Abstract
Objective
To compare the effectiveness of intracervical laminaria plus vaginal misoprostol and vaginal misoprostol only with variable dosages by analyzing the rate of spontaneous gestational sac expulsion for medical abortion within 12 hours.
Methods
This study was performed in 94 patients for missed abortion at Department of Obstetrics and Gynecology, St. Paul's Hospital, the Catholic University of Korea for 5 years (2004-2008). Forty seven patients were managed with laminaria insertion and intravaginal misoprostol 200 µg, 400 µg, or 800 µg at admission or outpatient clinic. The others were treated with only misoprostol at the same dose. We analyzed the rate of spontaneous expulsion of gestational sac within 12 hours.
Results
In non-laminaria group, spontaneous expulsion rate increased according to the doses of misoprostol (4.2%, 37.5%, and 33.3%, in 200 µg, 400 µg, and 800 µg, respectively, P =0.028). Between groups with the same misoprostol doses, no difference was observed in the spontaneous expulsion of the fetal sac within 12 hours according to the use of laminaria. On multivariate logistic regression analysis, factors that were associated significantly and independently with spontaneous expulsion of conceptus were misoprostol ≥400 µg and gestational age.
Curettage has been the method of choice for treatment of spontaneous abortion from the past. However, such a surgical treatment method can induce abortion-related complications such as bleeding, infection, and uterine damage and perforation, and increase maternal morbidity, and even in some cases it has been reported to be related to maternal death [1,2]. Medical therapy is applied in order to solve these shortcomings of the surgical method, and among drugs used in medical treatment, prostaglandin is effective for uterine contraction and cervical ripening, and especially prostaglandin E2 (PGE2) shows an outstanding effect on medical abortion [3]. However, PGE2 is expensive, and is not easy to be stored because of its chemical instability at room temperature. Moreover, it is accompanied with many gastrointestinal and cardiovascular side effects [4,5].
Recently emerging misoprostol, which is a synthetic derivative of PGE1, has been used as a drug for duodenal ulcer, but is extended to be used in obstetric field, such as induction of labor and abortion, because it induces cervical dilatation and uterine contraction [6,7]. In addition, it is inexpensive and storable at room temperature, and causes fewer side effects [6,7]. Much research has been carried out to define the most effective and best tolerated dosage and route of administration, but previous studies have reported its success rate mostly within 24 hours [8,9].
In this study, we compared the effectiveness of intracervical laminaria plus vaginal misoprostol and vaginal misoprostol only with variable dosages by analyzing the rate of spontaneous gestational sac expulsion for medical abortion within 12 hours.
This study was conducted through analyzing medical records retrospectively, and the subjects were patients that visited the hospital for missed abortion in the 1st trimester and terminated pregnancy with medical management during five years (January 1, 2004-December 31, 2008). During the period, a total of 103 patients visited for missed abortion as principal diagnosis, and were randomly administered different doses of misoprostol and/or laminaria. Exclusion criteria were inevitable abortion or incomplete abortion, administration of 600 µg misoprostol vaginally, and oral administration of misoprostol. A total of 94 patients were included in the final analysis. They were divided into the group with laminaria inserted and that without, and each group was subdivided into three groups according to misoprostol dose (200 µg, 400 µg, and 800 µg).
In our hospital, misoprostol and/or laminaria were inserted vaginally in the evening of admission day, and after 12 hours on the next morning the expulsion of the fetal sac was confirmed by ultrasound. If the gestational sac was expelled spontaneously, the patient was discharged, and if not, curettage was performed. After that, patients were followed up after 1 week. We analyzed the fetal sac and embryo size to the accurate gestational age, and accompanying symptoms such as bleeding and low abdominal pain. In order to compare the effectiveness between the treatment methods, we reviewed age, gestational age, and prior pregnancy history, such as gravida, parity, and cesarean delivery history.
Statistical analysis was used by XLSTAT ver. 2011.2.06 (Addinsoft, New York, NY, USA), and comparative analysis was performed by chi-square test for differences in qualitative variables and Student t-test for differences in continuous variables. A multivariate logistic regression model was constructed to identify independent risk factors associated with spontaneous expulsion rate and to control for confounders. Odds ratios and their 95% confidence interval were computed. Statistical significance was accepted if P-value<0.05.
