Abstract
Purpose
This study aimed to demonstrate a method to easily assess bladder capacity using knowledge of day-time voided volumes, which can be obtained even from patients with nocturnal enuresis where the first morning void cannot accurately predict the bladder capacity due to bladder emptying overnight.
Materials and Methods
We evaluated 177 healthy children from 7 Korean medical centres entered the study between January 2008 and January 2009. Voided volumes measured for more than 48 hours were recorded in the frequency volume chart (FVC).
Results
Most voided volumes during day-time were showed between 30% and 80% of the maximal voided volume (MVV). The maximal voided volume during day-time (MVVDT) was significantly less than the MVV (179.5±71.1 mL vs. 227.0±79.2 mL, p<0.001). The correlation coefficients with the MVV were 0.801 for the estimated MVV using the MVVDT (MVVDT×1.25), which suggested a fairly strong relationship between the MVVDT×1.25 and the MVV.
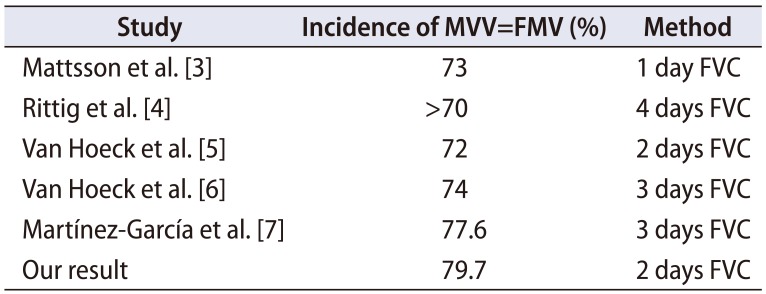
Determining bladder capacity has been a key factor for deciding upon the most suitable treatment modality for nocturnal enuresis [1]. While there are several invasive tools for determining bladder capacity, such as cystometry and cystography, one non-invasive tool is the frequency volume chart (FVC), in which the term maximal voided volume (MVV) is used to describe the volume that the bladder can accommodate [2]. In healthy children, the MVV is typically the first morning void (FMV). The FMV means the voided volume just after awakening in the morning without nighttime wetting or nocturia. Previous studies showed that the FMV was the MVV in more than 70% of cases (Table 1), reflecting the increased volume that the bladder can accommodate during sleep [34567]. In other words, the first voided volume after waking up in the morning is generally the largest voided volume recorded in the FVC. For this reason, the MVV must be assessed using the FVC including the FMV, which can lead to accurate estimation of the real bladder capacity. However, in patients with monosymptomatic nocturnal enuresis, the first voided volume after waking up is typically not the MVV since the bladder has already been emptied during sleep due to nighttime wetting [8]. Patients with nocturnal enuresis can easily record voided volumes except the FMV throughout the day, which are called “day-time voided volumes” in this study. The objectives of the present study on the basis of the FVC in healthy children were to confirm that the MVV is different depending on whether or not the FVC includes the FMV and to demonstrate a method to estimate the real bladder capacity easily using only the day time voided volumes when the FMV must be excluded, as in patients with nocturnal enuresis.
We evaluated healthy children who were volunteered by their parents to participate in the study. Children from 7 Korean medical centres were enrolled in the study between January 2008 and January 2009. The study protocol was approved by an Institutional Review Board of Dong-A University Hospital (approval number: 14-179). To avoid classroom regimens for voiding, all collections were performed during weekends or holidays. Children with a history of urinary tract infection, urologic pathology including vesicoureteral reflux, urinary incontinence, nocturnal enuresis, and gastrointestinal symptoms including constipation were excluded from the study. The health of the children was confirmed by a questionnaire completed by their parents. All participants provided written informed consent.
Children and/or their parents were instructed on the use of the FVC. Voided volumes were measured for more than 48 hours using a polyethylene cup with a maximum capacity of 600 mL (supported by Ferring Korea). The volumes and times of each voiding and the times of waking and sleeping were recorded in the individual FVCs. The MVV was defined as the largest voided volume on an individual FVC. The FMV was the first voided volume in the morning without nighttime wetting or nocturia. The largest day-time voided volume that was not the FMV was defined as the maximal voided volume during day-time (MVVDT). The smallest voided volume during the day-time was defined as the minimal voided volume during the