Abstract
Objective
To investigate the effect of intrauterine environment on adiponectin level in cord blood through comparison of normal pregnancy group and gestational diabetes group.
Methods
This cross sectional study included women with: normal pregnancy (n = 204); and patients with gestational diabetes mellitus (GDM) (n = 204). Among GDM patients, 118 were managed with diet alone and 86 were insulin requiring. Cord serum adiponectin concentration at birth was measured by enzyme-linked immunosorbent assay.
Results
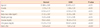
Cord serum adiponectin concentration was higher in GDM treatment pregnancies compared with normal pregnancies (P = 0.02). Cord serum adiponectin concentration was higher in female compared with male fetuses both normal and gestational diabetes pregnancies (P = 0.04, P = 0.03). In normal pregnancies, cord serum adiponectin concentration was positively correlated with gestational age (r = 0.2374, P < 0.02). In normal pregnancies, cord serum adiponectin concentration did not correlated with birth weight (r = -0.05, P > 0.05). Cord serum adiponectin concentration was not different between only diet treated women and insulin requiring women in GDM (P > 0.05).
Figures and Tables
Fig. 2
Correlation of birth weight to cord serum adiponectin in normal pregnancies. Adjusted for gestational age, infant's sex.

Fig. 3
Cord serum adiponectin concentration in normal pregnancies and gestational diabetes mellitus pregnancies. Adjusted for gestational age, infant's sex.

References
1. Dehghan M, Akhtar-Danesh N, Merchant AT. Childhood obesity, prevalence and prevention. Nutr J. 2005. 4:24.
2. Alexe DM, Syridou G, Petridou ET. Determinants of early life leptin levels and later life degenerative outcomes. Clin Med Res. 2006. 4:326–335.
3. Dunger DB, Ong KK. Endocrine and metabolic consequences of intrauterine growth retardation. Endocrinol Metab Clin North Am. 2005. 34:597–615.
4. Holt RI, Byrne CD. Intrauterine growth, the vascular system, and the metabolic syndrome. Semin Vasc Med. 2002. 2:33–43.
5. Hu E, Liang P, Spiegelman BM. AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem. 1996. 271:10697–10703.
6. Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem. 1995. 270:26746–26749.
7. Goldfine AB, Kahn CR. Adiponectin: linking the fat cell to insulin sensitivity. Lancet. 2003. 362:1431–1432.
8. Berg AH, Combs TP, Du X, Brownlee M, Scherer PE. The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med. 2001. 7:947–953.
9. Meier U, Gressner AM. Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin Chem. 2004. 50:1511–1525.
10. Kajantie E, Hytinantti T, Hovi P, Andersson S. Cord plasma adiponectin: a 20-fold rise between 24 weeks gestation and term. J Clin Endocrinol Metab. 2004. 89:4031–4036.
11. Lindsay RS, Walker JD, Havel PJ, Hamilton BA, Calder AA, Johnstone FD, et al. Adiponectin is present in cord blood but is unrelated to birth weight. Diabetes Care. 2003. 26:2244–2249.
12. Chan TF, Yuan SS, Chen HS, Guu CF, Wu LC, Yeh YT, et al. Correlations between umbilical and maternal serum adiponectin levels and neonatal birthweights. Acta Obstet Gynecol Scand. 2004. 83:165–169.
13. Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med. 1983. 308:242–245.
14. Silverman BL, Landsberg L, Metzger BE. Fetal hyperinsulinism in offspring of diabetic mothers. Association with the subsequent development of childhood obesity. Ann N Y Acad Sci. 1993. 699:36–45.
15. Pettitt DJ, Nelson RG, Saad MF, Bennett PH, Knowler WC. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care. 1993. 16:310–314.
16. Weiss PA, Scholz HS, Haas J, Tamussino KF, Seissler J, Borkenstein MH. Long-term follow-up of infants of mothers with type 1 diabetes: evidence for hereditary and nonhereditary transmission of diabetes and precursors. Diabetes Care. 2000. 23:905–911.
17. Plagemann A, Harder T, Kohlhoff R, Rohde W, Dörner G. Glucose tolerance and insulin secretion in children of mothers with pregestational IDDM or gestational diabetes. Diabetologia. 1997. 40:1094–1100.
18. Silverman BL, Metzger BE, Cho NH, Loeb CA. Impaired glucose tolerance in adolescent offspring of diabetic mothers. Relationship to fetal hyperinsulinism. Diabetes Care. 1995. 18:611–617.
19. WHO Expert Committee on Diabetes Mellitus: second report. World Health Organ Tech Rep Ser. 1980. 646:1–80.
20. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999. 257:79–83.
