Abstract
Primary uterine non-Hodgkin's lymphoma is a rare malignancy and the most common histological subtype is the diffuse large B-cell lymphoma. This case is a patient underwent surgery for early gastric cancer in November 2007, and determined to be completely cured, and subsequently, during the follow up observation, in pelvic computed tomography, a uterine mass suspicious to be either uterine cervical cancer or uterine sarcoma was observed. She was transferred to department of gynecologic oncology, modified radical hysterectomy and pelvic lymph node dissection were performed. Histologically the uterine mass was diagnosed as diffuse large B-cell lymphoma. Currently she is received the rituximab, cyclophosphamide, adriamycin, vincristine, and prednisone chemotherapy. Thus we report the case with a brief review of the literature. Primary malignant lymphoma in the uterus is very rare, and its diagnosis as well as treatments has not been established. Therefore, in the future, through continuous clinical discussion on this disease, a guideline for the diagnosis and treatment for primary uterine lymphoma should be established.
Primary lymphoma occurring in the female reproductive system is a very rare disease, and it accounts for merely approximately 0.54-0.64% of extra-nodal non-Hodgkin's lymphomas (NHL). The lymphoma occurring in the female reproductive system is diffused type, and in the histological classification, diffuse large B-Cell lymphoma is most prevalent [1,2]. Among them, in cases of lymphoma developed in the uterine cervix or the uterine body, clinical symptoms or imaging tests are not specific, and thus its diagnosis is delayed until the definite diagnosis by postsurgical histological test in many cases.
A 67-year-old female patient underwent partial gastrectomy for gastric cancer in November 2007, determined to be complete cure and under the follow up observation without special symptoms and findings, and in pelvic computed tomography (CT) performed during the follow up observation, a mass suspicious to be either uterine sarcoma or uterine cervical cancer in the uterine cervix as well as the uterine body was detected, and thus transferred to our department of gynecologic oncology.
At the time of admission, blood pressure was 100/70, pulse was 72, temperature was 36.5℃, and general condition was good, and in pelvic examination, a mass and the erosion of the uterine cervix were not detected macroscopically.
In blood test, hemoglobin was 11.2 g/dL, red blood cell volume was 31.4%, leukocyte was 4,800/mm3, platelet was 229,000/mm3, and they were within normal ranges, and in urine test, protein was detected, nonetheless, glucose was not detected. In addition, in biochemistry test, abnormal results were not reported. The tumor marker Ca 72-4 was 1.08 and CA 19-9 was 5.63, which were normal, and in addition, CA-125 was 6.7, and normal results were shown. In Papanicolaou test (PAP test) performed but special results were not shown.
In pelvic computed tomography a lobular shape mass of 7.6×6.5 cm in size showing heterogeneous contrast enhancement was detected (Fig. 1) in the vicinity of the uterine cervix, and other than that, recurrence or other special findings in the stomach resection area was not detected. And in positron emission tomography-computed tomography a mass approximately 8.5 cm in size with increased F-18 fluorodeoxyglucose intake was observed in the uterine cervical area, and it was speculated to be either uterine cervical cancer or uterine sarcoma showing a fast growing pattern (Fig. 2).
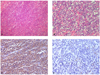
Under general anesthesia, open abdominal surgery was performed by lower abdominal transverse incision. The total uterus was 14.0×8.0×3.0 cm in size, and a mass 8×9 cm in size originated from the exocervix and appeared to be malignant was detected in the inside of uterus, and in the frozen biopsy, it was diagnosed as either small cell carcinoma or sarcoma. Because of the columnar shape of malignant tumor, the entire uterus was shown as a dumbbell shape. The mass invaded particularly the uterus and the upper vagina, grew to the left side laterally, and closely adhered to the external iliac vessel, and due to it, the partial stenosis of the left ureter was observed, and thus during surgery, a Double J-catheter was inserted. Both ovaries did not show special findings, nonetheless, the left ovary was firmly attached to the uterine body, and both oviducts were attached to the pelvic wall. Infiltrative tumors were detected even in the Douglas pouch, and thus after its resection, biopsy was performed. Depending on the location of the malignant mass invaded from the uterine body to the uterine cervix, adjuvant radical total hysterectomy, pelvic lymph dissection, the resection of tumors infiltrated the Douglas pouch and in the vicinity of the bladder were performed, and the surgery was completed. Microscopically each cell showed the large or medium size bullous nucleus, the distinct nucleolus, frequent cell division, and a small amount of cytoplasm. And in immunohistochemical staining, the positive reaction to CD 20 and CD79a and the negative reaction to CD 45RO and CD3 were shown, and thus it was diagnosed as diffuse large B-cell lymphoma (Fig. 3).
