Abstract
Objective
To know the correlation of punch-biopsy proven cervical intraepithelial neoplasia (CIN) 3 with the results of cone and hysterectomy.
Methods
We reviewed the medical records from 1999 to 2008, retrospectively, at a single institution. We checked age, cone and hysterectomy biopsy results, preoperative cervical smear results as well as human papillomavirus results.
Results
There were 104 patients whose punch biopsy results were CIN 3. 59 (56.7%) patients underwent cone and 45 did hysterectomy after punch biopsies. Cone found 6.8% of cervical cancer. Among patients undergoing hysterectomy without cone, 8.9% had cervical cancers. There were a lot of inflammations, atypical squamous cells of unknown significance, low-grade squamous intraepithelial lesion done as a Pap results just before cone. The positive rate of HPV was 80.0%. There were 5.1% of under-estimated and 6.8% of over-estimated results according to the cone results, and 6.7% of under-estimated and 8.9% of over-estimated according to the hysterectomy results.
Limited accuracy of punch biopsy of the cervix in defining extent and severity of epithelial lesions in women presenting with abnormal Pap smear remains an important clinical problem. Studies correlating the histology diagnosis of biopsy with that of the surgical specimen showed both under- and over-estimations. Biopsy diagnoses that overestimate the grade of cervical intraepithelial neoplasia (CIN) are associated primarily with potential overtreatment. Albeit less frequent, underestimations may have even more serious implications. The greatest concern is that early invasive lesions may be missed and inadvertently treated by an ablative technique [1,2]. Disease relapse in such patients has been described [3]. The risk of undertreatment may cause clinicians to lose confidence in conservative treatments of CIN [4]. Also, nondiagnosis of carcinoma may flaw quality control procedures for cytology [5] and colposcopy [6] as well as clinical studies of preinvasive disease using punch biopsy as an endpoint [7].
Many clinical factors are hypothesized to influence the accuracy of biopsy. In the literature, however, there is little statistical support. This is especially the case for the determinants of the probability of a carcinoma remaining undiagnosed. Most previous studies were based on small series of CIN biopsies and, while inherently unacceptable, the prevalence of missed microinvasive or invasive carcinoma was generally less than 5% with a mean of 1.8% [8,9]. We collected the clinical data of the patients whose punch biopsy results were CIN 3 and tried to correlate the histology diagnosis of biopsy with that of the surgical specimen in our institution.
This study was done through review of medical records of punch biopsy proven CIN 3 patients retrospectively. Histological diagnoses through conization or hysterectomy were used as references. The catchment area at our institution includes the metropolitan area of Incheon and several surrounding health districts of western seaside of Korea. Patients are referred for the management of an abnormal Pap smear and/or histological CIN diagnosed on punch biopsy or endocervical curettage. Patients, who underwent punch biopsy and the result was CIN 3 were enrolled in this study. Colposcopy examination was usually used for biopsy. Electrosurgical conizations were performed usually. The crater is fulgurated with the ball diathermy using a pure coagulation frequency. Even though conization was strongly recommended, some patients underwent hysterectomies without conization without specific reason.
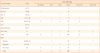
There were 104 patients whose cervical punch biopsies were CIN 3 between 1999 to 2008 in our institution. The age distribution was 42.6±9.9 years old. The median follow-up period was 3.3 years. There were 59 (56.7%) who underwent conization and 45 who did not (Table 1).
Among 59 patients who underwent conization, there were 3 (5.1%) whose cone results were CIN 1, and 2 (3.4%) whose results were CIN 2. These 5 patients did not undergo hysterectomies. There were 51 (86.4%) whose results were CIN 3. Forty-one (80.4%) did not undergo hysterectomy. Among 10 patients who underwent hysterectomy, 8 had no lesion and 1 had CIN 1 lesion. However, 1 had cervical cancer IB2 lesion and underwent adjuvant concurrent chemoradiation therapy. There were 3 (5.1%) whose cone result were cervical cancer IA1. 2 underwent hysterectomy and the results found no lesion and CIN 3 (Table 2).
Every 45 patient who did not undergo conization experienced hysterectomy. Three (6.7%) patients had no lesion and 3 had CIN 2. 35 (77.8%) had CIN 3 and 4 (8.9%) had cervical cancer IA1 (Table 3).
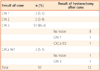
Among 104, 73 (70.2%) got cervical smear before punch biopsies. There were 2 (2.7%) patients with inflammation, 7 (9.6%) with atypical squamous cells of unknown significance, 5 (6.9%) with atypical squamous cells exclude high-grade lesions, 8 (11.0%) with low-grade squamous intraepithelial lesion (LSIL), 46 (63.0%) with high-grade squamous intraepithelial lesion (HSIL), 2 with squamous cell carcinoma and 3 (4.1%) with unsatisfactory. At LSIL group, 1 (1.3%) patient contracted cervical cancer IA1 and at HSIL group, 3 (6.5%) did cervical cancer IA1. Human papillomavirus (HPV) positive rate for the patients were 80% (48/60) (Table 4).
