This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Performance of minimally-invasive surgery (MIS) is increasing relative to open surgery. We sought to compare the contemporary rates of short-term complications of open versus laparoscopic renal and ureteral surgery in pediatric patients.
Materials and Methods
A retrospective cross-sectional analysis of the National Surgical Quality Improvement Program Pediatrics database was performed of all cases in 2014 identified using CPT procedure codes for nephrectomy, partial nephrectomy (PN), ureteroneocystostomy (UNC), and pyeloplasty, and reviewed for postoperative complications. Univariate analysis was performed to determine 30-day complications, with comparison between open and MIS approaches. Receiver operator curve (ROC) analysis was performed to determine differences in body surface area (BSA) and age for open versus MIS.
Results
Review identified 207 nephrectomies, 72 PN, 920 UNC, and 625 pyeloplasties. MIS was associated with older age and larger BSA except for cases of UNC. Apart from PN, operative durations were longer with MIS. However, only PN was associated with significantly longer length of hospital stay (LOS). There was no difference in incidence of all other 30-day complications. When evaluating BSA via ROC, the area under the curve (AUC) was found to be 0.730 and was significant. Children with a BSA greater than 0.408 m2 were more likely to have MIS (sensitivity, 66.9%; specificity, 69.3%). Regarding age, the AUC was 0.732. Children older than 637.5 days were more likely to have MIS (sensitivity, 72.8%; specificity, 63.3%).
Conclusions
Pediatric MIS is associated with longer operative time for nephrectomy, but shorter LOS following PN. Surgical approach was not associated with difference in short-term complications.
Go to :

Keywords: Complications, Kidney, Minimally invasive surgical procedures, Pediatrics, Postoperative period
INTRODUCTION
In recent times, numerous pediatric surgical procedures have been adapted to less invasive approaches. Technological advances and increased surgeon training have paved the way for increased popularity worldwide. However, application of these techniques may be limited at times by factors such as pediatric body habitus. Body surface area (BSA) dictates the available landscape for laparoscopic port placement and instrument mobility. In pediatric urology, this is particularly relevant to minimally-invasive renal and ureteral surgery.
Trends in utilization of minimally-invasive pediatric urologic surgery are an ever-growing area of interest [
1]. In 2005, the American College of Surgeons (ACS) collaborated with the American Pediatric Surgical Association to develop the ACS National Surgical Quality Improvement Program Pediatrics (NSQIP Peds) [
23]. This is a prospectively collected database of voluntarily submitted cases performed in patients under the age of 18. It is currently drawn from over 100 sites, with each site required to have a full-time trained clinical reviewer. Preoperative and perioperative data, as well as 30-day complication rates are catalogued across most pediatric surgical subspecialties, including urology. Although the data has been well-studied in disciplines such as otolaryngology [
4], plastic surgery [
5], general surgery [
6], neurosurgery [
7], and orthopedics [
8], efforts within urology have been limited [
9101112].
Given the growth in both interest and performance of minimally-invasive variants of pediatric urologic procedures, we aimed to evaluate the difference in 30-day complications following commonly performed renal and ureteral surgeries, with comparison to those accomplished via open surgery.
Go to :

MATERIALS AND METHODS
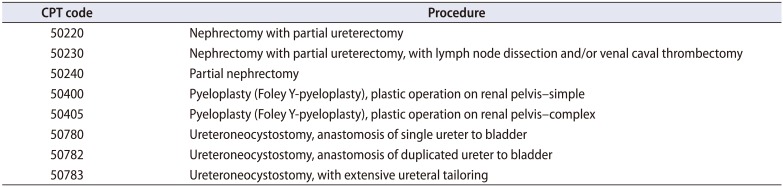
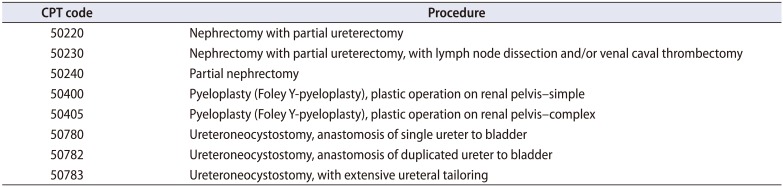
A retrospective cross-sectional analysis of data from surgical cases contained within NSQIP Peds was performed. Per our institutional policy, Institutional Review Board approval is not required for quality improvement review of the NSQIP databases. Cases of ureteroneocystostomy (UNC), pyeloplasty, complete and partial nephrectomy (PN) were identified using CPT procedure codes (
Table 1). All cases for 2014 were identified and postoperative complications were examined. After examining baseline demographic data, we created receiver operator curves (ROCs) as predictor models for determining laparoscopic versus open approach. We then reviewed quality metrics of operative time, length of hospital stay (LOS), and 30-day complication rates for deep and superficial wound infections, urinary tract infections (UTIs), bleeding, and unplanned reoperation or readmission and compared between approaches. All comparisons were done using one-way ANOVA. All statistical analysis was completed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA).
Table 1
Procedures and CPT codes
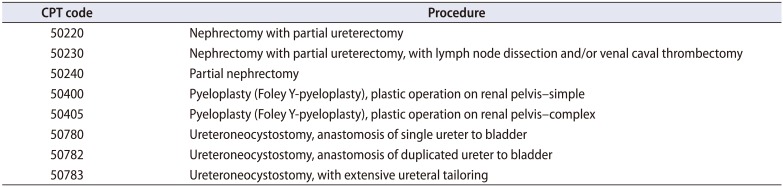
|
CPT code |
Procedure |
|
50220 |
Nephrectomy with partial ureterectomy |
|
50230 |
Nephrectomy with partial ureterectomy, with lymph node dissection and/or venal caval thrombectomy |
|
50240 |
Partial nephrectomy |
|
50400 |
Pyeloplasty (Foley Y-pyeloplasty), plastic operation on renal pelvis-simple |
|
50405 |
Pyeloplasty (Foley Y-pyeloplasty), plastic operation on renal pelvis-complex |
|
50780 |
Ureteroneocystostomy, anastomosis of single ureter to bladder |
|
50782 |
Ureteroneocystostomy, anastomosis of duplicated ureter to bladder |
|
50783 |
Ureteroneocystostomy, with extensive ureteral tailoring |

