Abstract
Purpose
The main objective of this study was to reveal the relationship between lower urinary tract symptoms (LUTS) and post-void residual (PVR) urine volume.
Materials and Methods
Between October 2014 and February 2015, older than 40 years patients were included in this study. Volunteers filled out a questionnaire consisted of demographic characteristics, comorbidities, medications, history of surgery and LUTS. Volunteers were undergone PVR measurement with transabdominal ultrasonography. The relationship between symptoms, demographic characteristics and PVR were analyzed.
Results
A total of 939 patients (756 men and 183 women) were enrolled in this study. There was a positive correlation between the sensation of incomplete bladder emptying and PVR volume in all age groups of women (p=0.0001). However such a relationship was found only over the age of 60 in the subgroup analysis of men (p=0.001). PVR volume increased in men by age (0.65 mL per year of age, p=0.011). In men, voiding symptoms and urgency were associated with a high PVR volume. In women, storage and voiding symptoms (except slow stream and terminal dribble) did not correlate with PVR volume.
Conclusions
Our study showed that all men over the age of 60 years and all women with the complaint of feeling of incomplete emptying should undergone PVR measurement. Women with the complaint of poor stream and men mainly with voiding symptoms are other candidates in whom PVR measurement would be considered as an important tool in the clinical management and follow-up.
Postvoid residual (PVR) urine volume is defined as the volume of urine left in the bladder at the end of micturition [1]. Elevation of PVR volume indicates a problem with emptying the bladder but does not show why [2]. The sensation of incomplete bladder emptying is a subjective information for the urologist to evaluate the patients with lower urinary tract symptoms (LUTS). Measurement of PVR is screening test for evaluating voiding dysfunction. This test helps the clinician to identify patients who need further studies to detect optimal treatment modality. Therefore, PVR measurement provides subjective hints and widely used in the daily practice of urologists.
The amount of PVR is very important for quality of life because PVR decreases functional bladder capacity and causes LUTS. Also, it is a risk factor for urinary tract infection [3]. In a study by Truzzi et al. [4] it was concluded that asymptomatic men with an 180 mL or greater PVR are at high risk for bacteriuria. These patients need close follow-up for medical or surgical therapy. Interestingly, PVR does not seem as a forceful factor for acute urinary retention (AUR) [5]. Only there is a risk for AUR if PVR is increasing rapidly [6]. The condition of urinary retention is often associated with LUTS, urinary infections, and bladder stones. Elevated intravesical pressures may lead to hydronephrosis and renal failure [7].
There are two methods of measuring PVR; catheterization and bladder ultrasound. Both of methods have advantages and disadvantages. Sterile catheterization can provide urine sample with a more reliable volume but it is time-consuming and it can cause discomfort, urethral injury, and urinary tract infection. Bladder ultrasound is a noninvasive and time-saving method and can be performed anywhere with a portable device [8]. However, ultrasound needs a trained staff and the results may be operator-dependent and sometimes not accurate as catheterization.
There is no actual numerical value or relative increase in the volume of PVR that has been universally accepted or adopted into current practice [5]. Because of that, it is not appropriate to group patients with or without high PVR volume. There are different opinions about the PVR cut-off point to detect the abnormal and there are various values reported [9]. Most urologists agree that 50–100 mL should be the ideal cut-off for abnormal PVR [8].
This study was planned to evaluate the correlation of LUTS reported by the patients and PVR volumes detected by ultrasound and the reliability of “feeling of incomplete bladder emptying” symptom for determining the amount of residual urine volume in the bladder after voiding.
Between October 2014 and February 2015, 939 patients evaluated in three different urology clinics, were included in this study. All volunteers were >40 years of age. All volunteers filled out a questionnaire which consisted of demographic characteristics, comorbidities, medications, history of surgery and LUTS in Supplementary material. All patients have undergone PVR measurement according to the suggestion of International Consultation of Incontinence with transabdominal ultrasonography. Measurements were performed with signosRT (Signostic Ltd., Thebarton, South Australia) bladder scan.
Then, the relationship between symptoms (including the sensation of incomplete emptying), demographic characteristics, and PVR was analyzed. SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. One way ANOVA and Mann-Whitney U tests were used to determine the significance of the relationship between the symptoms, demographics and PVR and a linear regression model was used to calculate the effect of age on the PVR volume. The Pamukkale University Local Ethics Committee approved the study (approval number: 2015-004) and all patients gave written informed consent. The p-value<0.05 was considered statistically significant.
A total of 939 patients were enrolled in this study (756 men with a mean age 63.0 years and 183 women with a mean age of 60.1). Patients' demographic characteristics and the prevalence of LUTS were shown in Table 1. Daytime frequency was detected as 6.6±3.3 for men and 7.9±4.9 for women. Nocturia frequency was detected 3.0±1.9 for men and 1.9±2.1 for women (p<0.001).
The mean PVR volumes in men and women were 63.9 mL and 21.6 mL, respectively. When classified into age groups, in men mean PVR volume was 56.0 mL in participants aged ≤60 years and 68.9 mL over 60 years of age (p=0.001). In women, PVR volumes were 21.4 mL and 21.6 mL, in participants aged ≤60 years and >60 years, respectively. The relationship between PVR volume and LUTS including the sensation of “incomplete emptying” were shown in Table 2 and Fig. 1. There was a positive correlation between the sensation of incomplete bladder emptying and PVR volume in all age groups of women (p=0.0001). However, such a relationship was found only over the age of 60 in the subgroup analysis of men. In men ≤60 years of age, mean PVR volumes were 59.4 mL and 50.3 mL in participants with and without the sensation of incomplete emptying, respectively. In men over 60 years of age, however mean PVR volumes were 79.5 mL and 56.4 mL in participants with and without the sensation of incomplete emptying, respectively (p=0.001). PVR volume increased in men by age (0.65 mL per year of age, p=0.011). There was not such a relationship in women. In men, the presence of the majority of the voiding symptoms and urgency correlated with a higher PVR volume. In women, none of the storage symptoms was found to be associated with PVR volume and among voiding symptoms slow stream and terminal dribble were the only symptoms that correlated with a high PVR volume.
