Abstract
Objective
To evaluate the clinical significance of soluble fms-like tyrosine kinase1 (sFlt-1), soluble endoglin (sEng) and placental growth factor (PlGF) in preeclampsia.
Methods
We conducted a case-control study analyzing serum levels of sFlt-1, sEng and PlGF in women with preeclampsia (n=30) and normal pregnancy (n=30) in the third trimester. We calculated the sensitivity, specificity, positive, and negative predictive values of each peptide in diagnosing preeclampsia.
Results
The mean serum level of sFlt-1 and sEng in women with preeclampsia was significantly higher than normal pregnancy. But the mean serum level of PIGF had no significant difference between two groups. The cut-off values of sFlt-1 and sEng showing differential significance were 26.3 ng/mL and 21.1 ng/mL each. Then the sensitivity, specificity, positive predictive value, negative predictive value was all over 80%. Serum levels of sFlt-1 and sEng were not significantly different between intrauterine growth restriction (IUGR) and non-IUGR group among preeclamptic women.
Preeclampsia is a leading cause of maternal and neonatal morbidity and mortality [1,2]. The incidence of preeclampsia ranges between 2% and 7% in healthy nulliparous women [3,4]. The rate is substantially higher in women with twin gestation (14%) [5] and those with previous preeclampsia (18%) [6]. The diagnosis is based on the onset of hypertension and proteinuria, usually after 20 weeks of gestation [7,8]. However, because the onset of hypertension and proteinuria can be variable and the disorder is without clinically apparent pathognomonic signs or symptoms, the diagnosis can be difficult and time-consuming, and often result indelaying appropriate care. Although abnormal placental development, systemic endothelial dysfunction and imbalance of level of maternal circulating angiogenic factors have been suggested to pathogenesis of preeclampsia [9], the etiology of hypertensive disease during pregnancy is unclear.
Recently, it has been shown that two placental anti-angiogenic peptides, soluble fms-like tyrosine kinase1 (sFlt-1) and soluble endoglin (sEng), and placental growth factor (PlGF) contribute to the pathogenesis of preeclampsia [10-13]. sFlt-1, a splice variant of the vascular endothelial growth factor (VEGF) receptor, Flt1 lacking the transmembrane and cytoplasmic domains, acts as a potent VEGF and PlGF antagonist. It is produced by various tissues, including the placenta. Exogenous administration of sFlt-1 has been shown to cause hypertension, proteinuria and glomerular endotheliosis (a pathological renal lesion seen in preeclampsia) in rats [10]. In human, the rise in circulating sFlt-1 in preeclamptic women has been shown at the time of the diagnosis specially 5 weeks before onset [11], suggesting that this peptide may play a causative role.
Endoglin, a coreceptor for transforming growth factor (TGF)-β1 and β3, has been shown to be up-regulated in the placenta in preeclampsia leading to increased secretion of the soluble form into maternal circulation [12]. In addition, sEngin the presence of elevated sFlt-1, has been shown to cause hemolysis, hepatic ischemia and necrosis, extensive vascular damage of the placenta including infarction at the maternal-fetal junction, as well as signs of severe maternal vascular damage in rats [12].
PlGF is a 45-to 50-kd dimeric glycoprotein with 53% sequence identity to VEGF. Alternative splicing of the primary PlGF transcript results in two messenger RNAs (mRNAs) that correspond to PlGF-1 and PlGF-2 protein isoforms. PlGF-2 differs only in the addition of 21 basic amino acids at the carboxyl terminus that confer heparin binding. PlGF has in vivo angiogenic activity in rabbit cornea and chick chorioallantoic membrane assays, with effects that are comparable to the effects of VEGF and basic fibroblast growth factor. The decreased PlGF production results in abnormalities of placental angiogenesis through direct and indirect effects on other vascular growth factors [13].
For the clinical utility of these factors in diagnosing preeclampsia, we performed this study to evaluate the sensitivity, specificity, positive and negative predictive valueof sFlt-1, sEng and PlGF in patients with preeclampsia.