Go to :

RESULTS
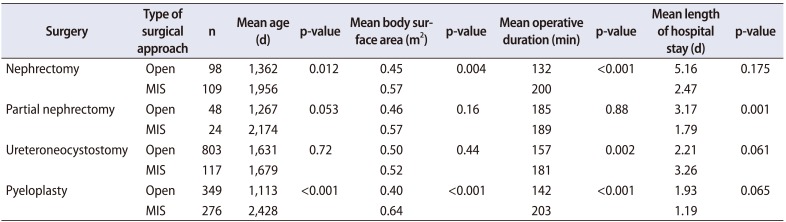
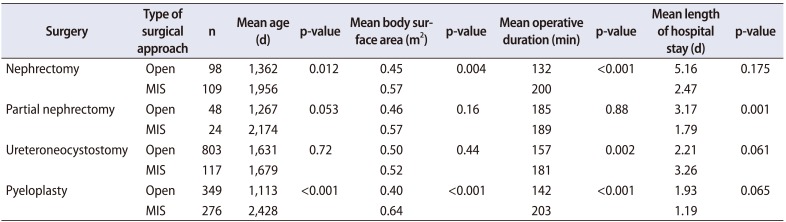
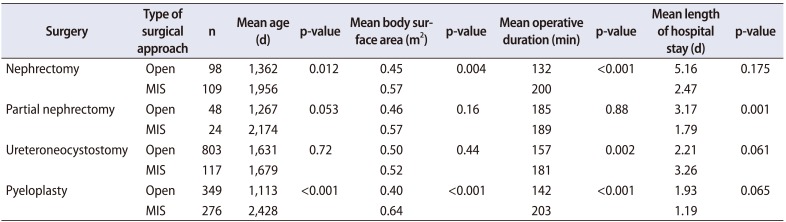
There were 98 and 109 instances of open and minimally-invasive surgery (MIS) for nephrectomy, respectively. Patients undergoing open surgery had a mean age of 1,362 days, and a mean BSA of 0.45 m2, whereas those managed with MIS had a mean age of 1,956 days (p=0.012), and a mean BSA of 0.57 m2 (p=0.004). MIS was associated with longer operative time, with a mean time of 200 minutes for minimally-invasive nephrectomy compared to 132 minutes with the open approach (p<0.001). There was no significant difference in LOS, or rates of wound infections, pneumonia, bleeding/transfusion requirements, pulmonary embolism, UTI, sepsis, death, or readmission.
Regarding PN, there were 48 and 24 instances of open surgery and MIS, respectively. Overall, we found no significant difference in age between open and MIS (1,267 vs. 2,174 days, respectively), but there was a trend towards older children undergoing MIS (p=0.053). There was no significant difference in mean BSA by approach (0.46 m2 vs. 0.57 m2 for open and MIS, respectively; p=0.16). Mean operative duration was essentially equal between groups (185 vs. 189 minutes for open and MIS, respectively; p=0.88). However, LOS was significantly longer following open surgery (3.17 vs. 1.79 days, p=0.001). Comparisons among all other 30-day complication rates found no significant differences.
Review of instances of UNC noted 803 open and 117 MIS cases. Mean age was not significantly different between groups (1,631 vs. 1,679 days for open and MIS, respectively; p=0.72). Likewise, BSA was similar (0.50 m2 vs. 0.52 m2 for open and MIS, respectively; p=0.44). However, MIS took significantly longer (181 vs. 157 minutes, p=0.002). LOS did not reach significance (2.21 vs. 3.26 days for open and MIS, respectively; p=0.061). Comparisons among all other 30-day complication rates found no significant differences.
There were 349 and 276 cases of open and MIS pyeloplasty, respectively. Children undergoing MIS for this indication were significantly older (2,428 vs. 1,113 days, p<0.001). Correspondingly, recipients of MIS had a larger mean BSA (0.64 m