Further analysis with different PVR cut-offs (50 mL and 100 mL) were carried out if the presence of any LUTS can be used to predict a high residual urine. Urgency, intermittency, hesitancy and straining were the symptoms that were related to a high residual urine in both 50 mL and 100 mL cut-offs. Additionally, nocturia was related to a high PVR when 100 mL was used as the cut-off point.
No correlation was detected between amount of PVR and patients' comorbidities and medications which were grouped as alpha-blockers, 5-alpha-reductase inhibitors, anticholinergics, antihypertensives, antidiabetics, and “others.”
Evaluating the LUTS with questions is widely used in urological practice and the symptoms and complaints that the patients reported are very important for the treatment plan. We tried to determine if any of these complaints could guide us for the presence or a relatively higher amount of PVR, which needs measurement and further evaluation. We also aimed to find the reliability of the feeling of incomplete emptying by comparing the patient related outcome with the measured PVR volume. In this study, we have found that PVR volume correlated well with the sensation of incomplete bladder emptying in all age groups of women however in men such a relationship was found only over the age of 60, which was not demonstrated previously.
There are numerous studies about all the aspects of storage and voiding LUTS in both men and women however there is lack of data about the correlation between these and objectively measured PVR volume which is widely used in current daily practice. Cayetano-Alcaraz et al. [10] analyzed the association between the sensation of incomplete emptying and high PVR volume. In this study no statistically significant association was found between the sensation of incomplete emptying and high PVR in the overall study group including both genders. However a significant association was demonstrated between high PVR volume and the presence of micturition effort. In our study, we only showed such a relation in men.
We also quantitatively determined for the first time that PVR volume increased in men by age (0.65 mL per year). In men, the presence of the majority of the voiding symptoms and urgency correlated with a higher PVR volume. In women, none of the storage symptoms was found to be associated with PVR volume and among voiding symptoms slow stream and terminal dribble were the only symptoms that correlated with a high PVR volume. These might be due a higher number of male participants included in our study and relatively low incidence of voiding symptoms in women.
We previously found the prevalence of “feeling of incomplete bladder emptying” 21.4% in men and 15.5% in women in a population based study [11]. In other studies, Dietz and Haylen [12] and Jeffery et al. [13] reported the incidence of “feeling of incomplete bladder emptying” as 35% and 29.3% respectively. In this study incomplete bladder emptying was reported by 39% of the participants which was relatively higher than the studies mentioned above. We think that this difference was mainly due to the difference in the study groups. In the current study the study group was composed of the patients who admitted to urology outpatient clinics so that LUTS including incomplete bladder emptying might be expected in higher rates.
In this study, we have demonstrated an association between high PVR volume and the symptoms of slow stream, terminal dribble and incomplete emptying in all age groups of women. There was not any relationship between high PVR volume and the remaining LUTS. Jeffery et al. [13] had demonstrated an association between high PVR volume and the symptoms of straining and poor stream. However they did not demonstrate any correlation between PVR volume and other symptoms including incomplete emptying. In the study of Dietz and Haylen [12] which included 414 women the correlation between PVR and poor stream and voiding parameters was demonstrated. Our results are consistent with these studies and therefore measuring PVR volume in all women with the complaint of poor stream can be recommended.
Postmicturition dribble symptom frequently reflects voiding dysfunction due to benign prostate hyperplasia in men. However, it was not widely evaluated for women. Jeffery et al. [13] reported that this symptom was not correlated with elevated PVR volume in women. In our study postmicturition dribble was not associated with elevated PVR volume in men and women.
Groutz et al. [14] reported that the most common symptom among patients with voiding difficulty was the feeling of incomplete emptying. In our study, it was the third most common symptom of voiding and postvoiding symptoms; 4th common voiding and postvoiding symptom in men and the 2nd common voiding and postvoiding symptom in women. In the study of Groutz et al. [14] mean PVR volume (34 mL) of the groups with voiding symptoms was significantly higher than the mean PVR volume (18 mL) of the groups without any voiding symptom. In a study by Lowenstein et al. [15] the mean PVR of women who were bothered with feeling of incomplete emptying was 16 mL higher than those of women who were not bothered and this difference was statistically significant. In our study mean PVR volumes of groups with or without feeling of incomplete emptying was significantly different (16 mL vs. 29 mL). Based on these studies and our findings we can suggest that all women bothered from feeling of incomplete emptying should be undertaken PVR measurement.
In a study that included 668 urodynamic studies it was reported that the symptoms of urgency, urgency incontinence, frequency, nocturia, slow stream, incomplete emptying was not correlated with elevated PVR volume [16]. Chung et al. [17] reported that the patients with wet overactive bladder (OAB) had 20 mL higher PVR than dry OAB patients and the analysis was performed with the both genders included. This data may be considered as a hint for the relation between increased PVR volume and the severity of urgency. In our study, we demonstrated such a relation only in men.
In the literature, there is not enough data to compare our findings in men because the majority of the studies about voiding dysfunction and storage symptoms had been designed to include women. Therefore, we can speculate that our findings about “feeling of incomplete bladder emptying” and “PVR increasing with aging” for men would be useful for urologists.
Our study showed that feeling of incomplete bladder emptying and certain LUTS are related to PVR urine. Although widely used as a noninvasive tool in the assessment of the patients with LUTS in daily practice, PVR measurement becomes more important in all men over the age of 60 years. We can also conclude that all women with the complaint of feeling of incomplete emptying should undergone PVR measurement. Women with the complaint of poor stream and men mainly with voiding symptoms are other candidates in whom PVR measurement would be considered as an important tool in the clinical management and follow-up.
Figures and Tables
Fig. 1
Postvoid residual (PVR) urine volumes (mL) according to the presence of lower urinary tract symptoms (LUTS). *p<0.05.
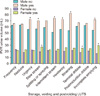
Table 1
Patient demographics and the prevalence of LUTS