Of the 94 pregnant women who visited for therapeutic pregnancy termination due to missed abortion, 47 had both the insertion of laminaria and the vaginal insertion of misoprostol, and the dose of misoprostol was 200 µg in 27 of them, 400 µg in 10, and 800 µg in 10. In addition, 47 patients had only the vaginal insertion of misoprostol, and the dose of misoprostol was 200 µg in 24 of them, 400 µg in 8, and 800 µg in 15.
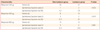
Maternal characteristic were analyzed in Table 1. In comparison with groups of different dosages of misoprostol, patients were not statistically different from each other in respect to age (31 years, 31 years, and 32 years, in 200 µg, 400 µg, and 800 µg, respectively, P =0.245), gravida (1, 2, and 1, in 200 µg, 400 µg, and 800 µg, respectively, P =0.585), parity (0.6, 0.6, and 0.5, in 200 µg, 400 µg, and 800 µg, respectively, P =0.851) and cesarean delivery history (10, 1, and 3, in 200 µg, 400 µg, and 800 µg, respectively, P =0.317). In gestational age, patients with 200 µg of misoprostol were lower than women with 400 µg and 800 µg (64 days, 75 days, and 77 days, in 200 µg, 400 µg, and 800 µg, respectively, P =0.027). In addition, these patients were divided into two groups according to the use of laminaria, and each group was subdivided into the 200 µg group, the 400 µg group, and the 800 µg group according to misoprostol dose. Table 1 shows the maternal age, gestational age, and prior pregnancy history, and statistically significant differences were observed in gestational age between the 400 µg groups, and age and gestational age between the 800 µg groups. No other statistical difference was observed.
We compared symptoms on admission such as vaginal bleeding and low abdominal pain among the groups, and found no significant difference (Table 2). In addition, ultrasonographic findings were compared in terms of gestational sac size, embryo size, and the presence of hematoma, and no difference was observed among the groups. In comparison with groups of different dosages of misoprostol, patients were not statistically different from each other in respect to vaginal bleeding (26, 8, and 11, in 200 µg, 400 µg, and 800 µg, respectively, P =0.805), abdominal pain (9, 3, and 6, in 200 µg, 400 µg, and 800 µg, respectively, P =0.769) gestational sac size (29 mm, 34 mm and 29 mm, in 200 µg, 400 µg, and 800 µg, respectively, P =0.959) embryo size (12 mm, 21 mm and 14 mm, in 200 µg, 400 µg, and 800 µg, respectively, P =0.103), and subchorionic hematoma (8, 1, and 4, in 200 µg, 400 µg and 800 µg, respectively, P =0.527).
Spontaneous expulsion rate of conceptus within 12 hours was analyzed in Table 3. In non-laminaria group, spontaneous expulsion rates increased according to the doses of misoprostol (4.2%, 37.5%, and 33.3%, in 200 µg, 400 µg, and 800 µg, respectively, P =0.028). In laminaria group, spontaneous expulsion rates were higher in the 400 µg, and 800 µg subgroups than 200 µg subgroup, but not significant statistically (7.4%, 20%, and 30%, in 200 µg, 400 µg, and 800 µg, respectively, P =0.077). Between groups with the same misoprostol dose, no difference was observed in the spontaneous expulsion of the fetal sac within 12 hours according to the use of laminaria.
On multivariate logistic regression analysis, factors that were associated significantly and independently with spontaneous expulsion of conceptus were misoprostol ≥400 µg and gestational age (Table 4). Laminaria insertion, previous abortion history and previous vaginal delivery were unrelated to increased risk of spontaneous expulsion.
No one visited emergency room or needed hospitalization for abdominal pain, vaginal bleeding or infection within 1 week of follow-up. No one required transfusion or additional curettage.
