Abstract
Periventricular leukomalacia is a disorder of white matter injury that is frequently found in premature infants and is the major cause of cerebral palsy. However, only a few cases of periventricular leukomalacia have been reported prenatally. Ultrasound investigation of the periventricular region could provide clues for the prenatal diagnosis and prediction of cerebral palsy. Herein, we report a case of cystic periventricular leukomalacia that was diagnosed prenatally and confirmed postnatally by brain magnetic resonance imaging.
Periventricular leukomalacia (PVL) is a typical cerebral lesion in premature infants, largely due to hypoxia-ischemia and reperfusion, which may result in cerebral palsy (CP) [1]. The pattern of perinatal brain injury is age-dependent, which in turn results in prognoses of different pathways. Depending on the type of lesion, the suspected incidental time may vary. PVL can be suspected on routine ultrasound screening. Periventricular echodensities (PVE), echolucent cysts, or ventricular dilatations are some of the abnormal prenatal ultrasonographic findings suggestive of PVL, which lead to a neurosonography and follow-up throughout the rest of the perinatal period.
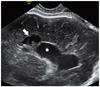
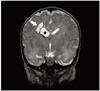
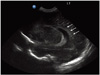
A 27-year-old, para 1 woman was referred for consultation due to the findings of a mildly dilated lateral ventricle in the fetus at 34 + 6 weeks of gestation. She had no past medical history, no operation history, and had not taken any kind of medication, except for oral iron for the current pregnancy. Her family did not have any history of medical illnesses, and she did not smoke nor drink. She had one full-term vaginal delivery two years prior. At the beginning of the current pregnancy, the patient did not have any obstetrical problems. Mid-gestation screening was reported low risk. Mild ventricle dilatation in the fetus was detected on the 2nd trimester ultrasound examination and was maintained until 35 weeks of gestation. Therefore, she was referred to our hospital at 34 + 6 weeks of gestation due to mild but persistent fetal ventriculomegaly. The biometry showed normal measures for head circumference, femur length, abdominal circumference, and estimated fetal weight. A closer look at the brain revealed the width of the lateral ventricle to be 9.8 mm. Cystic changes in the right frontal periventricular region were detected, along with a prominent lateral ventricle (Fig. 1). At 36 +5 weeks of gestation, the mother visited the delivery floor complaining of watery vaginal discharge. At 36 + 6 weeks of gestation, a baby girl, 3,150 g, was born by normal vaginal delivery, with an Apgar score of 9 at 1 minute and 9 at 5 minutes. The infant looked healthy without spasm. No hypotonia and spasticity were detected on physical examination done by a pediatric neurologist. On the second day, brain magnetic resonance imaging (MRI) showed grade 3 PVL with a mildly dilated right lateral ventricle with cystic encephalomalacia near the right lateral ventricle (Fig. 2) and focal chronic old hemorrhage in the inferolateral wall of the right lateral ventricle body. The brain ultrasound revealed grade 2 PVL in the right lateral ventricle and grade 1 PVL in the left lateral ventricles, with periventricular cysts and echogenicities (Fig. 3), respectively. Despite the severity of the findings, the patient had no severe neurologic complications. The baby was well and discharged at 4 days of age, and outpatient department follow-ups have included physical therapy for hypotonicity and weak upper extremities that have developed over the postnatal months.
PVL is a cerebral injury that is mainly prevalent in preterm infants but also arises in full-term neonates as well as infants as old as two months postnatally [1]. It is known to be a leading cause of CP in newborns. It is a disorder of diffuse white matter injury characteristic of focal cystic necrotic lesions to diffuse myelination disturbances [2]. The main pathogenesis of this disease is thought to be due to hypoxic-ischemia and maternal-fetal infection. The vasculature of the premature infant has not yet matured, and the walls of the arteries and veins are still fragile and thin. During episodes of decreased oxygenation, it is likely that these vessels are not able to maintain a sufficient amount of blood flow, which in turn results in hypoxic-ischemic events [3]. Therefore, incomplete development of the peripheral cerebral arteries and impaired tissue perfusion in periventricular white matter result in white matter damage, which is PVL. The damage may show as a diffuse lesion or as cystic, focal lesions. Another mechanism is infection-inflammation, which seems to be an important risk factor for brain injury, especially in term infants. Other risk factors for neonatal PVL mentioned in the literature are premature rupture of membrane, preterm birth, multiple pregnancy, intrauterine growth retardation, reduced amniotic fluid, cord compression, and low Apgar scores [4,5]. The fetal brain has restorative powers, in which intrauterine damage to the brain can be a brief incident where regrowth of the brain tissue occurs; consequently, the neonatal outcome would be normal, and PVE would disappear. The repairing function is thought to be due to a significant increase in insulin-like growth factor 1 (IGF-1) of maternal origin in maternal and cord sera in late gestation, which is supposed to play an essential role in fetal growth. After birth, the newborn is separated from the mother, and the IGF-1 is lost in the neonatal circulation, diminishing regrowth abilities. The PVE repairing function is diminished in the neonatal brain, necrotic changes progress to develop a cyst in PVE, and PVL is formed [6]. Early changes associated with cystic PVL may be apparent histologically within hours of insult, but at least 2 to 6 weeks are required before lesions can be visualized on the sonogram. Therefore, if cystic PVL is observed within 7 days after birth, the origins must be intrauterine [7]. Another big risk factor of term PVL, clinical chorioamnionitis, is strongly connected to CP, as the infectious products sensitize the fetus to secondary insults [8]. A study has suggested that maternal infection can activate the cytokine network, causing interleukin-6 levels to rise, which were found in high levels in the umbilical cord blood of neonates with white matter lesions [9].
