Abstract
Purpose
Local anesthetic agents such as bupivacaine and lidocaine are commonly used after surgery for pain control. The aim of this prospective study was to evaluate the safety of a mixture of bupivacaine and lidocaine in children who underwent urologic inguinal and scrotal surgery.
Materials and Methods
Fifty-five patients who underwent pediatric urologic outpatient surgeries, were prospectively enrolled in this study. The patients were divided into three groups according to age (group I: under 2 years, group II: between 3−4 years, and group III: 5 years and above). Patients were further sub-divided into unilateral and bilateral groups. All patients were injected with a mixture of 0.5% bupivacaine and 2% lidocaine (2:1 volume ratio) at the surgical site, just before the surgery ended. Hemodynamic and electrocardiographic parameters were measured before local anesthesia, 30 minutes after administration of local anesthesia, and 60 minutes after administration.
Results
The patients' mean age was 40.5±39.9 months. All patients had normal hemodynamic and electrocardiographic parameters before local anesthesia, after 30 minutes, and after 60 minutes. Also, results of all intervals were within normal values, when analyzed by age and laterality. No mixture related adverse events (nausea, vomiting, pruritus, sedation, respiratory depression) or those related to electrocardiographic parameters (arrhythmias and asystole) were reported in any patients.
Pain control is important in improving both clinical outcomes and patient comfort [1]. In pediatric patients, local anesthesia is commonly used, as it is a reliable, safe, and easy method of pain control. Therefore, it is common to inject local anesthetics at the end of surgery to relive postoperative pain [2]. Lidocaine is often used as local anesthesia because it is associated with a fast onset of sensory blockade and good efficacy. In clinical practice, a mixture of lidocaine and bupivacaine is often used [3]. The former quickly blocks sensations, and the latter blocks the senses for a long time, so they are mixed to take advantage of both [3]. The onset of action of bupivacaine is 5 to 10 minutes and it has a duration of effect of up to six hours [2].
The toxic effects of local anesthetic agents are relatively well documented [3]. The most prevalent form of toxicity of local anesthetics is cardiovascular toxicity. The two most important components of local anesthetic cardiac toxicity are arrhythmias and contractile depression. An overdose of a local anesthetic agent is likely to cause hypoxia and exacerbate cardiotoxicity. Deterioration of myocardial hypoperfusion worsens cardiac function and can lead to failed resuscitation [4]. These events often manifest as abnormal findings on electrocardiograms (ECGs). Specifically, bupivacaine toxicity tends to widen the QRS complex, leading to arrhythmias and asystole. A high dose of lidocaine can cause prolongation of the pulse rate (PR) time, widening of the QRS complex, atrioventricular (AV) block, and circulatory failure [5].
Based on a literature review, there is as yet no prospective study on hemodynamic and cardiac changes of local anesthetic agents in children who underwent urologic surgery. Therefore, we evaluated the safety of a mixture of bupivacaine and lidocaine in children who underwent urologic inguinal and scrotal surgery. Since cardiac function develops along with advancing age of the child, we investigated the effect of the local anesthetic on the hemodynamic and electrocardiographic changes, according to age and laterality.
A prospective analysis on the hemodynamic and cardiac safety of a mixture of bupivacaine and lidocaine was carried out in a single institution from December 2011 to March 2012 with written informed consent (PNUYH approval number: IRB 03-2014-029). After receiving informed patient consent, 55 children classified as American Society of Anesthesiologists grades I and II who were undergoing elective surgical procedures such as inguinal hernia repair, hydrocelectomy, or orchiopexy were included in this prospective study. Children with a history of allergic reactions to local anesthetic agents, coagulopathy, preexisting neurological or cardiac diseases, mental retardation, and neuromuscular disorders were excluded from this study.
Demographic parameters, such as age, weight, gender, and laterality, were recorded. The patients were allocated into one of 3 groups by age. Group I included patients less than 2 years of age, group II included those 3 to 4 years of age, and group III included those 5 years of age or older.
The patients were further subdivided into unilateral and bilateral groups. The unilateral group received a single local anesthetic, whereas the bilateral group received a local anesthetic twice, without exceeding the maximum dose.