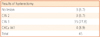
Among 59 patients who underwent cone, 3 (5.1%) patients had the lesions less than CIN 1 and 4 (6.8%) had the lesions of cervical cancers. Among 45 patients who did not, 3 (6.7%) and the lesions less than CIN 1 and 4 (8.9%) had the lesions of cervical cancers (Table 5).
The efficacy of cervical cone biopsy in the diagnosis of CIN was well known [10]. The conization rate of the catchment area at our institution when CIN 3 were found by punch biopsies was 13-71%. It depends on the year the biopsies were done and the age of the patients. The nearer the dates operated were and the younger the patients were, the higher conizations were done [11]. At our 10 year experiences, the rate of conization was 56.7%.
Most previous reports of the accuracy of colposcopically directed biopsy versus cone histology diagnosis have been descriptive evaluations [12,13], or were concerned with the calculation of perfect agreement [14,15], or agreement to within one degree [8], or both procedure were done at the same time prospectively [16]. In fact, the actual clinical significance of biopsy errors varies greatly. Patient age qualified as the strongest independent determinant of nondiagnosis of carcinoma [9]. At our data, the patients' age, however, did not have any impact on the cone or hysterectomy. Partial or total invisibility of the squamocolumnar junction [17,18] and error by the colposcopist in selecting a biopsy site in a large surface lesion [7,12] have often been postulated to explain nondiagnosis of carcinoma by biopsy. The need for multiple or multiquadrant biopsies is controversial [19]. Unfortunately, we did not have the data of colposcopic findings and we could not tell about these issues.
Unconfirmed high-estimated CIN biopsies are less worrisome but more frequent [20]. In previous reports, the frequency varied between zero [18] and 46% [21] with a mean of 16%. Our rate of unconfirmed high-estimated CIN biopsies 5.8% (6/104). A negative diagnosis on cone specimen may be caused by inflammation and wound healing processes induced by biopsy [8,14], removal of the entire lesion [12,15], spontaneous regression between biopsy and conization [12,21], failure to include the involved area in the cone excision specimen [21,22], laboratory errors in cone handling and processing [23], and variability in histopathological diagnosis [12] and grading of CIN [24]. In principle, these factors may account for our own cases. Their actual role, however, remains unclear [25]. There were 7.7% (8/104) microinvasive and invasive squamous carcinoma among the patients whose punch biopsy results were CIN 3. Previous univariate data suggested that the severity of Pap smear correlates positively with nondiagnosis of carcinoma by biopsy [26]. At our data, Pap smear as well as HPV results, however, did not have any impact on the cone or hysterectomy results.
Some limitations of this study should be considered in assessing its results. First, the material was retrospectively obtained from routine clinical records. This caused some important information not to be available. Second, patients were referred from a number of offices. This made it impossible to review the original smear or HPV specimens. Third, colposcopy which was not routinely used might reduce the accuracy of the biopsies. Fourth, several kinds of HPV test method might reduce the power of the results.
Major findings of this study may be summarised as follows: Through conization, 93.2% of the patients whose punch biopsy results were CIN 3 had CIN and did not need hysterectomy, and 6.8% had cervical cancers and might need further treatment. Through hysterectomy, 91.2% had CIN and might undergo overtreatment.
Figures and Tables
Table 4
The final pathology according to the cervical smear and HPV results
CIN, cervical intraepithelial neoplasia; CXCa, cervical cancer; ASCUS, atypical squamous cells of unknown significance; ASC-H, atypical squamous cells exclude high-grade lesions; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade squamous intraepithelial lesion; SCC, squamous cell carcinoma; HPV, human papillomavirus.
Acknowledgments
This work was supported by INHA UNIVERSITY Research Grant and Incheon Medical Association.
References
1. Ang MS, Kaufman RH, Adam E, Riddle G, Irwin JF, Reeves KO, et al. Colposcopically directed biopsy and loop excision of the transformation zone. Comparison of histologic findings. J Reprod Med. 1995. 40:167–170.
2. Baldauf JJ, Dreyfus M, Ritter J, Philippe E. An analysis of the factors involved in the diagnostic accuracy of colposcopically directed biopsy. Acta Obstet Gynecol Scand. 1997. 76:468–473.
3. Prendiville W, Cullimore J, Norman S. Large loop excision of the transformation zone (LLETZ). A new method of management for women with cervical intraepithelial neoplasia. Br J Obstet Gynaecol. 1989. 96:1054–1060.
4. Serafini M, Cordaro C, Montanari E, Falcini F, Bucchi L. Diagnosis and treatment of cervical intraepithelial neoplasia grade 3: a registry-based study in the Romagna region of Italy (1986-1993). Int J Epidemiol. 1999. 28:196–203.