We performed a case-control study measuring serum sFlt-1, sEng and PlGF in consenting pregnant women with hypertension presenting to labor and delivery unit of St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea from January 2005 to December 2007 in the third trimester. The Committee on Clinical Research at St. Mary's Hospital approved the study (SCMC07BR005). Preeclampsia was diagnosed according to the diagnostic criteria outlined by the American College of Obstetrics and Gynecology (ACOG) practice bulletin [7]. For proteinuria, either a ≥ 1+ dipstick or protein ≥ 0.3 g in a 24-hour urine specimen was used.
Severe preeclampsia was defined if 1 or more the following was present: 1) blood pressure of 160 mm Hg or greater systolic or greater than 110 mm Hg diastolic on 2 occasions at least 6 hours apart while on bed rest; 2) proteinuria of 5 g or higher in a 24-hour urine collection or greater than positive 3 on 2 random urine samples collected at least 4 hours apart; 3) oliguria of less than 500 mL in 24 hours; 4) cerebral or visual disturbance; 5) pulmonary edema or cyanosis; 6) epigastric or right upper-quadrant pain; 7) impaired liver function; 8) thrombocytopenia; or 9) fetal growth restriction [7].
Pregnant women without hypertension, proteinuria or underlying medical conditions were recruited as controls.
The serum samples were stored at -70℃ in a freezer before use. Assays were performed by personnel who were unaware of the outcome of the pregnancy. Enzyme-linked immunosorbent assays (ELISA) for sFlt-1, sEng and PlGF were performed with commercially-available kits, as previously described (R&D Systems Inc., Minneapolis, MN, USA). Briefly, various samples for ELISA measurement were diluted in respective Calibrator Diluent. After adding Assay Diluent and the diluted sample in a 96 well plate precoated with captured antibodies directed against human sFlt1, human sEng or PlGF, the plates were incubated for two hours. Then, the wells were washed four times in wash buffer and incubated with secondary polyclonal antibody against sFlt-1, sEng or PlGF conjugated to horseradish peroxidase for an additional two hours. The plates were then washed four times in wash buffer. Substrate solution containing hydrogen peroxide and tetramethylbenzadine were added to each well and incubated for 30 minutes under protection from light. Stop solution was added to each well. The optical density was then determined by subtracting readings at 540 nm from the reading at 450 nm. All assays were performed in duplicate, and the protein levels were calculated using a standard curve derived from a known concentration of respective recombinant proteins. The minimum detectable doses in the assay for sFlt-1, sEng, and PlGF were 3.5, 7, and 7 pg/mL respectively, with intra-assay and inter-assay coeffieients of variation of 3.7% and 5.2% for sFlt-1, 3.6% and 6.2% for endoglin, and 3.6%, and 10.9% for PlGF.
The data were analyzed using student t-test. Receiver operator characteristic (ROC) curve was drawn and a full analysis performed to detect the highest sensitivity, specificity, positive and negative-predictive valueas appropriate using the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
Thirty women with preeclampsia were recruited for the study. In addition, thirty women with normal pregnancy were used as controls. Basic clinical and demographic information is shown in Table 1. There were no significant differences between the groups in terms of maternal age, body mass index or parity at enrollment. Gestational age and birth weight percentile had significant differences between two groups. The women with preeclampsia had significantly higher systolic (P<0.001) and diastolic (P<0.001) blood pressure than the control group. Twenty-two of 30 patients with preeclampsia met the criteria for severe disease as defined by ACOG [7]. One of the 22 patients had HELLP syndrome (hemolysis, elevated liver enzymes and low platelet count). Fifteen women with preeclampsia had intrauterine growth restricted (IUGR) babies as defined by birth weight less than 10% for gestational age. The mean serum value of sFlt-1 in women with preeclampsia was significantly higher than normal pregnancy (58.7 ± 39.1 ng/mL vs. 16.0 ± 0.8 ng/mL, P<0.01) (Fig. 1).
Similarly, the mean serum level of sEng was significantly higher in women with preeclampsia than the control group (67.7 ± 36.3 ng/mL vs. 13.7 ± 8.9 ng/mL, P<0.01) (Fig. 2).
The mean serum level of PlGF had no significant difference between two groups (Fig. 3).
