Abstract
Neurilemmoma is a benign slow-growing nerve sheath neoplasm that is rarely found in the female genital system. To date, thirteen cases of vulvar neurilemmoma have been reported in the world literature. We report here on the first Korean case of vulvar neurilemmoma. A 43-year-old woman presented with a 0.6×0.6 cm sized oval nodule at the left labium minus. Complete excision was done. Microscopically, the mass was a well circumscribed lesion that was alternatively composed of cellular Antoni A and paucicellular Antoni B areas; The Antoni A areas were composed of spindle cells with twisted, buckled nuclei and occasional intranuclear vacuoles, and the spindle cells were arranged in short bundles or fascicles. Immunohistochemically, the spindle cells were positive for S100 protein and negative for desmin. Although it has a very low incidence, neurilemmoma should be considered in the differential diagnosis of a cutaneous or subcutaneous mass in the vulva.
Neurilemmoma is also named neurinoma, schwannoma and Schwann cell tumor. It is generally a solitary, nodular, benign tumor that arises from the neural sheath Schwann cells of the peripheral, cranial or autonomic nerves. The most common locations are the head, neck, upper and lower extremities, posterior mediastinum and retroperitoneum [1]. It rarely affects the female genitalia. To the best of our knowledge, epithelial tumors are the most common tumor in the vulvar region, and mesenchymal tumors comprise less than 10% of them. Neurilemmoma involving vulva is the least common. To date, only thirteen cases of vulvar neurilemmoma have been reported in the literature [2-14]. Here, we report on an additional case of vulvar neurilemmoma arising in the labium minus in a patient without neurofibromatosis.
A 43-year-old Korean woman (gravida 3, para 2) presented with a non-tender palpable small nodule at her left labium minus. The patient reported that she noticed the small nodule in her left vulvar region 2 weeks previously. The size measured 0.6 × 0.5 × 0.4 cm. Her previous menstrual history was regular. On general examination, she was found to be of average build and there were no clinical signs indicative of neurofibromatosis 1 and 2. On gynecologic examination, there was no abnormality except the small nodule. A simple excision of the nodule was performed under local anesthesia. After 6 months, she has had no evidence of recurrence or symptoms.
The excised nodule was situated in the lower part of the dermis and it was a well-circumscribed encapsulated lobular nodule for the architecture (Fig. 1A). Nuclear palisadings that formed Verocay bodies were found in the Antoni A area, and in the Antoni B areas, the cells were loosely arranged within a slightly myxoid stroma (Fig. 1B). The tumor cells were spindle shaped with nuclear buckling. The nucleoli were not prominent, and mitosis or necrosis was not seen. Perivascular hyalinization was also noted. Immunohistochemically, the spindle cells were strongly positive for S100 protein (polyclonal; 1:1200 dilution, Zymed, San Francisco, CA, USA), and they were negative for pancytokeratin (AE1/AE3; Dako, Glostrup, Denmark, prediluted), desmin (D33; Dako, 1:100 dilution) and smooth muscle actin (1A4; Dako, 1:100 dilution). Neurilemmoma arising in the labium minus was diagnosed.
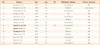
Neurilemmoma is an encapsulated, well circumscribed tumor that is classically characterized by cellular Antoni A and paucicellular Antoni B areas. The conventional type is the most common and the plexiform type with multinodular growth and cellular variants or ancient variants, i.e., degenerative changes can also be found [1]. Neurilemmoma is a tumor that arises from the Schwann cells of the nerve sheath, and it occurs throughout the whole body. Neurilemmoma can arise from neurofibromatosis or it can occur sporadically. Of all the neurogenic tumors, about half are found in the head and neck region. The origin of neurilemmoma is most commonly associated with a nerve trunk, and the clinical symptoms depend on the nerve of origin. Vulvar neurilemmoma is a slow-growing well encapsulated benign tumor. After reviewing the previous literature about vulvar neurilemmoma, the vulvar neurilemmoma presents with nonspecific symptoms that are indistinguishable from those of other cutaneous lesions; the lesions had presented for many years with a slow increase in size [2-14]. Due to the site of occurrence, sitting and walking can be affected, but most of the vulvar neurilemmoma are discovered by chance. Histologically, the conventional type of neurilemmoma is the most common type in the vulvar area. It was interesting in that plexiform (multinodular) neurilemmoma is one of the least common histologic variants of neurilemmomas, but five cases of plexiform variants and a case of ancient variant have been found among the reported cases of vulvar neurilemmoma [2,4,8,11-13]. The age at presentation of a vulvar neurilemmoma has varied from 5 to 84 years. The size of vulvar neurilemmoma ranged from 0.6 cm up to 15 cm (mean, 4.3 cm). Most of the vulvar neurilemmoma occurred in the labium except for four cases of clitoral neurilemmoma [3,9,12,13]. None of the reported patients with vulvar neurilemmoma were associated with neurofibromatosis, and even for the patients with plexiform neurilemmoma. These findings are summarized in Table 1.