2 vs. 0.40 m
2, p<0.001). Using ROC for BSA, the AUC was found to be 0.730 and was significant (
Fig. 1A). Children with BSA greater than 0.408 m
2 were more likely to have MIS for pyeloplasty, with a sensitivity of 66.9% and a specificity of 69.3%. In terms of age, the AUC was 0.732 (
Fig. 1B). Children older than 637.5 days were more likely to have MIS for pyeloplasty with a sensitivity of 72.8% and a specificity of 63.3%. MIS for pyeloplasty required longer operative time (203 vs. 142 minutes, p<0.001). LOS was similar (1.93 vs. 1.19 days for open and MIS, respectively; p=0.065). Comparisons among all other 30-day complication rates found no significant differences.
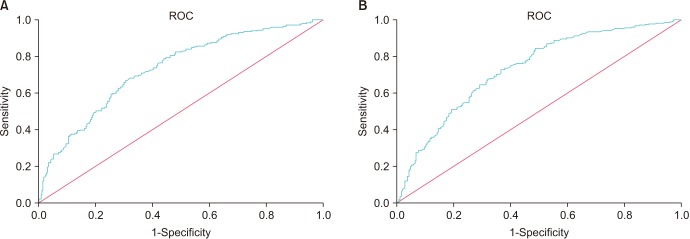 | Fig. 1Receiver operator curves (ROCs) for open versus minimally-invasive pyeloplasty to determine set points of (A) body surface area and (B) age above which children are more likely to undergo minimally-invasive surgery. Diagonal segments are produced by ties.
|
Comparative results are summarized in
Table 2. The rate of superficial and deep wound infections, UTI, bleeding requiring transfusion, pneumonia, and readmission within 30 days was below 0.1% for all queried operations regardless of approach, with no significant differences between approaches in any of these metrics.
Table 2
Comparison of open and MIS variants of common pediatric urologic surgeries
|
Surgery |
Type of surgical approach |
n |
Mean age (d) |
p-value |
Mean body surface area (m2) |
p-value |
Mean operative duration (min) |
p-value |
Mean length of hospital stay (d) |
p-value |
|
Nephrectomy |
Open |
98 |
1,362 |
0.012 |
0.45 |
0.004 |
132 |
<0.001 |
5.16 |
0.175 |
|
MIS |
109 |
1,956 |
0.57 |
200 |
2.47 |
|
Partial nephrectomy |
Open |
48 |
1,267 |
0.05 |
0.46 |
0.16 |
185 |
0.88 |
3.17 |
0.001 |
|
MIS |
24 |
2,174 |
0.57 |
189 |
1.79 |
|
Ureteroneocystostomy |
Open |
803 |
1,631 |
0.72 |
0.50 |
0.44 |
157 |
0.002 |
2.21 |
0.061 |
|
MIS |
117 |
1,679 |
0.52 |
181 |
3.26 |
|
Pyeloplasty |
Open |
349 |
1,113 |
<0.001 |
0.40 |
<0.001 |
142 |
<0.001 |
1.93 |
0.065 |
|
MIS |
276 |
2,428 |
0.64 |
203 |
1.19 |

Go to :

