Abstract
Lymphogranuloma venereum (LGV) is a rare sexually transmitted disease caused by chlamydia trachomatis serotypes L1-L3. The peak incidence occurs in persons 29 to 47 years old, and men are six times more likely than women to manifest clinical infection. The disease clinically manifests in three stages: a primary lesion consisting of a superficial ulcer or erosion, a secondary stage with prominent lymphadenopathy and a later stage with disease manifestations such as fibrosis, fistula, and anorectal strictures. The diagnosis of LGV is based on clinical suspicion, epidemiologic information, and the exclusion of other causes of inguinal lymphadenopathy. Diagnosis of LGV may be difficult. Patients with a clinical syndrome consistent with LGV, including genital ulcer with lymphadenopathy, should be treated for LGV. Recently we have experienced a case of LGV in 44-years-old women with inguinal bubo and sclerosing fibrous skin. We treated her with doxycycline and advancement flap.
Figures and Tables
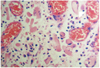
Fig. 1
Gross finding showed both inguinal bubo (arrowhead) and multiple granulation tissues, fistula, and abscess formations (arrow).

References
1. Mabey D, Peeling RW. Lymphogranuloma venereum. Sex Transm Infect. 2002. 78:90–92.
2. Centers for Disease Control and Prevention (CDC). Lymphogranuloma venereum among men who have sex with men--Netherlands, 2003-2004. MMWR Morb Mortal Wkly Rep. 2004. 53:985–988.
3. Nieuwenhuis RF, Ossewaarde JM, Götz HM, Dees J, Thio HB, Thomeer MG, et al. Resurgence of lymphogranuloma venereum in Western Europe: an outbreak of Chlamydia trachomatis serovar l2 proctitis in The Netherlands among men who have sex with men. Clin Infect Dis. 2004. 39:996–1003.
4. Herida M, Sednaoui P, Couturier E, Neau D, Clerc M, Scieux C, et al. Rectal lymphogranuloma venereum, France. Emerg Infect Dis. 2005. 11:505–506.
5. Blank S, Schillinger JA, Harbatkin D. Lymphogranuloma venereum in the industrialised world. Lancet. 2005. 365:1607–1608.
6. Meyer T, Arndt R, von Krosigk A, Plettenberg A. Repeated detection of lymphogranuloma venereum caused by Chlamydia trachomatis L2 in homosexual men in Hamburg. Sex Transm Infect. 2005. 81:91–92.
7. Kropp RY, Wong T. Canadian LGV Working Group. Emergence of lymphogranuloma venereum in Canada. CMAJ. 2005. 172:1674–1676.
8. French P, Ison CA, Macdonald N. Lymphogranuloma venereum in the United Kingdom. Sex Transm Infect. 2005. 81:97–98.
9. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010. 59:1–110.
10. Watson DJ, Parker AJ, Macleod TI. Lymphogranuloma venereum of the tonsil. J Laryngol Otol. 1990. 104:331–332.
11. Thorsteinsson SB, Musher DM, Min KW, Gyorkey F. Lymphogranuloma venereum. A cause of cervical lymphadenopathy. JAMA. 1976. 235:1882.
12. Dangor Y, Ballard RC, da L Exposto F, Fehler G, Miller SD, Koornhof HJ. Accuracy of clinical diagnosis of genital ulcer disease. Sex Transm Dis. 1990. 17:184–189.
13. Drew O, Smith Y, Jackie S. Sexually transmitted infections. Medicine. 2007. 35:410–412.
14. Marchand C, Granier F, Cetre JC, Brutzkus A, Perrot H. Anal lymphogranuloma venereum with erythema nodosa. Apropos of a case. Ann Dermatol Venereol. 1987. 114:65–69.
15. Schachter J, Osoba AO. Lymphogranuloma venereum. Br Med Bull. 1983. 39:151–154.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download