Abstract
Umbilical cord entanglement has been reported to occur in monoamniotic twins. However, it can occur in diamnionic twins due to rupture of the intertwin-dividing membrane, and is a cause for concern. A 31-year-old nullipara visited our hospital at 28+3 weeks gestation. A monochorionic diamniotic twin gestation was diagnosed ultrasonographically by visualizing a thin intertwin-dividing membrane and a single placenta. A cesarean section was performed at 35+3 weeks gestation and concordant twin fetuses with entangled umbilical cords were delivered. Gross examination revealed a single placenta with a ruptured dividing membrane. Our case, along with the other cases, confirms that antepartum rupture of an intertwin-dividing membrane is a clinical condition that should be considered in all cases of monochorionic diamniotic twin. A careful inspection of the dividing membrane and each cord insertion site should be performed. Once the dividing membrane cannot be easily visualized, the possibility of antepartum rupture should be suspected.
The perinatal morbidity and mortality rates associated with twin gestations are higher than singleton gestations [1]. Monochorionic twins have a perinatal mortality rate nearly twice as high as dichorionic twins (2.8% vs. 1.6%) and 4 times as high as singletons (2.8% vs. 0.7%) [2,3]. This risk may be secondary to prematurity, growth restriction, congenital anomalies, vascular anastomosis, and most commonly, umbilical cord entanglement. Umbilical cord entanglement has been reported to occur in as many as 70% of monoamniotic twins [4]. However, umbilical cord entanglement can occur in diamnionic twins due to rupture of the intertwin-dividing membrane. Although umbilical cord entanglement in diamnionic twins is a rare condition, it is a cause for concern.
A 31-year-old nullipara was transferred to our hospital for overt diabetes mellitus at 28+3 weeks gestation. She had a twin pregnancy. Her blood glucose was controlled within the normal range with insulin.
A monochorionic diamniotic twin gestation was diagnosed ultrasonographically by visualizing a thin intertwin-dividing membrane and a single placenta. The amniotic fluid volume was normal and equally distributed between the two sacs with concordant growth for 28+3 weeks gestation. During the subsequent follow-up scan at 30+6 weeks gestation, there was normal interval growth for both twins with a normal amniotic fluid volume. The intertwin-dividing membrane was visualized, although with some difficulty, and appeared not to be connected to a single line with minimal fluttering. She was noted to have bilateral pitting edema of the lower extremities.
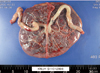
No invasive intrauterine procedures, including amniocentesis, were performed during pregnancy. At 34+3 weeks gestation, her blood pressure was 134/80 mm Hg and mild proteinuria was checked. A cesarean section was performed at 35+3 weeks gestation due to uncontrolled blood pressure and according to the request of patient; concordant twin fetuses with entangled umbilical cords were delivered. There was no deceleration in the fetal heart rates before delivery. Twin A weighed 2,700 g and had Apgar scores of 6 at 1 minute and 8 at 5 minutes. Twin B weighed 2,530 g and had Apgar scores of 4 at 1 minute and 7 at 5 minutes. At the time of delivery, we ruptured amniotic membrane and when we attempted to cut the cord of twin A we noticed that the umbilical cords were entangled and the intertwin-dividing membrane was already ruptured before operation. The cords were entangled without true knots for a distance of 8 cm. Gross examination of the placenta revealed a single placenta with a ruptured two layes of dividing membrane, which was present along the middle surface. The cords were inserted separately, but nearly adherent (Figs. 1, 2). The histopathologic examination confirmed the diagnosis of monochorionic, diamniotic placentation with artery-to-artery anastomosis.
The babies were admitted to the neonatal intensive care unit due to decreased muscle tone and poor oral intake. Electroencephalography revealed moderate cerebral dysfunction; however, brain ultrasonography and magnetic resonance imaging did not show any defects and their oral intake and activity were clinically improved, so they were discharged on post-operative day 31. Thereafter, their course and neurologic development were uneventful.
We report a case involving an intrauterine change in the diamniotic environment to a monoamniotic environment, resulting from antepartum rupture of the intertwin-dividing membrane. This change from double cavities to a single cavity resulted in cord entanglement, which caused major neonatal morbidity in the form of severe hypoxic ischemic encephalopathy. Seventeen such cases have been reported, six of which underwent invasive intrauterine procedures, including amniocentesis and laser ablation of the vascular anastomosis [5]. In our case, as in some other reports, the etiology for the antepartum rupture of the dividing membrane was not clear, although the proximity of the cords and the rubbing with fetal movement may have caused rupture of the intertwin-dividing membrane. We thus suggest more cautious antenatal examination regarding twin cord insertions with the attendant risk of membrane rupture or cord entanglement.
