Abstract
Puerperal genital hematomas are uncommon causes of postpartum hemorrhage but can be a cause of serious morbidity and even maternal death. When puerperal genital hematomas are clinically occult despite significant blood loss or found as delayed postpartum hemorrhage, there is a high risk of shock. We report a case with shock accompanied by rupture of progressive retroperitoneal hematoma through left upper vaginal wall on 2nd postpartum day.
Postpartum hemorrhage (PPH) is the most significant cause of maternal morbidity and mortality worldwide [1]. PPH is defined as an estimated blood loss in excess of 500 mL following a vaginal birth or a blood loss of greater than 1,000 mL following cesarean birth [2]. PPH is classified as primary and secondary. Primary PPH occurs within 24 hours of delivery and secondary PPH after 24 hours and within 6-12 weeks post-partum.
Puerperal genital hematomas are uncommon causes of PPH but can be a cause of serious morbidity and even maternal death [3]. The incidence of puerperal genital hematoma ranges from 1/300 to 1/1,400. Puerperal genital hematomas can be classified into vulvar, vulvovaginal, paravaginal, retroperitoneal or supravaginal type according to location [4]. When puerperal genital hematomas are clinically occult despite significant blood loss or are found as delayed postpartum hemorrhage, there is a high risk of shock. A close monitoring and prompt treatment should be required.
We report a case with shock accompanied by rupture of progressive retroperitoneal hematoma through left upper vaginal wall on postpartum 2nd day. It was suggested to be originated from injury of left vaginal artery.
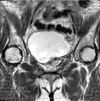
A 33-year-old woman (gravida 2, para 2) presented at emergency room with moderate left perineal pain and left lower quadrant abdominal pain. The patient spontaneously delivered a large baby (4.2 kg) after induction of labor two days ago. Physical examination showed tenderness and rebound tenderness on left lower abdominal area. The uterus was firm and the fundus was below umbilicus. The vaginal bleeding or laceration was not found on first speculum examination. The vital signs of the patient were as follows: blood pressure of 90/70 mm Hg, heart rate of 102 per minute and body temperature of 36.9℃. A transvaginal sonography revealed displaced uterus to the right and a large amount of blood clot in left pelvic cavity and we could not find left adnexae. Laboratory testing showed the following: hemoglobin (Hb) 9.4 g/dL, hematocrit (Hct) 27.6%, prothrombin time-internationalized ratio (PT-international normalized ratio) 1.14 and platelet count 193,000/µL. A computed tomographic (CT) scan demonstrated a huge hematoma in lower abdomen, pelvis and retroperitoneum which was presumed to be placed in left pararectal space and extravasation of intravenous contrast media from a branch of left vaginal artery (Fig. 1). About an hour after the CT scan, left perineal pain was abruptly aggravated and the patient became hemodynamically unstable: blood pressure was 70/50 mm Hg and pulse rate was above 120-130 per minute. The rupture of left upper vaginal wall and severe vaginal bleeding through the opening canal between pelvic cavity and vaginal lumen were found on subsequent speculum examination. Hb and Hct levels were decreased to 5.7 g/dL and 17.1%, respectively. The patient was promptly transferred to operation room for emergency operation. During the operation, we removed about 3,500 mL of hematoma but could not identify the exact focus of bleeding. The opening canal between left upper vaginal wall and left pararectal retroperitoneal cavity was found. Postpartum hysterectomy and repair of pelvic floor including vaginal wall were performed. Blood products were all administered during operation as follows; 20 units of packed red blood cells, 12 units of fresh frozen plasma, 10 units of platelet concentrate. The postoperative course was uneventful. However, the patient felt fatigue easily after short walking. The patient had no specific finding on pelvic magnetic resonance imaging after 3 weeks from operation (Fig. 2).