After all surgical procedures were completed, local anesthesia was administered with a mixture of 0.5% bupivacaine and 2% lidocaine (2:1 volume ratio) via injection into the surgical wound. The maximal dose of lidocaine was 3 mg/kg and the maximal dose of bupivacaine was 1.5 mg/kg. For example, when the weight of the child was 10 kg, the maximum dose of the mixture was 0.5% bupivacaine 3 mL (15 mg) and 2% lidocaine 1.5 mL (30 mg).
Electrocardiographic and hemodynamic parameters were recorded three times, just before local anesthesia, 30 minutes after administration, and 60 minutes after administration. Electrocardiographic parameters included PR interval, QRS interval, and QT interval. Clinically significant PR interval in this study was defined as 0.16 seconds or more in group I, and 0.17 seconds or more in groups II and III. Significant QRS widening was set at 0.08 seconds or more in groups I and II, and 0.09 seconds or more in group III. This is because QRS widening is defined as 0.09 seconds or more in patients older than 5 years. The normal value of the QT interval in pediatric ECG is 0.44 seconds or less [6]. The hemodynamic parameters included blood pressure, heart rate, and respiratory rate. The clinically adverse events related to the mixture of bupivacaine and lidocaine, such as nausea, vomiting, pruritus, respiratory depression, and hypotension, were assessed at the time of discharge and at the outpatient clinic one week after discharge.
Statistical analysis was done using the chi-squared test using SPSS statistical software version 13.0 (SPSS Inc., Chicago, IL, USA). The p<0.05 was regarded as statistically significant. Data are reported as mean±standard deviation.
Patient characteristics are summarized in Table 1. Hemodynamic parameters before local anesthesia, after 30 minutes, and after 60 minutes were normal in all patients. Mean systolic blood pressure before local anesthesia, 30 minutes after, and 60 minutes after was 105.0±14.6 mmHg, 121.5±21.4 mmHg (p<0.001), and 126.7±17.9 mmHg (p<0.001), respectively. Mean PR before local anesthesia, 30 minutes after, and 60 minutes after administration were 137.3±23.7 /minute, 142.2±28.0/minute (p=0.322), and 136.4±38.7/minute (p=0.887), respectively. There was no significant difference in these results. The respiratory rate 60 minutes after administration of local anesthesia was 26.1±11.2/minute (p=0.008) (Table 2).
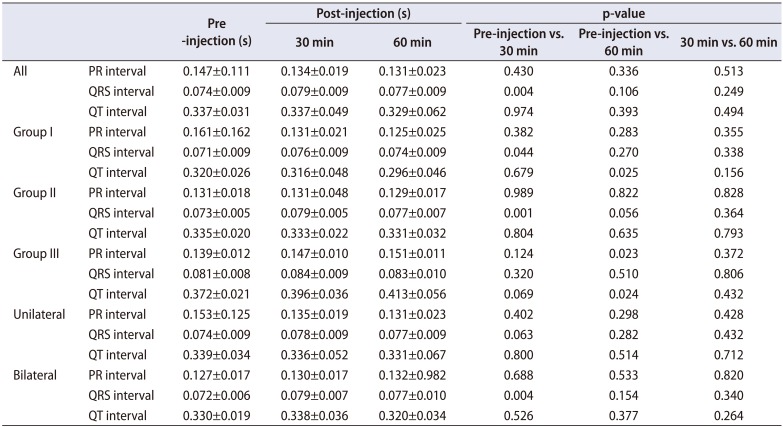
Electrocardiographic parameters before local anesthesia, 30 minutes after, and 60 minutes after administration were normal in all patients. The PR interval before local anesthesia, 30 minutes after local anesthesia, and 60 minutes after local anesthesia was 0.147±0.111 seconds, 0.134±0.019 seconds (p=0.430), and 0.131±0.023 seconds (p=0.336), respectively. The QRS interval before local anesthesia, 30 minutes after local anesthesia, and 60 minutes after local anesthesia was 0.074±0.009 seconds, 0.079±0.009 seconds (p=0.004) and 0.077±0.009 seconds (p=0.106), respectively. The QT interval before local anesthesia, 30 minutes after local anesthesia, and 60 minutes after local anesthesia was 0.337±0.031 seconds, 0.337±0.049 seconds (p=0.974) and 0.329±0.062 seconds (p=0.393), respectively (Table 3).