21. Yang WS, Lee WJ, Funahashi T, Tanaka S, Matsuzawa Y, Chao CL, et al. Weight reduction increases plasma levels of an adipose-derived anti-inflammatory protein, adiponectin. J Clin Endocrinol Metab. 2001. 86:3815–3819.
22. Havel PJ, Stanhope KL, Sinha M, Dubuc GR, Phinney SD. Gender differences in circulating adiponectin concentrations and in adiponectin responses to 7 d of energy restriction in normal weight men and women (Abstract 1867P). Proc 62nd Annual Meeting of the American Diabetes Association. 2002. 2002 June 14-18; San Francisco (CA). Washington, DC: American Diabetes Association;A454.
23. Delporte ML, Brichard SM, Hermans MP, Beguin C, Lambert M. Hyperadiponectinaemia in anorexia nervosa. Clin Endocrinol (Oxf). 2003. 58:22–29.
24. Sivan E, Mazaki-Tovi S, Pariente C, Efraty Y, Schiff E, Hemi R, et al. Adiponectin in human cord blood: relation to fetal birth weight and gender. J Clin Endocrinol Metab. 2003. 88:5656–5660.
25. Yamauchi T, Kamon J, Waki H, Murakami K, Motojima K, Komeda K, et al. The mechanisms by which both heterozygous peroxisome proliferator-activated receptor gamma (PPARgamma) deficiency and PPARgamma agonist improve insulin resistance. J Biol Chem. 2001. 276:41245–41254.
26. Kamon J, Yamauchi T, Waki H, Uchida S, Ito C, Suzuki H, et al. Mechanism for the regulation of adiponectin expression (Abstract 351P). Proc 62nd Annual Meeting of the American Diabetes Association. 2002. 2002 June 14-18; San Francisco, CA. Washington, DC: American Diabetes Association;A87.
27. Boulton TJ, Dunlop M, Court JM. The growth and development of fat cells in infancy. Pediatr Res. 1978. 12:908–911.
28. Soriguer Escofet FJ, Esteva de Antonio I, Tinahones FJ, Pareja A. Adipose tissue fatty acids and size and number of fat cells from birth to 9 years of age: a cross-sectional study in 96 boys. Metabolism. 1996. 45:1395–1401.
29. Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C. Williams obstetrics. 2009. 23th ed. New York: McGraw-Hill Professional.
30. Kishore U, Reid KB. Modular organization of proteins containing C1q-like globular domain. Immunopharmacology. 1999. 42:15–21.
31. Bullen JW Jr, Bluher S, Kelesidis T, Mantzoros CS. Regulation of adiponectin and its receptors in response to development of diet-induced obesity in mice. Am J Physiol Endocrinol Metab. 2007. 292:E1079–E1086.
32. Hotta K, Funahashi T, Arita Y, Takahashi M, Matsuda M, Okamoto Y, et al. Plasma concentrations of a novel, adiposespecific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol. 2000. 20:1595–1599.
33. Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab. 2001. 86:1930–1935.
34. Mantzoros CS, Rifas-Shiman SL, Williams CJ, Fargnoli JL, Kelesidis T, Gillman MW. Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics. 2009. 123:682–689.
35. Bozzetti P, Ferrari MM, Marconi AM, Ferrazzi E, Pardi G, Makowski EL, et al. The relationship of maternal and fetal glucose concentrations in the human from midgestation until term. Metabolism. 1988. 37:358–363.
36. Leturque A, Ferre P, Burnol AF, Kande J, Maulard P, Girard J. Glucose utilization rates and insulin sensitivity in vivo in tissues of virgin and pregnant rats. Diabetes. 1986. 35:172–177.
37. Hill DE. Insulin and fetal growth. Prog Clin Biol Res. 1976. 10:127–139.
38. Pirc LK, Owens JA, Crowther CA, Willson K, De Blasio MJ, Robinson JS. Mild gestational diabetes in pregnancy and the adipoinsular axis in babies born to mothers in the ACHOIS randomised controlled trial. BMC Pediatr. 2007. 7:18.
39. Lain KY, Garabedian MJ, Daftary A, Jeyabalan A. Neonatal adiposity following maternal treatment of gestational diabetes with glyburide compared with insulin. Am J Obstet Gynecol. 2009. 200:501.e1–501.e6.
40. Stettler N. Nature and strength of epidemiological evidence for origins of childhood and adulthood obesity in the first year of life. Int J Obes (Lond). 2007. 31:1035–1043.
41. Rosenbaum M, Leibel RL, Hirsch J. Obesity. N Engl J Med. 1997. 337:396–407.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download