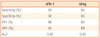
ROC curves were plotted for sFlt-1 and sEng (Fig. 4). The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the ROC curve for sFlt-1 and sEng in women with preeclampsia are shown in Table 2. The serum sFlt-1 level of 26.3 ng/mL had the best sensitivity and specificity with the highest PPV and the lowest NPV (83%, 90%, 89%, and 84%, respectively) in differentiating women with preeclampsia from normal pregnancy. The area under the ROC curve was ± 0.901 with SE of 0.04 (P<0.01). For sEng, the serum level of 21.1 ng/mL, had bestsensitivity and specificity with PPV and NPV (90%, 83%, 84%, and 89%, respectively) in differentiating women with preeclampsia from those with normal pregnancy. The area under the ROC curve was 0.924 with standard error of 0.042 (P<0.01).
Both serum levels of sFlt-1 and sEng were not significantly different in group with IUGR babies when compared with that of group with non IUGR babies among preeclamptic women (sFlt-1, 80.4 ± 86.8 ng/mL vs. 45.7 ± 28.9 ng/mL, P<0.28; sEng, 80.4 ± 32.3 ng/mL vs. 51.2 ± 31.7 ng/mL, P<0.43) (Table 3).
Hypertension complicates approximately 7% to 10% of all pregnancies and is associated with significant maternal, fetal and neonatal morbidity and mortality [3]. Although preeclampsia/eclampsia presents the greatest risk to the mother and her fetus, correctly identifying women with preeclampsia in early stage can be challenging because the disorder is not associated with clinically apparent pathognomonic signs and symptoms. One study reported that 19% of women with eclampsia did not have proteinuria [14]. In a similar study, Douglas and Redman [15] showed that 10% of women with eclampsia did not have hypertension or proteinuria. The main reason for not having a reliable biomarker for the diagnosis of preeclampsia would bethe lack of understanding of the etiology for preeclampsia. However, recently it has been demonstrated that two anti-angiogenic peptides, sFlt-1 and sEng, and P1GFseem to play a critical role in the pathogenesis of preeclampsia. Consistent with published reports, our data showed that sFlt-1 and sEng are significantly elevated in women with preeclampsia. However, PlGF is not significantly changed in preeclampsia and control groups. The analysis on our ROC curves showed that both sFlt-1 and sEng are excellent markers for diagnosing patients with preeclampsia from those with normal pregnancy (Fig. 4). There was a good correlation between these serum markers. Serum sFlt-1 demonstrated a wider distribution in women with preeclampsia and normal pregnancy than sEng (Fig. 1). Thus, if this finding is consistent with further studies, it is possible that sEng may be a better potential candidate for the diagnostic biomarker for preeclampsia compared to sFlt-1.
The serum levels of these anti-angiogenic peptides may correlate better with various perinatal outcomes than blood pressure or 24-hour urine protein. In our study, fifteen women (50%) with preeclampsia had intrauterine growth restricted babies. But our study did not demonstrate that serum levels of these antiangiogenic peptides may correlate with intrauterine growth restriction (Table 3). If the elevated levels of these anti-angiogenic peptides can better predict adverse maternal and/or fetal outcome, it is possible that we may replace urinary protein with serum levels of these peptides for the diagnosis and immediate proper management of patients with preeclampsia.
There are some limitations in this study worth noting. Although we were able to achieve high statistical significance in our results, small sample size makes these findings preliminary. In next critical step to examine the clinical significance of sFlt-1 and sEng in preeclampsia, a larger scale study is warranted.
Another limitation was that we were not able to perform gestational-age-matched analysis. The gestational age at the time of the sampling was much later for control population than those with preeclampsia (38.5 ± 3.1 weeks vs. 33.9 ± 3.5 weeks, P<0.05). It has been reported previously that the serum levels of both sFlt-1 and sEng rise in normal pregnant population with increasing gestational age [11]. Because the serum levels of our control group were measured later in gestation, we believe that this would have biased the data against our findings. Nevertheless, our data show that the serum levels of these anti-angiogenic factors are higher in women with preeclampsia. Further study with large sample size to characterize the variation of these factors in normal pregnancy and preeclampsia depending on different gestational ages would be needed.
It would be more worth studying to confirm prospective cohort study for longer gestational period.
Because the serum levels of these markers rise approximately 5 weeks before the onset of the symptoms [12], increased serum levels of these factors on the setting of labile blood pressure or equivocal proteinuria may identify patients who would develop the full symptoms and signs of preeclampsia shortly after. Possible diagnostic or screening serum markers would allow early diagnosis, proper surveillance, and prompt medical intervention in women with preeclampsia.