For medical abortion, it is known that combined regimen of mifepristone (antiprogesterone) and prostaglandin is more effective than prostaglandin alone, but misoprostol alone is widely used in some parts of the world, including Korea, where mifepristone is not available [10]. The reported complete abortion rate for misoprostol alone varies between 33% to 60% for single dose and 93% for repeat doses [10]. The success rates of medically-treated first trimester miscarriages varied according to dosages and route of misoprostol, the ultrasonographic definitions of pregnancy failure, time of assessment, and the criteria for success [11]. Of the different routes of misoprostol administration, vaginal route appears to be superior to oral, sublingual and buccal administration in terms of efficacy, and has fewer side effects when compared to other routes [11]. A regimen of 800 µg of misoprostol administered vaginally every 24 hours for up to three doses achieved complete abortion rates in 88% to 91% of women who were <8 weeks pregnant. This regimen takes several days [12,13]. Another regimen using 800 µg of misoprostol (administered vaginally) as an initial dose followd by 400 µg of misoprostol (administered orally) every 3 hours for three to four doses achieved complete abortion rates in 70%-85% of women [14,15].
In case pregnancy termination is performed for missed abortion in the 1st trimester, the first consideration is whether to use drug treatment or surgical treatment, and also it should be considered how to reduce the patient's anxiety and guilty feeling. In order to relieve them, we need to minimize the number of hospital visits or hospital stay and this consideration is also meaningful in terms of expenses [16,17]. According to previous reports, when misoprostol was administered the probability of the successful spontaneous expulsion of the fetal sac within 24 hours was around 80%, but it is practically difficult to wait for 24 hours after the administration of the drug [18]. One of the reasons is that outpatient follow-up after the vaginal insertion of misoprostol may result in abdominal pain or vaginal bleeding at an unpredictable time and this may cause many troubles to the patient and guardian including admission to the emergency room. For these reason, the authors compared patients who had both the insertion of laminaria and the vaginal insertion of misoprostol with those who had only the vaginal insertion of misoprostol in order to see the probability of the spontaneous expulsion of the fetal sac within 12 hours and which treatment is more successful with less pain and discomfort.
In our study, all women with a spontaneous expulsion, which was no gestational sac in endometrium confirmed by ultrasound, did not need to undergo additional surgical management. It is known that if no gestational sac is present, in the absence of heavy bleeding, intervention in most women is unnecessary [19]. This is true even when, as is common, the uterus contains sonographically evident debris [19].
Misoprostol is known as a safe agent for early pregnancy failure, but precautions should be taken into consideration in some complications and side-effects. Diarrhea is the major adverse reaction, but it is usually mild and self-limiting [20]. Fever and chills have also been reported, but are more associated with higher doses in the third trimester or immediate postpartum period [20]. In addition, medical methods are associated with a longer duration of bleeding than surgical methods [10]. Another concern is the risk of uterine rupture, especially in women with a previous uterine scar. Reports of uterine rupture are rare in first trimester medical abortion, but the risk seems to increase with gestation [20,21]. Exposure to misoprsol in early pregnancy has been associated with multiple congenital defects, therefore, counsel the women on the risk of fetal abnormality if the pregnancy is continued after exposure to misoprostol [20,22].
According to the results of this analysis, the use of laminaria did not have an effect on the spontaneous expulsion of the fetal sac. In addition, among those who had the vaginal insertion of misoprostol, the success rate was highest when the misoprostol dose was 400 µg and 800 µg. In conclusion, the vaginal insertion of misoprostol was safe and acceptable method for therapeutic pregnancy termination for missed abortion in the 1st trimester, and reduced the number of surgical intervention.
Figures and Tables
References
1. Ulmann A, Silvestre L, Chemama L, Rezvani Y, Renault M, Aguillaume CJ, et al. Medical termination of early pregnancy with mifepristone (RU 486) followed by a prostaglandin analogue. Study in 16,369 women. Acta Obstet Gynecol Scand. 1992. 71:278–283.
2. Ho PC, Ngai SW, Liu KL, Wong GC, Lee SW. Vaginal misoprostol compared with oral misoprostol in termination of second-trimester pregnancy. Obstet Gynecol. 1997. 90:735–738.
3. Kushwah DS, Kushwah B, Salman MT, Verma VK. Acceptability and safety profile of oral and sublingual misoprostol for uterine evacuation following early fetal demise. Indian J Pharmacol. 2011. 43:306–310.