DISCUSSION
Numerous reasons are offered to support the increasing transition to MIS. These include, but are not limited to, improved cosmesis, increased intraoperative visualization, and elimination of human tremor with robotic assistance [
13]. Incorporation of a surgical robot adds cost relative to conventional laparoscopy and open surgery, such that understanding outcomes is important [
14]. This analysis pooled laparoscopic approaches and found that, compared to open surgery, there is no significant advantage in 30-day complications for the operations selected. However, this does not attest to long-term outcomes and cannot be used alone to dictate practice. Efforts such as this must be considered alongside other clinical data to determine the best approach for pediatric patients and the overall healthcare system. Open surgery was only associated with longer LOS for PN. Apart from PN, however, all operations performed via MIS demanded longer operative time than the open surgical approach.
This analysis offers some insight into patient selection. Not unexpectedly, the MIS appears to be increasingly applied to larger/older patients, presumably related to logistics of port placement and maneuverability of instruments with adequate field exposure. Those children managed with MIS for nephrectomy or pyeloplasty were significantly older, with a trend towards significance in PN cases. Similarly, those selected for MIS nephrectomy and pyeloplasty had significantly greater BSA. Again, since BSA increases with age, this is not surprising.
The transition point at which pediatric patients are more likely to undergo a MIS relative to an open approach for a given operation has not been previously reported. The ROC curves for pyeloplasty in this study found that children with BSA >0.408 m2 or age >637.5 days are more likely to receive MIS. The AUC was 0.730 and 0.732, respectively. While these transition points are not definitive and have low sensitivities and specificities, they offer a reasonable estimate, and may be useful in better understanding surgeon decision-making and comparing outcomes. Such information may also guide future instrument development by industry.
Prior evaluations of NSQIP Peds within urology have been limited. One prior study by Wang et al. [
15] reviewed data on UNC alone, and included data from 1998–2012. Unlike our analysis, which focused on more contemporary data alone, they found that patients undergoing MIS UNC were more likely to be older and with a significantly higher rate of 30-day complications. In their work, however, the number of open cases was nearly 100 times higher than those managed with MIS. It is possible that limiting the analysis to more recent data provides better insight into current trends.
It was previously shown that increased specialization results in lower rates of complications and mortality [
19]. While rates of overall 30-day complications following urologic surgery in children have been reported as low as 5.9%, cases involving urinary diversion and incorporation of bowel have been associated with rates as high as 27.8% [
101216]. Adverse events in this early postoperative period seem to be more common among children managed at low-volume centers, especially in cases such as nephrectomy and percutaneous nephrolithotomy [
17]. One analysis of NSQIP Peds data found that increasing body mass index (BMI) was a significant risk factor for post-operative events [
18]. This may serve to highlight the difference in BMI and BSA, as the latter was significantly different between select groups in our study, but without increased risk of 30-day complications.
As with any retrospective database review, this study is not without limitations. This database provides no information regarding quality of life factors related to the improved cosmesis of MIS nor does it provide pain scale assessments of these patients postoperatively. The data is subject to human error in collection. Also, there is no information on long-term clinical outcomes. Additionally, this study of fers no insight into cost, which is of considerable interest to providers. Laparoscopic cases were viewed collectively regardless of robotic assistance. Thus, if the future trend is towards a different balance between conventional and robotic-assisted laparoscopy, repeat analysis may be indicated.
Go to :

CONCLUSIONS
Compared to open surgery, MIS for pediatric instances of nephrectomy, PN, UNC, and pyeloplasty demonstrated no difference in 30-day complication rates. We have determined contemporary thresholds for MIS based on patient age and BSA, which may offer insight into patient-selection by surgeons and subjective impressions of feasibility of MIS relative to patient factors. This information may be useful for future developments in surgical instrumentation. Data on short-term complications such as we've presented should be considered along future cost-analyses and reports of long-term clinical outcomes to better understand and ultimately dictate optimal application of technology relative to patient care.
Go to :

Although there are many studies of surgery outcomes and complications using huge databases in urologic oncology, there are only a few in pediatric urologic surgery. Because the number of pediatric surgeries is much less than the number of oncologic surgeries, more information is needed to evaluate the outcomes and complications of pediatric surgeries from those huge database in order to better define these variables.
The current study showed that minimally-invasive surgery (MIS, including robot-assisted surgery) for pediatric instances of open or partial nephrectomy, ureteral reimplantation (UR), and pyeloplasty compared to open surgery demonstrated no difference in 30-day complication rates from the National Surgical Quality Improvement Program Pediatrics database (NSQIP Peds) at year 2014. However, several issues need clarification to better understand the study findings.
First, the current study was performed with just 1 year of data, and we do not have information on yearly trends to show what kinds of surgeries increased or decreased. Such trends would be interesting to show how MIS vs. open surgery changed over time. A bibliometric analysis showed a progressive trend of increasing volume of reported procedures annually [
1]. From an identified 780 MIS procedures and 75,976 open UR surgeries (NSQIP, 1998–2012), patients who underwent MIS were significantly older (6.2 vs. 4.8 years), more likely to be publicly insured (43% vs. 26%), and more likely to be treated in recent years (90% vs. 46%) compared with patients who underwent open surgery [
2]. Different outcomes in the current study compared with previous results are caused by the relatively recent 1-year data.
Second, the authors focused mainly on length of stay and surgical time to analyze the differences between MIS and open surgery. However, the beauty of MIS is not only the benefits for length of stay but also and importantly those for quality of life such as the reduced pain scale and improved cosmesis.
Nevertheless, the current study reports current trends showing that pediatric urologists like to perform conventional open surgeries earlier in children with lower surface area and younger age. With advancing technology and as pediatric urologists gain experiences [
345], it is expected that MIS will become more popular for pediatric surgeries as for oncologic surgeries.