Abstract
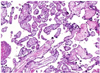
Placental infarction is a localized area of ischemic villous necrosis, resulting from interruption in maternal blood supply. These have been associated with postterm pregnancies, maternal hypertension, and anticardiolipin antibodies. Most are due to thrombotic occlusion of an uteroplacental artery. But, infarction in the basal layer of the placenta is very rare and characterized histologically by massive deposition of fibrin. The etiology remains uncertain. However, it has clearly associated with significant perinatal morbidity and mortality including stillbirth, preterm birth, and intrauterine growth restriction. This condition has been diagnosed by prenatal ultrasonography with hyperechoic areas along the maternal side, but extending through much of the placental tissue. Recently we have experienced a case of extensive infarction in the basal layer of the placenta diagnosed by prenatal ultrasonography at 17 weeks, resulted in stillbirth. We describe this case with a brief review of the literature.
Figures and Tables
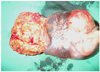
Fig. 1
Transabdominal sonogram showed an abnormally thick and 76×33 mm sized hypoechoic areas along the basal layer of placenta, but extending through much of the placental tissue.

References
1. Benirschke K, Driscoll SG. Benirschke K, Driscoll SG, editors. Maternal floor infarction. Pathology of the human placenta. 1967. New York (NY): Springer-Verlag;328–330.
2. Benirschke K, Kaufmann SL. Pathology of the human placenta. J Perinatol. 1995. 15:245–250.
3. Andres RL, Kuyper W, Resnik R, Piacquadio KM, Benirschke K. The association of maternal floor infarction of the placenta with adverse perinatal outcome. Am J Obstet Gynecol. 1990. 163:935–938.
4. Mandsager NT, Bendon R, Mostello D, Rosenn B, Miodovnik M, Siddiqi TA. Maternal floor infarction of the placenta: prenatal diagnosis and clinical significance. Obstet Gynecol. 1994. 83:750–754.
5. Vernof KK, Benirschke K, Kephart GM, Wasmoen TL, Gleich GJ. Maternal floor infarction: relationship to X cells, major basic protein, and adverse perinatal outcome. Am J Obstet Gynecol. 1992. 167:1355–1363.
6. Bane AL, Gillan JE. Massive perivillous fibrinoid causing recurrent placental failure. BJOG. 2003. 110:292–295.
7. Adams-Chapman I, Vaucher YE, Bejar RF, Benirschke K, Baergen RN, Moore TR. Maternal floor infarction of the placenta: association with central nervous system injury and adverse neurodevelopmental outcome. J Perinatol. 2002. 22:236–241.
8. Bendon RW, Hommel AB. Maternal floor infarction in autoimmune disease: two cases. Pediatr Pathol Lab Med. 1996. 16:293–297.
9. Gersell DJ. Chronic villitis, chronic chorioamnionitis, and maternal floor infarction. Semin Diagn Pathol. 1993. 10:251–266.
10. Robb JA, Benirschke K, Mannino F, Voland J. Intrauterine latent herpes simplex virus infection: II. Latent neonatal infection. Hum Pathol. 1986. 17:1210–1217.
11. Jauniaux E, Campbell S. Ultrasonographic assessment of placental abnormalities. Am J Obstet Gynecol. 1990. 163:1650–1658.
12. Katzman PJ, Genest DR. Maternal floor infarction and massive perivillous fibrin deposition: histological definitions, association with intrauterine fetal growth restriction, and risk of recurrence. Pediatr Dev Pathol. 2002. 5:159–164.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download