After surgery, the patient recovered without special symptoms. And histopathologically, it was diagnosed as diffuse large B-cell lymphoma. In the thoracic computed tomography taken after the diagnosis, special findings were not shown. After the transfer to the department of hematological oncology, it was decided to administer the chemotherapy rituximab (375 mg/m2), cyclophosphamide (750 mg/m2), adriamycin (50 mg/m2), vincristine (1.4 mg/m2), and prednisone (100 mg) (R-CHOP). Presently, after the second cycle of chemotherapy, general weakness and leukopenia were developed repeatedly, and thus chemotherapy was terminated, and currently under the follow up observation.
The trend of the incidence of NHL is on the continuous increase since the 1930s, and the incidence of average 3.5 cases in 100,000 individuals annually in 1935-1939 was increased to average 20 cases in 100,000 individuals annually in 1990-1994 [3]. Such increase could be considered to reflect the improvement of diagnostic method and histological diagnosis rather than the increase of the incidence. 30% of NHL occur in tissues other than lymph nodes, which is referred to as extranodal lymphoma, and in ¼ of the most prevalent subtype of NHL diffuse large B cell lymphoma (DLBCL), it occurs as extranodal primary lymphoma [4]. The cases developing lymphoma as the secondary lesion in the female reproductive system are approximately 40%, nonetheless the cases developing as a primary lesion is very rare, and tumors originated from the ovary account for 49%, originated from the uterus are 29%, and originated from the oviduct account for approximately 11% [5,6]. For the diagnosis of primary lymphoma developed in the female reproductive system, it has to be diagnosed first that tumors show the pattern restricted to the uterus, it has to be evaluated comprehensively that the evidence of disease is absent in organs other than the uterus, and the evidence of leukemia should be absent in blood tests [7]. In cases developed primary lymphoma in the uterus, vaginal hemorrhage is presented with most frequently, and in addition, non-specific pelvic pain, vaginal hemorrhage after intercourse, dyspareunia, etc. may be presented with, and as in our case, gynecological symptoms are absent in some cases. Nevertheless, the B symptoms showing in systemic lymphoma, such as high fever, night sweating, and weight loss do not manifest frequently [8]. Uterine primary lymphoma requires the differential diagnosis from inflammatory diseases, and malignant diseases such as uterine cervical cancer, cancer in the uterine body, and uterine sarcoma, and for its accurate diagnosis, histopathological test as well as immunohistochemical test are prerequisite [6,9]. Particularly, lymphomas developed in the uterine cervix are originated from the uterine cervical parenchyma and located below the epithelium, and the squamous cell layer above them is maintained intact, and thus it is a difficult task to detect lymphoma by PAP test [10].
Upon the diagnosis of lymphoma by histological test, the differential diagnosis for the cell type of the origin of lymphoma is performed, and the final diagnosis is made by performing the staining for B cell and T cell specific markers such as CD 20, CD 79a, CD 45RO, and CD 3. In our case, the positive reaction to CD 20 and CD 79a was shown and the negative reaction to CD 45RO and CD 3 was shown, and thus it was able to be diagnosed as lymphoma originated from B cells. The primary lymphoma developed in the female reproductive system is very rare, and thus the treatment protocol has not been established, and according to reports, surgery, chemotherapy, and radiation therapy alone, the combination with postoperative adjuvant chemotherapy, the simultaneous treatment of chemotherapy and radiation therapy, etc. have been attempted [8,10]. Based on recently reported studies, the anti-CD-20 immunochemotherapy the R-CHOP regimen has been administered as the effective standard therapy [11,12]. Rituximab is the monoclonal antibody used for the treatment of B cell lymphoma for the first time, and because of its clinical effectiveness and little drug side effects, it has been established as a treatment regimen [11].
