Abstract
Objective
We analyzed subtypes of human papilloma virus (HPV) infection in Papanicolaou (Pap) smear results of women in Jeju island, Korea.
Methods
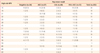
We investigated the distribution of HPV subtypes according to Pap smear results among 635 women in Jeju island, Korea between October 2005 and October 2010.
Results
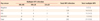
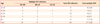
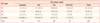
The most prevalent HPV subtypes were HPV 16, 52, 53, 58 in negative Pap smear result and HPV 16, 52, 31, 53, 66 in atypical squamous cell, HPV 52, 53, 56, 66 in low grade squamous intraepithelial lesion, HPV 16, 58, 52, 33, 33 in high grade squamous intraepithelial lesion/squamous cell carcinoma each other. The subtypes of HPV 16, 52, 53, 58, 31 were common in all women participated in study from Jeju island, Korea. And multiple infections were more common in women under 30 years of age than above age as previous study and the majority of HPV multiple infections were high risk types (94.5%).
Conclusion
This prevalence was some different from previous study of Korean other region, but more similar to Japanese study data. We think this result shows that Jeju island women maybe have the genetic, regional or environmental close relationship with Japanese because of close distance and culture irrespective of different national race.
Figures and Tables
References
1. McCrory DC, Matchar DB, Bastian L, Datta S, Hasselblad V, Hickey J, et al. Report No.: 99-E010. Evaluation of cervical cytology. Evidence report/technology assessment No. 5. 1999. Rockville (MD): Agency for Health Care Policy and Research.
2. Kim JW, Kang SB, Seo DK, Choi SH, Lee CM, Kim YB, et al. Cytologic screening history of 249 patients with cervical cancer. J Korean Cancer Assoc. 1998. 30:1198–1206.
3. Mandelblatt JS, Lawrence WF, Womack SM, Jacobson D, Yi B, Hwang YT, et al. Benefits and costs of using HPV testing to screen for cervical cancer. JAMA. 2002. 287:2372–2381.
4. Saslow D, Runowicz CD, Solomon D, Moscicki AB, Smith RA, Eyre HJ, et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002. 52:342–362.
5. Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst. 1995. 87:796–802.
6. Castellsagué X, Díaz M, de Sanjosé S, Muñoz N, Herrero R, Franceschi S, et al. Worldwide human papillomavirus etiology of cervical adenocarcinoma and its cofactors: implications for screening and prevention. J Natl Cancer Inst. 2006. 98:303–315.
7. Hildesheim A, Schiffman MH, Gravitt PE, Glass AG, Greer CE, Zhang T, et al. Persistence of type-specific human papillomavirus infection among cytologically normal women. J Infect Dis. 1994. 169:235–240.
8. Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al. A systematic review of the role of human papilloma virus (HPV) testing within a cervical screening programme: summary and conclusions. Br J Cancer. 2000. 83:561–565.
9. Cuzick J. Screening for cancer: future potential. Eur J Cancer. 1999. 35:1925–1932.
10. zur Hausen H. Human papillomaviruses and their possible role in squamous cell carcinomas. Curr Top Microbiol Immunol. 1977. 78:1–30.
11. Bao YP, Li N, Smith JS, Qiao YL. ACCPAB members. Human papillomavirus type distribution in women from Asia: a meta-analysis. Int J Gynecol Cancer. 2008. 18:71–79.
12. Li LK, Dai M, Clifford GM, Yao WQ, Arslan A, Li N, et al. Human papillomavirus infection in Shenyang City, Peoples Republic of China: A population-based study. Br J Cancer. 2006. 95:1593–1597.
13. Wheeler C. Human papillomavirus type specific prevalence. The Human Papillomaviruses Compendium On Line [Internet]. c1999. cited 2011 Oct 15. Los Alamos (NM): Los Alamos National laboratory;Available from: http://www.stdgen.lanl.gov/COMPENDIUM_PDF/96PDF/3/wheeler.pdf.
14. de Roda Husman AM, Walboomers JM, Meijer CJ, Risse EK, Schipper ME, Helmerhorst TM, et al. Analysis of cytomorphologically abnormal cervical scrapes for the presence of 27 mucosotropic human papillomavirus genotypes, using polymerase chain reaction. Int J Cancer. 1994. 56:802–806.
15. Gargiulo F, De Francesco MA, Schreiber C, Ciravolo G, Salinaro F, Valloncini B, et al. Prevalence and distribution of single and multiple HPV infections in cytologically abnormal cervical samples from Italian women. Virus Res. 2007. 125:176–182.
16. Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002. 55:244–265.
17. Chan PK, Li WH, Chan MY, Ma WL, Cheung JL, Cheng AF. High prevalence of human papillomavirus type 58 in Chinese women with cervical cancer and precancerous lesions. J Med Virol. 1999. 59:232–238.
18. Park AM, Koh SB. Prevalence and distribution of single and multiple HPV infections in cervical cancer and precancerous lesion from Daegu and Gyeongbuk province. Korean J Obstet Gynecol. 2008. 51:1128–1136.
19. Choi SH, Baik KD, Lee SI. An analysis of HPV subtype in the uterine cervix and clinical usefulness of HPV DNA chip test. Korean J Obstet Gynecol. 2007. 50:465–475.
20. Kim CJ, Jeong JK, Park M, Park TS, Park TC, Namkoong SE, et al. HPV oligonucleotide microarray-based detection of HPV genotypes in cervical neoplastic lesions. Gynecol Oncol. 2003. 89:210–217.
21. Cho NH, An HJ, Jeong JK, Kang S, Kim JW, Kim YT, et al. Genotyping of 22 human papillomavirus types by DNA chip in Korean women: comparison with cytologic diagnosis. Am J Obstet Gynecol. 2003. 188:56–62.
22. Hwang TS, Jeong JK, Park M, Han HS, Choi HK, Park TS. Detection and typing of HPV genotypes in various cervical lesions by HPV oligonucleotide microarray. Gynecol Oncol. 2003. 90:51–56.
23. Kim PY, Lee DW, Seo JH, Sunwoo JG, Bae DH, Jeong DJ. A study for the prevalence of high-risk HPV subtype in uterine cervical neoplasia of Korean women. Korean J Obstet Gynecol. 2003. 46:2005–2012.
24. Lee JH, Lee KH, Lee IH, Woo HJ, Seong SJ, Kim TJ, et al. Clinical efficacy of HPV DNA chip test in human papillomavirus detection of uterine cervix. Korean J Obstet Gynecol. 2006. 49:2128–2136.
25. Sasagawa T, Basha W, Yamazaki H, Inoue M. High-risk and multiple human papillomavirus infections associated with cervical abnormalities in Japanese women. Cancer Epidemiol Biomarkers Prev. 2001. 10:45–52.
26. Grinsztejn B, Veloso VG, Levi JE, Velasque L, Luz PM, Friedman RK, et al. Factors associated with increased prevalence of human papillomavirus infection in a cohort of HIV-infected Brazilian women. Int J Infect Dis. 2009. 13:72–80.
27. Chang DY, Chen RJ, Lee SC, Huang SC. Prevalence of single and multiple infection with human papillomaviruses in various grades of cervical neoplasia. J Med Microbiol. 1997. 46:54–60.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download