The most important concern of antepartum disruption of the intertwin-dividing membrane is cord entanglement. In a case report and review, Nasrallah and Faden [5] noted that this complication was reported in 60% of reported cases (9 of 15), which approximates the risk in true monoamniotic twins [6-9]. If the possibility of cord entanglement is suspected, an earlier delivery by cesarean section would prevent fetal heart rate abnormalities and the major consequences, although in our case there were no fetal heart rate decelerations before delivery.
Furthermore, antepartum disruption of the intertwin-dividing membrane may also result in preterm labor and delivery and amniotic band syndrome [10].
Thus, to minimize these shortcomings in the diagnosis of actual amnionicity, it is very important to visualize multiple sections of the membrane along with an attempt to visualize the whole course of the membrane as much as possible. Cord entanglement is not only diagnosed in monoamniotic twins, but has also been diagnosed in a case of twins with an intact intertwin-dividing membrane at the time of delivery [11].
The difficulties in diagnosis of umbilical cord entanglement can be summarized as follows. First, the gravida was referred in the third trimester, so we could not perform a more detailed ultrasound scan, which is generally performing in the second trimester. Then, it was hard to find the umbilical cord insertion site, so that we overlooked the close proximity of the cords. Second, although we identified the intertwin-dividing membrane at the first visit, we could not observe the membrane continuously during the subsequent follow-up scan. At 30+6 weeks gestation, the intertwin-dividing membrane was visualized with some difficulty and had a fluttering characteristic, but we did not suspect the possibility of membrane rupture, and did not visualize multiple sections of the membrane.
Our case with the other reported cases confirms that the antepartum rupture of an intertwin-dividing membrane is a condition that should be kept in mind in all cases of monochorionic, diamniotic twin gestations, especially after any invasive intrauterine procedure. For this reason, a careful inspection of the dividing membrane and each cord insertion site should be performed at every follow-up examination. Once the dividing membrane cannot be easily visualized, the possibility of antepartum rupture should be suspected, thus indicating a modification in the method and frequency of the prenatal fetal well-being follow-up, as well as the time and mode of delivery.
Figures and Tables
References
1. Benirschke K. Twin placenta in perinatal mortality. N Y State J Med. 1961. 61:1499–1508.
2. D'Alton ME, Simpson LL. Syndromes in twins. Semin Perinatol. 1995. 19:375–386.
3. Sebire NJ, Snijders RJ, Hughes K, Sepulveda W, Nicolaides KH. The hidden mortality of monochorionic twin pregnancies. Br J Obstet Gynaecol. 1997. 104:1203–1207.
4. Lee CY. Management of monoamniotic twins diagnosed antenatally by ultrasound. Am J Gynecol Health. 1992. 6:25–27.
5. Nasrallah FK, Faden YA. Antepartum rupture of the intertwin-dividing membrane in monochorionic diamniotic twins: a case report and review of the literature. Prenat Diagn. 2005. 25:856–860.
6. Gilbert WM, Davis SE, Kaplan C, Pretorius D, Merritt TA, Benirschke K. Morbidity associated with prenatal disruption of the dividing membrane in twin gestations. Obstet Gynecol. 1991. 78:623–630.
7. Krause HG, Goh JT. Cord entanglement in monochorionic diamniotic twins. Aust N Z J Obstet Gynaecol. 1998. 38:341–342.
8. Megory E, Weiner E, Shalev E, Ohel G. Pseudomonoamniotic twins with cord entanglement following genetic funipuncture. Obstet Gynecol. 1991. 78:915–917.
9. De Lia JE, Worthington D. Intrauterine sling with umbilical cord entanglement in diamniotic twins. Ultrasound Obstet Gynecol. 2000. 15:447.
10. Chen SE, Trupin L, Trupin S. Antepartum rupture of diamniotic membranes separating monozygotic twins. A case report. J Reprod Med. 1994. 39:67–70.
11. Chmait RH, Aghajanian P, Kontopoulos EV, Quintero RA. Prenatal diagnosis of spontaneous septostomy of the dividing membranes in complicated monochorionic diamniotic multiple gestations. J Ultrasound Med. 2009. 28:663–668.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download