Abstract
Most chemotherapeutic drugs are known to possess significant teratogenic effects. Although several agents have been proven to be safe for the fetus after organogenesis period, there is limited information on their use during pregnancy and it is very difficult to establish researches on the effect to human. We report a very unique case of unrecognized pregnancy in lung cancer patient who had been treated with variable agents of chemotherapy. A 25-year-old woman (gravida 0) who had been diagnosed as non-small cell lung cancer 6 years ago and received multiple regimens of chemotherapy presented at full term pregnancy with unknown gestational period. Without knowledge of pregnancy, she received a palliative chemotherapy with Docetaxel during first and second trimesters. Vaginal delivery with induction of labor due to postterm pregnancy was performed after evaluation of her medical condition and fetal surveillance. A 2,450 g female newborn was delivered with no evidence of congenital malformations.
With the increasing incidence of lung cancer worldwide, coupled with increased smoking rates in women and later age of conception, it seems that lung cancer complicating pregnancy may become more common and treatment of this condition will be a more frequent problem as a consequence. Researches on the use of chemotherapy in lung cancer patients during pregnancy and its potential effects on the fetus are limited [1]. Although lung cancer develops more frequently among patients in their sixth or seventh decades of life with a male preponderance, its incidence in individuals younger than 40 years has increased currently, especially in women [2].
Most chemotherapeutic agents are known to possess potentially significant teratogenic effects. Although several agents have been proven to be safe for the fetus after organogenesis period, there is far more limited information on their use during the first trimester of pregnancy [3].
We here report a patient with metastatic non-small cell lung cancer who was treated with palliative chemotherapy from the first trimester without awareness of pregnancy.
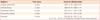
A 25-year-old woman (G0) was referred to obstetrics department of Seoul National University Hospital for incidentally found pregnancy in March 2011. She has been diagnosed as metastatic non-small cell lung cancer stage T2N2M1 in October 2005 at National Cancer Center and received multiple regimens of palliative chemotherapy until November 2010. The chemotherapeutic agents that she had been received are listed in Table 1. The last regimen was Docetaxel which had been injected since June 2010 and during Docetaxel application, she continuously complained for severe nausea, vomiting, and dizziness. On November 2010, while the fourth cycle of Docetaxel was being injected, her blood pressure dropped to 70/40 mm Hg and other vital signs went unstable. Chemotherapy was immediately ceased and since that event, the Oncology department of National Cancer Center decided to hold additional palliative chemotherapy, but kept close observation with regular follow-ups. Her last brain magnetic resonance imaging (MRI) showed no significant interval change (Fig. 1) and dry cough which had been stationary since the first time of diagnosis was the only symptom that she complained of. She never smoked or used illicit drugs.
On March 2011, she was referred to gynecology department of National Cancer Center for abdominal discomfort that had started one month ago. Her urine analysis revealed positive human chorionic gonadotropin and subsequent transabdominal ultrasound showed a fetus of about full term gestational age with good fetal movements. She lived with her mother and was unmarried. She recalled the date of her last menstrual period (LMP) at 4th of June, 2010 and the gestational age of the fetus could be estimated as about 41 weeks by LMP. For intensive counseling with obstetricians and neonatologists, she was referred to Seoul National University Hospital on the next day of diagnosis of pregnancy.
The patient was admitted for further evaluation. Her blood test revealed normal ranges except for anemia (hemoglobin 10.1 g/dL) and mild increase in liver enzyme (aspartate aminotransferase/alanine aminotransferase 49/52 IU/L). Pulmonary function test showed mild restrictive pattern and chest X-ray presented with multiple nodules in bilateral lobes (Fig. 2). A more detailed ultrasound examination was performed by an obstetrician and the fetus was suspected to be small for gestational age which was calculated by LMP, but no obvious abnormalities were found. The medical oncologist and pulmonologist examined her condition and concluded that she had no problem for proceeding induction of labor and delivery. On the next day, elective induction of labor with oxytocin infusion was performed and the patient delivered a normal female newborn whose birth weight was 2,450 g. The Apgar scores were 5 at 1 minute and 9 at 5 minutes. The placenta had no abnormality by gross examination. The fetal blood counts were normal at the time of delivery. Pediatric evaluation revealed no evidence of hearing, thyroid, adrenal, hepatorenal, and hematologic dysfunction, or gross congenital malformation in the infant. Thereafter, the infant developed normally and was discharged one week later in good condition weighing 2,900 g. The patient did not have any complications after delivery and was discharged two days later. She presented good postpartum state at office three weeks later and is planning to keep observation through oncology department without further chemotherapy for the time being.
Management of cancer during pregnancy is a great challenge. Although surgery has been found to be safe during pregnancy, chemotherapy and radiotherapy were mostly considered incompatible with normal development of fetus [4]. Recent studies of prenatal exposure to chemotherapy show a reassuring outcome for long term development of children [5]. However, data especially on human are still limited. The majority of data for chemotherapy in the pregnant female has been from breast cancer, Hodgkin's lymphoma and leukemia treatment. Although long term infant data are lacking, it is largely thought that chemotherapy administered to mother in the second or third trimester is relatively safe for the fetus [6]. Nonetheless, cytotoxic therapy has been connected to increased incidence of intrauterine growth retardation, miscarriages, stillbirths, preeclampsia and prematurity [7]. There are a few literatures showing use of chemotherapy during the first trimester is associated with the risk of spontaneous abortion, fetal death, and major malformations since the fetus is particularly vulnerable when exposed during organogenesis [8].