4. Margulies M, Campos Pérez G, Voto LS. Misoprostol to induce labour. Lancet. 1992. 339:64.
5. Bebbington MW, Kent N, Lim K, Gagnon A, Delisle MF, Tessier F, et al. A randomized controlled trial comparing two protocols for the use of misoprostol in midtrimester pregnancy termination. Am J Obstet Gynecol. 2002. 187:853–857.
6. Conrad JT, Ueland K. The stretch modulus of human cervical tissue in spontaneous, oxytocin-induced, and prostaglandin E2-induced labor. Am J Obstet Gynecol. 1979. 133:11–14.
7. Ercan CM, Coksuer H, Karasahin KE, Alanbay I, Aydogan U, Parlak A, et al. Comparison of different preoperative sublingual misoprostol regimens for surgical termination of first trimester pregnancies: a prospective randomized trial. J Reprod Med. 2011. 56:247–253.
8. Ngai SW, To WK, Lao T, Ho PC. Cervical priming with oral misoprostol in pre-labor rupture of membranes at term. Obstet Gynecol. 1996. 87:923–926.
9. Scheepers HC, van Erp EJ, van den Bergh AS. Use of misoprostol in first and second trimester abortion: a review. Obstet Gynecol Surv. 1999. 54:592–600.
10. Kulier R, Kapp N, Gulmezoglu AM, Hofmeyr GJ, Cheng L, Campana A. Medical methods for first trimester abortion. Cochrane Database Syst Rev. 2011. 11:CD002855.
11. Vejborg TS, Nilas L, Rørbye C. Medical management of first trimester miscarriage according to ultrasonographic findings. Acta Obstet Gynecol Scand. 2007. 86:604–609.
12. Jain JK, Dutton C, Harwood B, Meckstroth KR, Mishell DR Jr. A prospective randomized, double-blinded, placebo-controlled trial comparing mifepristone and vaginal misoprostol to vaginal misoprostol alone for elective termination of early pregnancy. Hum Reprod. 2002. 17:1477–1482.
13. Zikopoulos KA, Papanikolaou EG, Kalantaridou SN, Tsanadis GD, Plachouras NI, Dalkalitsis NA, et al. Early pregnancy termination with vaginal misoprostol before and after 42 days gestation. Hum Reprod. 2002. 17:3079–3083.
14. Singh K, Fong YF, Dong F. A viable alternative to surgical vacuum aspiration: repeated doses of intravaginal misoprostol over 9 hours for medical termination of pregnancies up to eight weeks. BJOG. 2003. 110:175–180.
15. Tang OS, Wong KS, Tang LC, Ho PC. Pilot study on the use of repeated doses of misoprostol in termination of pregnancy at less than 9 weeks of gestation. Adv Contracept. 1999. 15:211–216.
16. Li YT, Hsieh JC, Hou GQ, Chen TH, Chu YC, Lin TC, et al. Simultaneous use of mifepristone and misoprostol for early pregnancy termination. Taiwan J Obstet Gynecol. 2011. 50:11–14.
17. Ngoc NT, Blum J, Raghavan S, Nga NT, Dabash R, Diop A, et al. Comparing two early medical abortion regimens: mifepristone+misoprostol vs. misoprostol alone. Contraception. 2011. 83:410–417.
18. Cabrera Y, Fernández-Guisasola J, Lobo P, Gámir S, Alvarez J. Comparison of sublingual versus vaginal misoprostol for second-trimester pregnancy termination: a meta-analysis. Aust N Z J Obstet Gynaecol. 2011. 51:158–165.
19. Cunningham F, Leveno K, Bloom S, Hauth J, Rouge D, Spong C. Williams obstetrics. 2010. 23rd ed. New York: McGraw-Hill Professional.
20. Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet. 2007. 99:Suppl 2. S160–S167.
21. Kim JO, Han JY, Choi JS, Ahn HK, Yang JH, Kang IS, et al. Oral misoprostol and uterine rupture in the first trimester of pregnancy: a case report. Reprod Toxicol. 2005. 20:575–577.
22. Orioli IM, Castilla EE. Epidemiological assessment of misoprostol teratogenicity. BJOG. 2000. 107:519–523.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download