Our data support that measuring serum levels of sFlt-1 and sEng may be clinically useful in diagnosis of preeclampsia. But the serum levels of these factors may not predict poor perinatal outcomes. We hope that this will be contributed to establishing these anti-angiogenic markers as reliable diagnostic biomarkers of preeclampsia.
Figures and Tables
Fig. 1
Serum levels of soluble fms-like tyrosine kinase (sFlt)-1 in women with preeclampsia. P<0.01 by t-test. Upper line of the box: mean ± standard deviation (SD). Lower line of the box: mean-SD. Bold line in the box: mean. Upper line above the box: maximum level. Lower line below the box: minimum level. The mean serum level of sFlt-1 in women with preeclampsia was significantly higher than that of the normal group (58.7 ± 39.1 ng/mL vs. 16.0 ± 9.8 ng/mL).

Fig. 2
Serum levels of soluble endoglin (sEng) in women with preeclampsia. P<0.01 by t-test. Upper line of the box: mean ± standard deviation (SD). Lower line of the box: mean-SD. Bold line in the box: mean. Upper line above the box: maximum level. Lower line below the box: minimum level. The mean serum level of sEng in women with preeclampsia was significantly higher than that of the normal group (67.7 ± 36.3 ng/mL vs. 13.7 ± 8.9 ng/mL).

Fig. 3
Serum levels of placental growth factor (PlGF) in women with preeclampsia. P=0.883 by t-test. Upper line of the box: mean ± standard deviation (SD). Lower line of the box: mean-SD. Bold line in the box: mean. Upper line above the box: maximum level. Lower line below the box: minimum level. The mean serum level of PlGF in women with preeclampsia was not significantly different between both groups (144.7 ± 91.6 ng/mL vs. 134.9 ± 84.9 ng/mL).

Fig. 4
Receiver operator characteristic curves of serum sFlt-1 and sEng for diagnosing preeclampsia. sEng, soluble endoglin; sFlt-1, soluble fms-like tyrosine kinase 1. sFlt-1 and sEng were excellent markers for diagnosing patients with preeclampsia from those with normal pregnancy. Cut-off value of sFlt-1 is 26.3 ng/mL and sEng is 21.1 ng/mL.

Acknowledgments
The authors wish to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2007.
References
1. Walker JJ. Pre-eclampsia. Lancet. 2000. 356:1260–1265.
2. Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005. 308:1592–1594.
3. Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, et al. Calcium for Preeclampsia Prevention Study Group. Pregnancy outcomes in healthy nulliparas who developed hypertension. Obstet Gynecol. 2000. 95:24–28.
4. Knuist M, Bonsel GJ, Zondervan HA, Treffers PE. Intensification of fetal and maternal surveillance in pregnant women with hypertensive disorders. Int J Gynaecol Obstet. 1998. 61:127–133.
5. Sibai BM, Hauth J, Caritis S, Lindheimer MD, MacPherson C, Klebanoff M, et al. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Hypertensive disorders in twin versus singleton gestations. Am J Obstet Gynecol. 2000. 182:938–942.
6. Hnat MD, Sibai BM, Caritis S, Hauth J, Lindheimer MD, MacPherson C, et al. Perinatal outcome in women with recurrent preeclampsia compared with women who develop preeclampsia as nulliparas. Am J Obstet Gynecol. 2002. 186:422–426.
7. ACOG Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002. 99:159–167.
8. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000. 183:S1–S22.
9. Lam C, Lim KH, Karumanchi SA. Circulating angiogenic factors in the pathogenesis and prediction of preeclampsia. Hypertension. 2005. 46:1077–1085.
10. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003. 111:649–658.
11. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004. 350:672–683.
12. Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006. 12:642–649.
13. Taylor RN, Grimwood J, Taylor RS, McMaster MT, Fisher SJ, North RA. Longitudinal serum concentrations of placental growth factor: evidence for abnormal placental angiogenesis in pathologic pregnancies. Am J Obstet Gynecol. 2003. 188:177–182.
14. Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003. 102:181–192.
15. Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994. 309:1395–1400.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download