Retroperitoneal puerperal hematoma which occurrs secondary to lacerations of the uterine artery or vessels of the broad ligament is the least common hematoma encountered with an estimated incidence of 1/3500 to 1/20,000 [5,6]. However, it could have fatal progress if the diagnosis is delayed. Thus, prompt diagnosis and treatment must be carried out.
Only 40% of women who develop PPH have an identifiable risk factor. Risk factors for injuring the pelvic vasculature and hematoma formation include episiotomy, nulliparity, operative vaginal delivery, breech delivery, delivery of multiples, prolonged second stage labor, birthweight above 4,000 g, hereditary clotting deficiencies, vulvar varicosities, and pre-eclampsia [4]. In our case, the patient spontaneously delivered a large baby (4.2 kg).
The treatment of puerperal genital hematomas is variable according to size, location and severity of patient. According to algorithm by Bienstman-Pailleux et al. [7], we could first consider pelvic arterial embolization. Pelvic arterial embolization has become a reliable and safe alternative procedure for postpartum hemorrhage only when the patient is hemodynamically stable and the embolization unit is located close to the delivery room [8,9]. However, our patient went into shock within an hour and we decided to perform exploratory laparotomy.
Our case is similar to the case described by Chia and Huang [10]. The patient had a large retroperitoneal hematoma with left posterior vaginal wall laceration after emergency cesarean section. The large laceration over posterior vaginal wall extended from left uterosacral ligament towards the left rectovaginal septum. The authors sutured the laceration site of vaginal wall and packed the area with gel foam to achieve hemostasis. In our case, we found an opening canal connected between vaginal lumen and left pelvic cavity. We had concern whether the patient could have gait disturbance due to left pelvic floor injury and recommended physiotherapy. However, the patient had no problem to perform her daily activities after surgery. Simple vaginal suture and hemostasis were sufficient to treat an opening canal between pelvic cavity and vaginal lumen, formed by large retroperitoneal hematoma.
In conclusion, this case shows that concealed retroperitoneal hematoma after delivering a large baby can cause fulminant clinical course and prompt evaluation or treatment is required. In case with an opening canal between pelvic cavity and vaginal lumen, primary repair of vaginal opening site after bleeding control seems to be suitable.
Figures and Tables
References
1. Combs CA, Murphy EL, Laros RK Jr. Factors associated with postpartum hemorrhage with vaginal birth. Obstet Gynecol. 1991. 77:69–76.
2. Ramanathan G, Arulkumaran S. Postpartum hemorrhage. J Obstet Gynaecol Can. 2006. 28:967–973.
3. Lee NK, Kim S, Lee JW, Sol YL, Kim CW, Kim HS, et al. Postpartum hemorrhage: clinical and radiologic aspects. Eur J Radiol. 2010. 74:50–59.
4. Mirza FG, Gaddipati S. Obstetric emergencies. Semin Perinatol. 2009. 33:97–103.
5. Fliegner JR. Postpartum broad ligament haematomas. J Obstet Gynaecol Br Commonw. 1971. 78:184–189.
6. Sheikh GN. Perinatal genital hematomas. Obstet Gynecol. 1971. 38:571–575.
7. Bienstman-Pailleux J, Huissoud C, Dubernard G, Rudigoz RC. Management of puerperal hematomas. J Gynecol Obstet Biol Reprod (Paris). 2009. 38:203–208.
8. Doumouchtsis SK, Papageorghiou AT, Arulkumaran S. Systematic review of conservative management of postpartum hemorrhage: what to do when medical treatment fails. Obstet Gynecol Surv. 2007. 62:540–547.
9. Sentilhes L, Gromez A, Clavier E, Resch B, Verspyck E, Marpeau L. Predictors of failed pelvic arterial embolization for severe postpartum hemorrhage. Obstet Gynecol. 2009. 113:992–999.
10. Chia CC, Huang SC. Postpartum hemorrhage of genital tract origin. Taiwan J Obstet Gynecol. 2010. 49:513–514.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download