The nature of vulvar neurilemmoma has not yet been properly characterized in the previously reported cases including the present one. In general, neurilemmoma has a true capsule composed of epineurium, which makes the nerve be displaced to the periphery by the mass when large nerves are the sites of origin. This finding is helpful, but it is not found in neurilemmoma of the small nerves. Growth of neurilemmoma within the epineurium creates encapsulation, which makes total resection possible. Complete surgical excision is the treatment of choice for vulvar neurilemmoma, the same as for those at other sites. The prognosis is excellent. The only reported case of vulvar neurilemmoma of the plexiform type recurred twice [4]. The patient was alive and well three years after the second resection. Unlike plexiform neurofibroma, which occurs almost exclusively in patients with NF1, the large majority of plexiform neurilemmoma are sporadic tumors in the vulva [1]. Malignant progression is extremely rare.
Although rare, neurilemmoma should be considered in the differential diagnosis of vulvar masses.
Figures and Tables
References
1. Weiss SW, Goldblum JR. Weiss SW, Goldblum JR, editors. Benign tumors of peripheral nerves. Enzinger and Weiss's soft tissue tumors. 2008. 5th ed. Philadelphia (PA): Mosby;825–901.
2. Fong KL, Bouwer H, Baranyai J, Jones RW. Ancient schwannoma of the vulva. Obstet Gynecol. 2009. 113:510–512.
3. Huang HJ, Yamabe T, Tagawa H. A solitary neurilemmoma of the clitoris. Gynecol Oncol. 1983. 15:103–110.
4. Woodruff JM, Marshall ML, Godwin TA, Funkhouser JW, Thompson NJ, Erlandson RA. Plexiform (multinodular) schwannoma. A tumor simulating the plexiform neurofibroma. Am J Surg Pathol. 1983. 7:691–697.
5. Yamashita Y, Yamada T, Ueki K, Ueki M, Sugimoto O. A case of vulvar schwannoma. J Obstet Gynaecol Res. 1996. 22:31–34.
6. Hanafy A, Lee RM, Peterson CM. Schwannoma presenting as a Bartholin's gland abscess
. Aust N Z J Obstet Gynaecol. 1997. 37:483–484.
7. Quesada G, Solera JC, Sanchez-Baartolome J, Vazquez F, Lopez-Garcia L. Benign schwannoma of the vulva: a case report. J Gynecol Surg. 1998. 14:195–198.
8. Santos LD, Currie BG, Killingsworth MC. Case report: plexiform schwannoma of the vulva. Pathology. 2001. 33:526–531.
9. Llaneza P, Fresno F, Ferrer J. Schwannoma of the clitoris. Acta Obstet Gynecol Scand. 2002. 81:471–472.
10. Fujimoto E, Onishi Y, Tajima S, Okura T. Vulvar schwannoma. Rinsho Derma. 2004. 46:548–549.
11. Agaram NP, Prakash S, Antonescu CR. Deep-seated plexiform schwannoma: a pathologic study of 16 cases and comparative analysis with the superficial variety. Am J Surg Pathol. 2005. 29:1042–1048.
12. Chuang WY, Yeh CJ, Jung SM, Hsueh S. Plexiform schwannoma of the clitoris. APMIS. 2007. 115:889–890.
13. Yegane RA, Alaee MS, Khanicheh E. Congenital plexiform schwannoma of the clitoris. Saudi Med J. 2008. 29:600–602.
14. Das S, Kalyani R, Kumar ML. Vulvar schwannoma: a cytological diagnosis. J Cytol. 2008. 25:108–110.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download