Primary malignant lymphoma in the uterus is very rare, and the symptoms as well as syndromes are non-specific, and thus its diagnosis as well as treatments has not been established. Therefore, in the future, through continuous clinical discussion on this disease, a guideline for the diagnosis and treatment for primary uterine lymphoma should be established.
Figures and Tables
Fig. 1
Pelvic computed tomography. they show that the about 7.6×6.5 sized lobulated, heterogenous contrast enhancing mass in around uterine cervix (arrow).
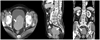
Fig. 2
Positron emission tomography-computed tomography (PET-CT). Whole body PET-CT shows an about 8.5 cm sized mass with increased F-18 fluorodeoxyglucose uptake at cervix and upper vagina, suggesting rapid growing atypical uterine cervical cancer or sarcoma (arrow).
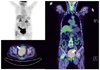
Fig. 3
(A) On low magnification, the architecture is replaced by neoplastic process with a diffuse growth pattern (H&E, ×100). (B) On high magnification, the tumor cells have large nuclei with dispersed chromatin, small nucleoli, and a variable amount of cytoplasm (H&E, ×400). (C) CD20 demonstrates positive staining in the cytoplasm of tumor cells (Immune stain for CD20, ×400). (D) CD3 demonstrates negative staining in the cytoplasm of tumor cells (immune stain for CD3, ×400).
References
1. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972. 29:252–260.
2. Stroh EL, Besa PC, Cox JD, Fuller LM, Cabanillas FF. Treatment of patients with lymphomas of the uterus or cervix with combination chemotherapy and radiation therapy. Cancer. 1995. 75:2392–2399.
3. Polednak AP. Trends in cancer incidence in Connecticut. Conn Med. 1997. 61:211–218.
4. Harris NL. Jaffe EJ, Harris NL, Stein H, editors. Mature B-cell neoplasm. WHO classification of tumours: pathology and genetics of tumours of haematopoietic and lymphoid tissues. 2001. Lyon (FR): IARC Press;121–126.
5. Chorlton I, Karnei RF Jr, King FM, Norris HJ. Primary malignant reticuloendothelial disease involving the vagina, cervix, and corpus uteri. Obstet Gynecol. 1974. 44:735–748.
6. Kuo HC, Chou CY, Chang CH, Liu MT, Tzeng CC, Huang KE. Primary malignant lymphoma of the uterine cervix shows favorable response to neoadjuvant chemotherapy. Gynecol Oncol. 1994. 52:408–410.
7. Wilson JD, Braunwald E, Isselbacher KJ, Petersdorf RG, Martin JB, Fauci AS, et al. Harrison's principles of internal medicine. 1991. 12th ed. New York (YK): McGraw-Hill.
8. Dursun P, Gultekin M, Bozdag G, Usubutun A, Uner A, Celik NY, et al. Primary cervical lymphoma: report of two cases and review of the literature. Gynecol Oncol. 2005. 98:484–489.
9. Szantho A, Balega JJ, Csapo Z, Sreter LL, Matolcsy A, Papp Z. Primary non-Hodgkin's lymphoma of the uterine cervix successfully treated by neoadjuvant chemotherapy: case report. Gynecol Oncol. 2003. 89:171–174.
10. Chan JK, Loizzi V, Magistris A, Hunter MI, Rutgers J, DiSaia PJ, et al. Clinicopathologic features of six cases of primary cervical lymphoma. Am J Obstet Gynecol. 2005. 193:866–872.
11. Boye J, Elter T, Engert A. An overview of the current clinical use of the anti-CD20 monoclonal antibody rituximab. Ann Oncol. 2003. 14:520–535.
12. Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002. 346:235–242.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download