delivery [8]. In the evaluation of a pelvic mass during pregnancy computed tomography should be avoided because of the radiation dose. It may also have a detrimental effect on fetal development in the first trimester. Ultrasonography (US) is useful for distinguishing between cystic and solid masses [9], but can be undetermined in lesion characterization, such that a differential diagnosis from malignant ovarian neoplasms is not always possible [10].
US and computed tomography (CT) findings of SST show an increased peripheral vascular as seen in malignant tumors. Since peripheral is a thick layer with a remarkable proliferation of blood vessels, the stromal is the representing form of lobulation by local edema.
SST can not predict its presence preoperatively on the basis of clinical and ultrasonographic findings alone. Magnetic resonance imaging (MRI) is the technique of choice in the characterization and preoperative assessment of pelvic masses during pregnancy. MRI findings include typical signal patterns such as hypointense nodules, hyperintense stroma, lobulation, strong enhancement with gadolinium and a peripheral hypointense rim are present [11]. Sclerosing stromal tumors were reported in which the inactive tumors did not represent endocrine clinical symptoms [7]. However, currently according to several reports, it is the active tumor that produce hormones [12-14]. A few case of SST in pregnant women have been described about virilization. In this case, neither hormonal activity nor virilization was observed.
Treatment of SST is sufficient only for oophorectomy because these are benign tumors. By considering the impact on pregnancy, progesterone 100 mg was taken vaginally until 12 weeks of gestation. SST is a very rare tumor but tumor markers, hormone tests and US, in addition to MRI should be performed when the women are under the age of 30 and the visual inspection reveals 5 cm or more of a solid tumor. Frozen biopsies should also be performed during surgery. We report a case of SST in a 26-year-old woman who was admitted to confirm pregnancy with a review of the literature.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download