5. Heatley MK, Bury JP. The correlation between the grade of dyskaryosis on cervical smear, grade of cervical intraepithelial neoplasia (CIN) on punch biopsy and the final histological diagnosis on cone biopsies of the cervix. Cytopathology. 1998. 9:93–99.
6. Benedet JL, Anderson GH, Boyes DA. Colposcopic accuracy in the diagnosis of microinvasive and occult invasive carcinoma of the cervix. Obstet Gynecol. 1985. 65:557–562.
7. Buxton EJ, Luesley DM, Shafi MI, Rollason M. Colposcopically directed punch biopsy: a potentially misleading investigation. Br J Obstet Gynaecol. 1991. 98:1273–1276.
8. Barker B, Garcia F, Lozevski J, Warner J, Hatch K. The correlation between colposcopically directed cervical biopsy and loop electrosurgical excision procedure pathology and the effect of time on that agreement. Gynecol Oncol. 2001. 82:22–26.
9. Costa S, Nuzzo MD, Rubino A, Rambelli V, Marinelli M, Santini D, et al. Independent determinants of inaccuracy of colposcopically directed punch biopsy of the cervix. Gynecol Oncol. 2003. 90:57–63.
10. Kim BG, Kim JH, Song ES, Shim SD, Choi YM, Kang SB, et al. The efficacy of cervical cone biopsy in the diagnosis of the cervical intraepithelial neoplasia. Korean J Gynecol Oncol Colposc. 1990. 1:49–57.
11. Song ES. The change of trend on surgical treatment of patients with cervical intraepithelial neoplasia 3 in Incheon and Bucheon area. Korean J Obstet Gynecol. 2005. 48:2330–2335.
12. Denny LA, Soeters R, Dehaeck K, Bloch B. Does colposcopically directed punch biopsy reduce the incidence of negative LLETZ? Br J Obstet Gynaecol. 1995. 102:545–548.
13. Spitzer M, Chernys AE, Seltzer VL. The use of large-loop excision of the transformation zone in an inner-city population. Obstet Gynecol. 1993. 82:731–735.
14. Massad LS, Halperin CJ, Bitterman P. Correlation between colposcopically directed biopsy and cervical loop excision. Gynecol Oncol. 1996. 60:400–403.
15. Vergote IB, Makar AP, Kjørstad KE. Laser excision of the transformation zone as treatment of cervical intraepithelial neoplasia with satisfactory colposcopy. Gynecol Oncol. 1992. 44:235–239.
16. Zuchna C, Hager M, Tringler B, Georgoulopoulos A, Ciresa-Koenig A, Volgger B, et al. Diagnostic accuracy of guided cervical biopsies: a prospective multicenter study comparing the histopathology of simultaneous biopsy and cone specimen. Am J Obstet Gynecol. 2010. 203:321.e1–321.e6.
17. Killackey MA, Jones WB, Lewis JL Jr. Diagnostic conization of the cervix: review of 460 consecutive cases. Obstet Gynecol. 1986. 67:766–770.
18. Chen RJ, Chang DY, Yen ML, Lee EF, Chow SN, Huang SC, et al. Independent clinical factors which correlate with failures in diagnosing early cervical cancer. Gynecol Oncol. 1995. 58:356–361.
19. Burger MP, Hollema H. The reliability of the histologic diagnosis in colposcopically directed biopsies. A plea for LETZ. Int J Gynecol Cancer. 1993. 3:385–390.
20. Kirkup W, Hill AS. The accuracy of colposcopically directed biopsy in patients with suspected intraepithelial neoplasia of the cervix. Br J Obstet Gynaecol. 1980. 87:1–4.
21. Chappatte OA, Byrne DL, Raju KS, Nayagam M, Kenney A. Histological differences between colposcopic-directed biopsy and loop excision of the transformation zone (LETZ): a cause for concern. Gynecol Oncol. 1991. 43:46–50.
22. Howell R, Hammond R, Pryse-Davies J. The histologic reliability of laser cone biopsy of the cervix. Obstet Gynecol. 1991. 77:905–911.
23. Robboy SJ, Bentley RC, Russel P, Anderson MC. Robboy SJ, Anderson MC, Russel P, editors. Cut up: the gross description processing and reporting of specimens. Pathology of the female reproductive tract. 2002. London: Churchill-Livingstone;861–908.
24. Bonardi R, Cecchini S, Grazzini G, Ciatto S. Loop electrosurgical excision procedure of the transformation zone and colposcopically directed punch biopsy in the diagnosis of cervical lesions. Obstet Gynecol. 1992. 80:1020–1022.
25. Chenoy R, Billingham L, Irani S, Rollason TP, Luesley DM, Jordan JA. The effect of directed biopsy on the atypical cervical transformation zone: assessed by digital imaging colposcopy. Br J Obstet Gynaecol. 1996. 103:457–462.
26. Wetrich DW. An analysis of the factors involved in the colposcopic evaluation of 2194 patients with abnormal Papanicolaou smears. Am J Obstet Gynecol. 1986. 154:1339–1349.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download