Abstract
Objective
Although there were many studies about postoperative voiding dysfunction after anti-incontinence operation, little studies after pelvic organ prolapse operation were published. We sought to determine risk factors for voiding dysfunction (VD) after abdominal sacrocolpopexy (ASC).
Methods
ASC was performed on 89 women at Yonsei University Health System from January 2007 to December 2009. VD was defined as post void residual (PVR)>150 mL. Foley catheter was removed after the third or forth postoperative day (POD). Risk factors for VD were examined using logistic regression models.
Results
Seventeen patients (19.1%) had VD. Total abdominal hysterectomy (TAH) was performed on 70.8%, transobturator tape (TOT) on 55.1% concomitantly. There was no significant difference in age (mean±standard deviation [SD], 59.9±12.8 vs. 62.7±8.1 yr), parity (mean [range], 3 [1-5] vs. 3 [1-8]), body mass index (mean±SD, 24.0±2.7 vs. 24.4±3.6), TAH (70.6% vs. 70.8%), TOT (52.9% vs. 55.6%) and pelvic organ prolapse quantification stage 4 (94.1% vs. 68.1%, P-value 0.057). There was significant difference in diabetes mellitus (29.4% vs. 9.7%, odds rations [OR]: 3.87 [95% confidence intervals, CI: 1.05-14.23]) and the day of foley removal (POD 4: 47.1% vs. 13.9%, OR: 5.51 [95% CI: 1.72-17.64]). There was no significant difference in urodynamic parameters including maximal capacity, urethral closure pressure, maximal flow rate, mean flow rate, post void residual except detrusor pressure at maximal flow rate (Pdet at Qmax), (13±8 vs. 23±15, per 10 cm H20, OR 0.54 [95% CI: 0.31-0.95]). In the multiple logistic regression model, only Pdet at Qmax OR 0.94 (95% CI: 0.89-0.99) remained statistically significant.
Figures and Tables
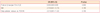
Table 1
Demographic, surgical and preoperative characteristics
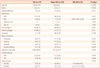
Data presented as n (%) or mean±standard deviation (SD).
VD, voding dysfunction; OR, odds ratio; CI, confidence interval; BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; ds, disease; Preop, preoperative; Sx, symptom; TAH, total abdominal hysterectomy; TOT, transobturator tape; POD, postoperative day.
References
1. Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002. 186:1160–1166.
2. Marchionni M, Bracco GL, Checcucci V, Carabaneanu A, Coccia EM, Mecacci F, et al. True incidence of vaginal vault prolapse. Thirteen years of experience. J Reprod Med. 1999. 44:679–684.
3. Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004. 104:805–823.
4. Alonzo-Sosa JE, Flores-Contreras JT, Paredes-Canul M. Method for transurethral catheterization for 1-3 days for pelvic floor relaxation in the postoperative period. Ginecol Obstet Mex. 1997. 65:455–457.
5. Hakvoort RA, Elberink R, Vollebregt A, Ploeg T, Emanuel MH. How long should urinary bladder catheterisation be continued after vaginal prolapse surgery? A randomised controlled trial comparing short term versus long term catheterisation after vaginal prolapse surgery. BJOG. 2004. 111:828–830.
6. Shiotz HA. Comparison of 1 and 3 days' transurethral Foley catheterization after vaginal plastic surgery. Int Urogynecol J. 1995. 6:158–161.
7. Beck RP, McCormick S, Nordstrom L. A 25-year experience with 519 anterior colporrhaphy procedures. Obstet Gynecol. 1991. 78:1011–1018.
8. Sokol AI, Jelovsek JE, Walters MD, Paraiso MF, Barber MD. Incidence and predictors of prolonged urinary retention after TVT with and without concurrent prolapse surgery. Am J Obstet Gynecol. 2005. 192:1537–1543.
9. Thompson JD. Rock JA, Thompson JD, editors. Surgical correction of defects in pelvic supports: pelvic organ prolapse. Te Linde's operative gynecology. 1997. 8th ed. Philadelphia (PA): Lippincott-Raverpublishers;961–979.
10. Higgs P, Goh J, Krause H, Sloane K, Carey M. Abdominal sacral colpopexy: an independent prospective long-term follow-up study. Aust N Z J Obstet Gynaecol. 2005. 45:430–434.
11. Jeon MJ, Moon YJ, Jung HJ, Lim KJ, Yang HI, Kim SK, et al. A long-term treatment outcome of abdominal sacrocolpopexy. Yonsei Med J. 2009. 50:807–813.
12. Hakvoort RA, Dijkgraaf MG, Burger MP, Emanuel MH, Roovers JP. Predicting short-term urinary retention after vaginal prolapse surgery. Neurourol Urodyn. 2009. 28:225–228.
13. Basu M, Duckett J. Effect of prolapse repair on voiding and the relationship to overactive bladder and detrusor overactivity. Int Urogynecol J Pelvic Floor Dysfunct. 2009. 02. 12. [Epub]. DOI:10.1007/s00192-009-0807-z.
14. Bhatia NN, Bergman A. Use of preoperative uroflowmetry and simultaneous urethrocystometry for predicting risk of prolonged postoperative bladder drainage. Urology. 1986. 28:440–445.
15. Sze EH, Miklos JR, Karram MM. Voiding after Burch colposuspension and effects of concomitant pelvic surgery: correlation with preoperative voiding mechanism. Obstet Gynecol. 1996. 88:564–567.
16. Vervest HA, Bisseling TM, Heintz AP, Schraffordt Koops SE. The prevalence of voiding difficulty after TVT, its impact on quality of life, and related risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:173–182.
17. Duckett JR, Patil A, Papanikolaou NS. Predicting early voiding dysfunction after tension-free vaginal tape. J Obstet Gynaecol. 2008. 28:89–92.
18. Kamilya G, Seal SL, Mukherji J, Bhattacharyya SK, Hazra A. A randomized controlled trial comparing short versus long-term catheterization after uncomplicated vaginal prolapse surgery. J Obstet Gynaecol Res. 2010. 36:154–158.
19. Huang CC, Ou CS, Yeh GP, Der Tsai H, Sun MJ. Optimal duration of urinary catheterization after anterior colporrhaphy. Int Urogynecol J Pelvic Floor Dysfunct. 2010. 11. 11. [Epub]. DOI:10.1007/s00192-010-1309-8.
20. Daneshgari F, Liu G, Birder L, Hanna-Mitchell AT, Chacko S. Diabetic bladder dysfunction: current translational knowledge. J Urol. 2009. 182:S18–S26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download