day-time (mVVDT). To evaluate the correlation between the MVVDT or mVVDT and the MVV, the ratios of MVVDT or mVVDT to MVV were analysed (Rmax=MVVDT/MVV, Rmin=mVVDT/MVV). The data are reported as the mean±standard deviation. The MVVs estimated using the day-time voided volumes excluding the FMV were calculated using the following formulas, eMVVmax=MVVDT×(1/Rmax) using the MVVDT and eMVVmin=mVVDT×(1/Rmin) using the mVVDT. Pearson's correlation coefficient was used to calculate correlations between the eMVVmax or eMVVmin and the MVV. Linear regression analysis was used to find the best linear model to estimate bladder capacity by age. The expected bladder capacity for each age was calculated using the formula bladder capacity (mL)=(age+1)×30 [9]. Children with an MVV <65% of the expected bladder capacity for their age were considered to have a decreased bladder capacity. Statistical analyses were performed using SPSS ver. 11.0 software (SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered statistically significant.
Complete FVC data recorded for 48 hours or more were available from 177 subjects (86 males and 91 females) out of the 298 children that initially volunteered for the study. The mean age of the subjects was 5.8±2.7 years. In 79.7% of the subjects, the FMV equalled the MVV. The mean Rmax (MVVDT/MVV) was 0.80±0.17 (0.35–1.00) and the mean Rmin (mVVDT/MVV) was 0.30±0.15 (0.08–0.73) (Fig. 1). When the MVV was estimated using only the day-time voided volumes on the basis of Rmax and Rmin, the eMVVmax was MVVDT/0.8 (=MVVDT×1.25) and the eMVVmin was mVVDT/0.3 (=mVVDT×3.33). Table 2 summarizes parameters used to understand bladder capacity. While there were no differences between eMVVmax, eMVVmin, and MVV (p>0.05), the MVVDT was significantly less than the MVV (p<0.001). In other words, the largest volume among the day-time voided volumes excluding the FMV was significantly less than the MVV when the FMV was included. A total of 13 children (7.3%) and 39 children (22.0%) were considered to have a decreased bladder capacity compared to that expected for their age when the FMV was included or excluded, respectively (Fig. 2). Pearson's correlation coefficient was used to analyse whether eMVVmax and eMVVmin calculated using day-time voided volumes (MVVDT×1.25 and mVVDT×3.33) could actually estimate the true MVV. The correlation coefficients with MVV were 0.801 for the eMVVmax (p<0.001) and 0.452 for the eMVVmin (p<0.001). This result suggested a fairly strong relationship between the eMVVmax and the MVV. Fig. 3 shows scatter plots of eMVVmax and eMVVmin versus age. Linear regression analysis suggested the following formula for estimation of eMVVmax and eMVVmin by age: eMVVmax (mL)=11.8×age (years)+158.2 (r2=0.244, p<0.001), eMVVmin (mL)=4.6×age (years)+200.1 (r2=0.117, p<0.001). The formula derived using the eMVVmax was similar to a previously reported formula for bladder capacity [10].
Determining bladder capacity is important for helping decide treatment modalities for patients with nocturnal enuresis. Specifically, bladder capacity has been a predictor of the impact of desmopressin on nocturnal enuresis [1112]. The FVC is a common, functional tool used to measure the bladder capacity in clinical practice. Out of all parameters derived from the FVC, the MVV is used to describe the bladder accommodating ability [2]. The FMV is typically the MVV because the bladder is able to accumulate the largest amount of urine during sleep [13]. According to data from previous studies and the present one, the FMV corresponded to the MVV in 70% or more of FVCs [34567]. However, the FMV in patients with nocturnal enuresis is typically not the MVV since they void prior to awakening. Van Hoeck et al. [5] demonstrated that the FMV equated to the MVV in 72% of normal children, but in only 28% of children with nocturnal enuresis. If the MVV is not the FMV, but another day-time voided volume, then it will likely be less than when the MMV is the FMV after a night without voiding. In the current study, the MVV determined by excluding the FMV was about 20% less than including the FMV. Diagnosis of decreased bladder capacity was therefore increased by about 15% (false positives). In accordance with the current study, Rittig et al. [4] reported that the MVV determined by including the FMV was 80 to 100 mL higher than the MVV excluding the FMV. Tauris et al. [12] showed that there was a 13.5% difference in diagnosis of decreased bladder capacity, depending on whether or not the FMV was included. These results confirm the importance of accurately knowing the FMV for determining the bladder capacity, and suggest that the FVC including the FMV should not be compared with excluding it.