Table 2
Mean postvoid residual volumes (mL) according to the presence of lower urinary tract symptoms in both genders

References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178.

2. Nitti VW. Urodynamics and video-urodynamic evaluation of the lower urinary tract. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campell-Walsh urology tenth edition. 10th ed. Philedelphia, PA: Elsevier Saunders;2012. p. 1847–1855.
3. Stern JA, Hsieh YC, Schaeffer AJ. Residual urine in an elderly female population: novel implications for oral estrogen replacement and impact on recurrent urinary tract infection. J Urol. 2004; 171:768–770.

4. Truzzi JC, Almeida FM, Nunes EC, Sadi MV. Residual urinary volume and urinary tract infection--when are they linked? J Urol. 2008; 180:182–185.

5. Kaplan SA, Wein AJ, Staskin DR, Roehrborn CG, Steers WD. Urinary retention and post-void residual urine in men: separating truth from tradition. J Urol. 2008; 180:47–54.

6. Rule AD, Jacobson DJ, McGree ME, Girman CJ, Lieber MM, Jacobsen SJ. Longitudinal changes in post-void residual and voided volume among community dwelling men. J Urol. 2005; 174:1317–1321. discussion 1321-2; author reply 1322.

7. Negro CL, Muir GH. Chronic urinary retention in men: how we define it, and how does it affect treatment outcome. BJU Int. 2012; 110:1590–1594.

8. Kelly CE. Evaluation of voiding dysfunction and measurement of bladder volume. Rev Urol. 2004; 6:Suppl 1. S32–S37.
9. Abdelwahab HA, Abdalla HM, Sherief MH, Ibrahim MB, Shamaa MA. The reliability and reproducibility of ultrasonography for measuring the residual urine volume in men with lower urinary tract symptoms. Arab J Urol. 2014; 12:285–289.

10. Cayetano-Alcaraz AA, Herrera-Cáceres JO, García-Mora A. The relationship between the sensation of incomplete voiding and a high postvoid residual volume. Actas Urol Esp. 2016; 40:309–316.

11. Zumrutbas AE, Bozkurt AI, Tas E, Acar CI, Alkis O, Coban K, et al. Prevalence of lower urinary tract symptoms, overactive bladder and urinary incontinence in western Turkey: results of a population-based survey. Int J Urol. 2014; 21:1027–1033.

12. Dietz HP, Haylen BT. Symptoms of voiding dysfunction: what do they really mean? Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16:52–55. discussion 55.

13. Jeffery ST, Doumouchtsis SK, Vlachos IS, Fynes MM. Are voiding symptoms really associated with abnormal urodynamic voiding parameters in women? Int J Urol. 2008; 15:1044–1048.

14. Groutz A, Gordon D, Lessing JB, Wolman I, Jaffa A, David MP. Prevalence and characteristics of voiding difficulties in women: are subjective symptoms substantiated by objective urodynamic data? Urology. 1999; 54:268–272.

15. Lowenstein L, Anderson C, Kenton K, Dooley Y, Brubaker L. Obstructive voiding symptoms are not predictive of elevated postvoid residual urine volumes. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:801–804.

SUPPLEMENTARY MATERIAL
Scan this QR code to see the supplementary material, or visit http://www.icurology.org/src/sm/icurology-59-38-s001.pdf.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download