Depending on the findings of the ultrasound, PVL is graded into four findings: grade 1 correlates with findings of increased PVE at the external angle of the lateral ventricle, corresponding to the early stages of PVL. Grade 2 is when small cysts develop 2 to 3 weeks after the onset of PVE in the same area as grade 1. Grade 3 shows PVE extending to the parieto-occipital white matter, breaking down into cystic lesions 2 to 4 weeks later. With grades 2 and 3, cysts are usually no longer visible when the infant is 2 to 3 months old. Owing to loss of brain tissue, dilation of the ventricles develops, either uni- or bilateral, as predicted by the early localization of the lesions. Grade 4 mainly affects full-term infants and is often called subcortical leukomalacia. Localization of PVE and cysts is farther away from the lateral ventricles than in premature infants, and the cysts do not resolve [10]. The baby in this case has findings consistent with grades 2 and 3 in the right lateral ventricle and grade 1 in the left lateral ventricle. Identifying PVL during a pregnancy can be difficult, and depending on the type of lesion, PVL of the diffuse, echodense type could be missed if not examined closely with caution. Usually it is diagnosed during a routine sonogram, and depending on whether the lesion is cystic or atrophic, the suspected incidental time may be very early in pregnancy or as late as 32 to 35 weeks of gestation. The baby in this case was diagnosed with cystic PVL with periventricular echogenic shadows or echodensities. A study by Yamamoto et al. [4] states that there is a relationship between the gestational age at delivery and the persistence of fetal PVE, which eventually leads to neonatal PVL. White matter damage causes accumulation of astroglia, which may cause high echogenicity on ultrasound examination. Motor nerve conduction is disconnected by the cystic change of the white matter, after which CP appears as a result. PVE may be a precedent to PVL locally, showing hypoxic-ischemia before motor nerve fiber necrosis occurs. In another study that aimed to find out the relationship between the grade and duration of PVE and its subsequent development of CP, the result was that no matter what the gestational age, the longer the duration of PVE, the worse the CP. However, the authors could not find a correlation between grade of PVE and adverse neurodevelopmental outcome [11]. As for the present case, the baby was evaluated by a pediatrician and a rheumatologist one month post birth. She showed overall hypotonicity and weakness in the upper extremities, especially the axilla. Development of motor movement and muscle control was lagging, so physical therapy was started. It has been a year now, and so far therapy has helped the baby recover some of her muscle strength. There have been no occurrences of spasticity, especially in the lower extremities. However, periodic follow-up investigation is mandatory to find a correlation between the grade and duration of PVE and the possible development of CP.
Cerebral palsy is one of the most prevalent conditions associated with obstetric malpractice litigation, and PVL is a major cause of CP. For this reason, precise prenatal diagnosis of PVL and proper counseling about the prognosis are essential. Periventricular cyst and ventricle dilatation with prolonged PVE increase the risk of CP. When performing the prenatal sonogram, caution must be taken, especially when the baby is full term with risk factors, in which case a detailed examination of the periventricular area would be indispensible. This case suggests the importance of the meticulous surveillance of the fetus with prenatal sonographic features of suspected brain lesions. Close investigation and follow-up of a PVL fetus would prepare us for increasing medical litigations and pre- and postnatal counseling, including possible early treatment.
Figures and Tables
Fig. 1
Prenatal sonogram: Enlarged right lateral ventricle (white star) with periventricular cystic changes (white arrow).
References
1. Folkerth RD. Periventricular leukomalacia: overview and recent findings. Pediatr Dev Pathol. 2006. 9:3–13.
2. Back SA. Perinatal white matter injury: the changing spectrum of pathology and emerging insights into pathogenetic mechanisms. Ment Retard Dev Disabil Res Rev. 2006. 12:129–140.
3. Rezaie P, Dean A. Periventricular leukomalacia, inflammation and white matter lesions within the developing nervous system. Neuropathology. 2002. 22:106–132.
4. Yamamoto N, Utsu M, Serizawa M, Ohki S, Murakoshi T, Seguchi M, et al. Neonatal periventricular leukomalacia preceded by fetal periventricular echodensity. Fetal Diagn Ther. 2000. 15:198–208.
5. Murata Y, Itakura A, Matsuzawa K, Okumura A, Wakai K, Mizutani S. Possible antenatal and perinatal related factor in development of cystic periventricular leukomalacia. Brain Dev. 2005. 27:17–21.
6. Funakoshi T, Ueda Y, Kobayashi A, Morikawa H, Mochizuki M. Studies on insulin-like growth factors (IGF-I, -II) and there binding proteins in normal human pregnancy. Nihon Naibunpi Gakkai Zasshi. 1990. 66:688–699.
7. Nitta A, Suzumura H, Kano K, Arisaka O. Congenital cystic periventricular leukomalacia in a small-for-gestational age full-term infant. Pediatr Int. 2008. 50:696–697.
8. Hagberg H, Peebles D, Mallard C. Models of white matter injury: comparison of infectious, hypoxic-ischemic, and excitotoxic insults. Ment Retard Dev Disabil Res Rev. 2002. 8:30–38.
9. Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, et al. Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol. 1996. 174:1433–1440.
10. Gilbert-Barness E, Kapur RP, Oligny LL, Siebert JR. Potter's pathology of the fetus, infant, and child. 2007. 2nd ed. Philadelphia (PA): Mosby Elsevier.
11. Resch B, Jammernegg A, Perl E, Riccabona M, Maurer U, Müller WD. Correlation of grading and duration of periventricular echodensities with neurodevelopmental outcome in preterm infants. Pediatr Radiol. 2006. 36:810–815.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download