Previous studies proposed alternatives to compensate for the FMV not equating with the MVV in patients with nocturnal enuresis. The first method is to check the weight of a diaper at the time of enuresis using an enuretic alarm [1415]. However, the voided volume at that time was likely to be smaller than the estimated bladder capacity because enuresis episodes commonly associated with incomplete bladder emptying [16]. The second method is to measure the volume after postponing urination for as long as possible [17]. However, when this was done with normal children, a significant number were diagnosed with decreased bladder capacity, indicating that the method was inaccurate [5]. The present study suggests a new method where MVVDT×1.25 (eMVVmax) was regarded as the bladder capacity when the FMV could not be obtained, as in patients with nocturnal enuresis. This method can be easily used to estimate the bladder capacity using only day-time voided volumes such as MVVDT and mVVDT in patients with nocturnal enuresis. In this study, there was a high correlation between the real MVV and eMVVmax. When using eMVVmax to determine the bladder capacity in normal children, decreased bladder capacity was diagnosed as little as by using the real MVV. In addition, the formula for eMVVmax by age is in close agreement with the formula for the MVV by age in our previous study [10], and therefore it is considered that eMVVmax (=MVVDT×1.25) can sufficiently replace the MVV if necessary. It should be noted that the formula of Pearson's correlation (eMVVmax=11.8×age (years)+158.2) suggests that applying MVVDT×1.25 seems likely to overestimate bladder capacity for children under 5 years of age. Since patients who were diagnosed with nocturnal enuresis are over 5 years of age, it seems to be no problem to apply it to patients with nocturnal enuresis.
In the present study, the correlation coefficient between eMVVmin and the MVV was smaller than between eMVVmax and the MVV. The formula for estimation of eMVVmin by age was quite different from our previous study. One reason is that the FVC included small volumes voided during defecation, in which consist of these without desire for urination, and consequently FVC included unnatural small volumes voided, and which could change the correlation coefficient between the eMVVmin and the MVV.
The limitation of the present study may be the relatively short duration (48-hours) for the FVC. In other studies, two weekends (4 days) of use of the FVC was necessary to obtain a reproducible estimate of the MVV including the FMV [18]. Although all of the children were considered healthy by an interview and a questionnaire, 7.3% of them were diagnosed with decreased bladder capacity in our study. If a longer recording period could be obtained, it is possible that the FMV could more accurately reflect a full bladder. A second limitation of our study is including voids during defecation. These data worsened the variation of values derived from the FVC.
The FMV equalled the MVV in about 80% of the healthy children included in the study. The MVV is significantly different depending on whether or not the FVC includes the FMV. Therefore, the FMV is important for accurately evaluating bladder capacity. When an accurate FMV volume cannot be obtained, as in patients with nocturnal enuresis, calculating MVVDT×1.25 allows easy estimation of the bladder capacity and significantly correlates with the real MVV, as determined by studying healthy children.
References
1. Rushton HG, Belman AB, Zaontz MR, Skoog SJ, Sihelnik S. The influence of small functional bladder capacity and other predictors on the response to desmopressin in the management of monosymptomatic nocturnal enuresis. J Urol. 1996; 156:651–655. PMID: 8683752.
2. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.