In this case, the patient who has been received multiple regimens of palliative chemotherapy was not aware of her pregnancy until full term pregnancy. As a result, the fetus was exposed to Docetaxel during the first and second trimesters. The baby did not show any gross congenital malformation and pediatricians found no abnormal findings through thorough evaluation during admission to neonatal intensive care unit. The use of taxanes during pregnancy has been described in few reports. Because of the limited human experience and the uniqueness of taxanes' antineoplastic mode of action, the use of taxanes in pregnancy is not recommended, however this recommendation can change as more cases of exposure are reported [8]. Information on the outcomes of patients receiving Docetaxel during pregnancy is found in three case reports with four breast cancer patients [9-11]. Three patients delivered healthy babies, and the other one delivered an infant with mild hydrocephalus which had been detected before Docetaxel therapy and persisted on serial ultrasound examinations, but regressed spontaneously over several months after birth.
This case is important in a view of reproductive counseling for cancer patients who receive chemotherapy. The patient and her physicians could not recognize her pregnancy for a long time because the patient recalled her menstrual period was very irregular since she has received palliative chemotherapy. Therefore, physicians need to pay attention to existence of menstruation and possibility of pregnancy of women who are undergoing chemotherapy even they seem to have lost ovarian function. In addition, the patient complained frequent nausea and chemotherapy was ceased due to unstable vital signs including low blood pressure during chemotherapy. The period of these symptoms corresponds with the first trimester, which implies that hyperemesis gravidarum could be mistaken as toxic effects of chemotherapeutic agents. The pathophysiologic changes that came from chemotherapy may make early detection of pregnancy even more difficult. Accordingly, it is essential for safe administration of chemotherapeutic drugs to maintain effective contraception for women of reproductive age. Close monitoring of menstrual history before and during chemotherapy in women is needed for early detection of an unintended pregnancy as well.
Since more women are delaying childbearing and the incidence of cancer before 50 years age group is increasing, it can be expected that cancer diagnosed in pregnant women will be found more often in the future [12]. Diagnosis of cancer in a woman with pregnancy results in medical and ethical dilemmas accompanied by conflicts between maternal and fetal perspectives. Therefore, additional studies and reviews of available data regarding the different aspects of treatment including chemotherapy of cancer during pregnancy as well as the effect of pregnancy on cancer prognosis are necessary.
Figures and Tables
Fig. 1
(A) Probable metastatic nodule in right post central gyrus and (B) another metastatic nodule left medial temporal lobe were found in brain magnetic resonance imaging taken in October, 2010.

References
1. Gurumurthy M, Koh P, Singh R, Bhide A, Satodia P, Hocking M, et al. Metastatic non-small-cell lung cancer and the use of gemcitabine during pregnancy. J Perinatol. 2009. 29:63–65.
2. Penha DS, Salge AK, Tironi F, Saldanha JC, Castro EC, Teixeira Vde P, et al. Bronchogenic carcinoma of squamous cells in a young pregnant woman. Ann Diagn Pathol. 2006. 10:235–238.
3. Kim JH, Kim HS, Sung CW, Kim KJ, Kim CH, Lee KY. Docetaxel, gemcitabine, and cisplatin administered for non-small cell lung cancer during the first and second trimester of an unrecognized pregnancy. Lung Cancer. 2008. 59:270–273.
4. Moran BJ, Yano H, Al Zahir N, Farquharson M. Conflicting priorities in surgical intervention for cancer in pregnancy. Lancet Oncol. 2007. 8:536–544.
5. Hahn KM, Johnson PH, Gordon N, Kuerer H, Middleton L, Ramirez M, et al. Treatment of pregnant breast cancer patients and outcomes of children exposed to chemotherapy in utero. Cancer. 2006. 107:1219–1226.
6. Meirow D, Schiff E. Appraisal of chemotherapy effects on reproductive outcome according to animal studies and clinical data. J Natl Cancer Inst Monogr. 2005. 21–25.
7. Zemlickis D, Lishner M, Degendorfer P, Panzarella T, Sutcliffe SB, Koren G. Fetal outcome after in utero exposure to cancer chemotherapy. Arch Intern Med. 1992. 152:573–576.
8. Cardonick E, Iacobucci A. Use of chemotherapy during human pregnancy. Lancet Oncol. 2004. 5:283–291.
9. De Santis M, Lucchese A, De Carolis S, Ferrazani S, Caruso A. Metastatic breast cancer in pregnancy: first case of chemotherapy with docetaxel. Eur J Cancer Care (Engl). 2000. 9:235–237.
10. Nieto Y, Santisteban M, Aramendía JM, Fernández-Hidalgo O, García-Manero M, López G. Docetaxel administered during pregnancy for inflammatory breast carcinoma. Clin Breast Cancer. 2006. 6:533–534.
11. Potluri V, Lewis D, Burton GV. Chemotherapy with taxanes in breast cancer during pregnancy: case report and review of the literature. Clin Breast Cancer. 2006. 7:167–170.
12. Stensheim H, Moller B, van Dijk T, Fosså SD. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol. 2009. 27:45–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download