3. Mattsson S, Gladh G, Lindström S. Relative filling of the bladder at daytime voids in healthy school children. J Urol. 2003; 170:1343–1346. PMID: 14501766.

4. Rittig S, Kamperis K, Siggaard C, Hagstroem S, Djurhuus JC. Age related nocturnal urine volume and maximum voided volume in healthy children: reappraisal of International Children's Continence Society definitions. J Urol. 2010; 183:1561–1567. PMID: 20176383.

5. Van Hoeck K, Bael A, Lax H, Hirche H, Van Dessel E, Van Renthergem D, et al. Urine output rate and maximum volume voided in school-age children with and without nocturnal enuresis. J Pediatr. 2007; 151:575–580. PMID: 18035133.

6. Van Hoeck K, Bael A, Lax H, Hirche H, van Gool JD. Circadian variation of voided volume in normal school-age children. Eur J Pediatr. 2007; 166:579–584. PMID: 17043843.

7. Martínez-García R, Ubeda-Sansano MI, Díez-Domingo J, Pérez-Hoyos S, Gil-Salom M. It is time to abandon "expected bladder capacity." Systematic review and new models for children's normal maximum voided volumes. Neurourol Urodyn. 2014; 33:1092–1098. PMID: 23847007.

8. Mattsson SH. Voiding frequency, volumes and intervals in healthy schoolchildren. Scand J Urol Nephrol. 1994; 28:1–11. PMID: 8009180.

9. Hjalmas K, Arnold T, Bower W, Caione P, Chiozza LM, von Gontard A, et al. Nocturnal enuresis: an international evidence based management strategy. J Urol. 2004; 171:2545–2561.

10. Kim SO, Kim KD, Kim YS, Kim JM, Moon du G, Park S, et al. Evaluation of maximum voided volume in Korean children by use of a 48-h frequency volume chart. BJU Int. 2012; 110:597–600. PMID: 22145861.

11. Radvanska E, Kovács L, Rittig S. The role of bladder capacity in antidiuretic and anticholinergic treatment for nocturnal enuresis. J Urol. 2006; 176:764–768. discussion 768-9. PMID: 16813940.

12. Tauris LH, Kamperis K, Hagstroem S, Bower WF, Rittig S. Tailoring treatment of monosymptomatic nocturnal enuresis: the role of maximum voided capacity. J Urol. 2012; 187:664–669. PMID: 22177206.

13. Graugaard-Jensen C, Schmidt F, Thomsen HF, Djurhuus JC. Normal voiding patterns assessed by means of a frequency-volume chart. Scand J Urol Nephrol. 2008; 42:269–273. PMID: 18432534.

14. Kawauchi A, Tanaka Y, Naito Y, Yamao Y, Ukimura O, Yoneda K, et al. Bladder capacity at the time of enuresis. Urology. 2003; 61:1016–1018. PMID: 12736027.

15. Hagstroem S, Kamperis K, Rittig S, Djurhuus JC. Bladder reservoir function in children with monosymptomatic nocturnal enuresis and healthy controls. J Urol. 2006; 176:759–763. PMID: 16813939.

16. Hagstroem S, Kamperis K, Rittig S, Rijkhoff NJ, Djurhuus JC. Monosymptomatic nocturnal enuresis is associated with abnormal nocturnal bladder emptying. J Urol. 2004; 171:2562–2566. discussion 2566. PMID: 15118419.

17. Van Hoeck KJ, Bael A, Van Dessel E, Van Renthergem D, Bernaerts K, Vandermaelen V, et al. Do holding exercises or antimuscarinics increase maximum voided volume in monosymptomatic nocturnal enuresis? A randomized controlled trial in children. J Urol. 2007; 178:2132–2136. PMID: 17870123.

18. Hansen MN, Rittig S, Siggaard C, Kamperis K, Hvistendahl G, Schaumburg HL, et al. Intra-individual variability in nighttime urine production and functional bladder capacity estimated by home recordings in patients with nocturnal enuresis. J Urol. 2001; 166:2452–2455. PMID: 11696810.

Fig. 1
Scatter plots of the MVVDT/MVV (Rmax) and mVVDT/MVV (Rmin) ratios. The mean Rmax was 0.80±0.17 (0.35–1.00) and mean Rmin was 0.30±0.15 (0.08–0.73). MVV, maximal voided volume; VVDT, voided volume during day-time; MVVDT, maximal VVDT; mVVDT, minimal VVDT.
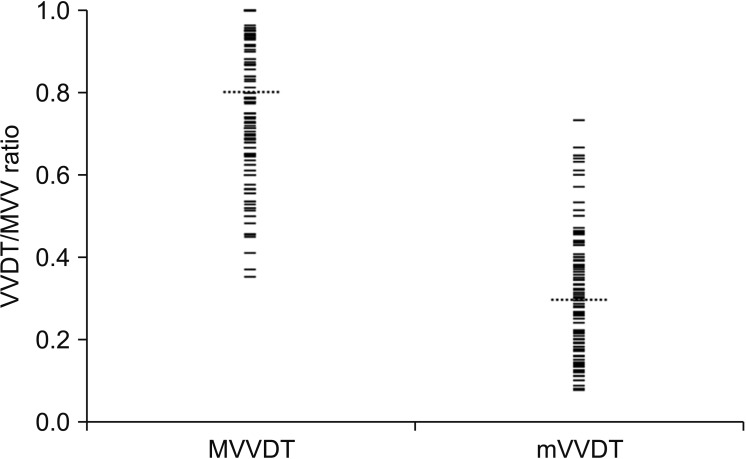
Fig. 2
Scatter plots of the maximal voided volume during day-time (MVVDT) and the maximal voided volume (MVV) versus age. The dotted line is the limit below which children are considered to have decreased bladder capacity compared to estimated bladder capacity for their age (y=0.65×30×(age+1)). (A) While 22.0% of the data points are below the line in the MVVDT vs. age plot, (B) 7.3% are below the line in the MVV vs. age plot.
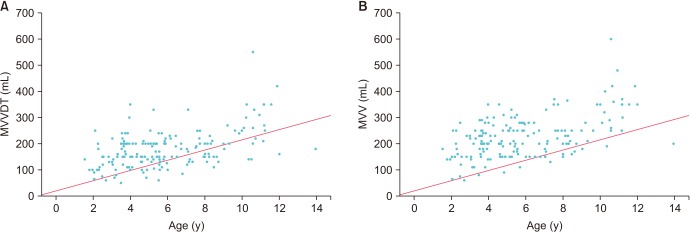
Fig. 3
The estimated maximal voided volume using the maximal voided volume during day-time (MVVDT) and the minimal voided volume during the day-time (mVVDT) eMVVmax (A) and eMVVmin (B) plotted versus age, with 5% and 95% reference ranges (dotted grey lines). Y=0.65×30×(age+1) (thin solid line).
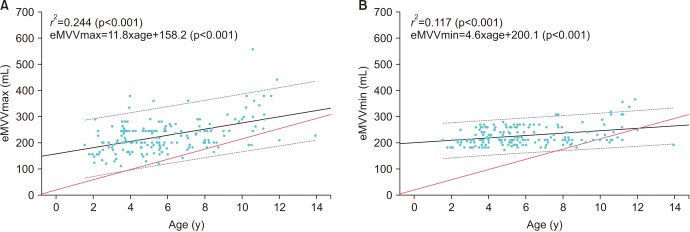
Table 1
Studies demonstrating the incidence of the first morning void being equivalent to the maximal voided volume
| Study | Incidence of MVV=FMV (%) | Method |
|---|---|---|
| Mattsson et al. [3] | 73 | 1 day FVC |
| Rittig et al. [4] | >70 | 4 days FVC |
| Van Hoeck et al. [5] | 72 | 2 days FVC |
| Van Hoeck et al. [6] | 74 | 3 days FVC |
| Martínez-García et al. [7] | 77.6 | 3 days FVC |
| Our result | 79.7 | 2 days FVC |
Table 2
Demographic data of the children included in this study (n=177)
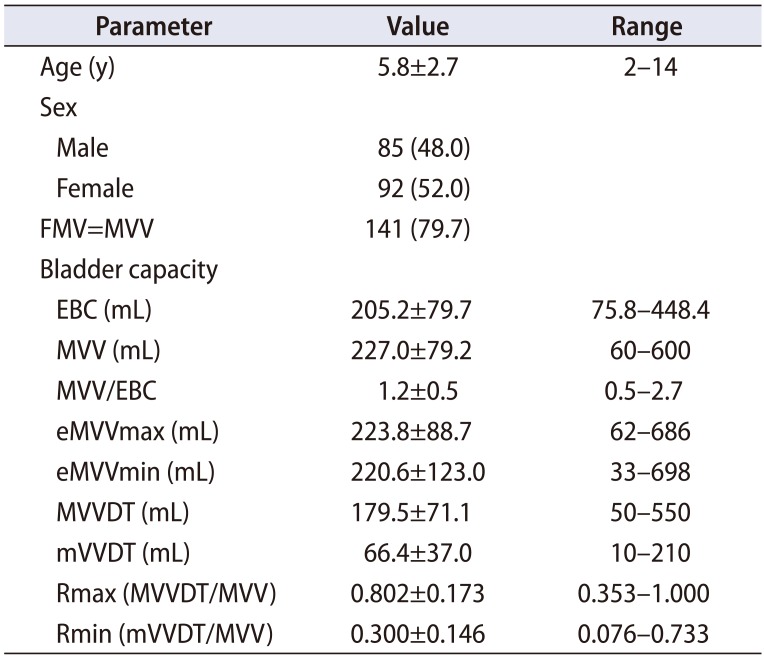
Values are presented as mean±standard deviation, number (%), or range.
FMV, first morning void; MVV, maximal voided volume; EBC, estimated bladder capacity (by age); MVVDT, maximal voided volume during day-time; mVVDT, minimal voided volume during day-time.
EBC=(age+1)×30. eMVVmax=MVVDT/0.80. eMVVmin=mVVDT/0.30.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download