When analyzed by age, we observed significant PR interval differences in group III, 60 minutes after local anesthesia (p=0.023). Significant QT interval differences were observed in group I and III at 60 minutes after local anesthesia (p=0.025, 0.024, respectively). Also, significant QRS interval differences were observed in groups I and II, at 30 minutes after local anesthesia (p=0.044, 0.001, respectively). However, all intervals were within the normal range.
When analyzed by laterality, significant QRS interval differences were observed in patients who underwent bilateral surgery 30 minutes after local anesthesia (p=0.004). However, all intervals were within normal values (Table 3).
No clinically adverse events related to administration of the mixture of bupivacaine and lidocaine, were observed at the time of discharge and at the outpatient clinic one week after discharge.
More than 80% of patients undergoing surgery experience acute pain after surgery, and about 75% of them report moderate or severe pain [7]. Inadequately controlled pain negatively affects function, quality of life, and functional recovery, and there is a risk of persistent postsurgical pain and postsurgical complications [8]. Owing to difficulties in assessing pain and concern about lowering cardiorespiratory function, children often do not receive appropriate treatment for postoperative pain [1]. Operating rooms and recovery rooms are unfamiliar and unpleasant environments for children. In addition, isolation from parents, hunger, and pain during surgery can cause stress and can lead to prolonged hospital stays, and can increase the cost of care [3]. Several physiological changes, including increases in heart rate, respiratory rate, blood pressure, sweating, and decreases in vagal tone and oxygen saturation are used to assess pain in children [9]. Furthermore, a patient's clinical condition is affected by hypoxemia, hypoglycemia, body temperature, and sepsis [10].
The American Pain Society published a practice guideline for acute pain management in the perioperative setting in 2012 [11]. Multiple analgesics are more effective for pain relief than monoform intervention because different analgesics have different effects on central and/or peripheral nervous systems [8]. Many tools use both physiological and behavioral measures to determine pain scores [11]. Local anesthesia is a simple-to-use technique for post-operative pain management [2]. Toxicity of local anesthetics is mostly attributable to high plasma concentrations of such agents [12].
The cardiotoxic effects of local anesthesia are relatively well known. Typical effects seen on ECG include lengthening of the PR interval and widening of the QRS complex [4]. Ventricular conduction depends only on the sodium channel, and QRS widening reflects the effects of the drug on ventricular conduction [13].
Bupivacaine is a long-acting amide-based topical anesthetic that is commonly used in clinical practice [14]. Unlike lidocaine, which binds and dissociates quickly, bupivacaine blocks the myocardial sodium channel and regulates the channels slowly during the heart relaxation period [15]. In vitro studies, bupivacaine has been shown to cause a significant decrease in blood pressure and heart rate through electrical excitability of the heart and dilation of blood vessels [16].
Some studies have investigated the impact of bupivacaine on the baroreflex, which acts in the rat heart and brainstem [3]. Krikava et al. [3] reported that bupivacaine was selectively toxic to the cardiovascular control center located in the brainstem. Large amounts of bupivacaine significantly reduce myocardial contractility and impair cardiac electrophysiology, particularly ventricular conduction. Laskowski et al. [17] reported that increased heart rate via anesthesia in dogs given large doses of bupivacaine promotes ventricular interval prolongation, QRS enlargement, and the development of ventricular arrhythmias.
Lidocaine is a short-acting drug that is classified as a 1B antiarrhythmic drug in the Vaughan Williams classification [5]. However the elimination half-life of lidocaine is around 90 to 120 minutes in most patients [5]. Lidocaine acts on similar sites as bupivacaine and sodium channels, but lidocaine and bupivacaine have different effects on the heart [5]. Lidocaine competes with bupivicaine at the sodium channel binding site [5]. For this reason, lidocaine is used to treat cardiac toxicity caused by bupivacaine [5]. Some animal studies suggest a protective effect of lidocaine when mixed with bupivacaine [18]. One researcher suggested that addition of lidocaine with bupivacaine in pigs increases the threshold at which bupivacaine causes ventricular fibrillation [18].
Toxicity due to local anesthesia can be prevented by careful injection techniques, careful observation, and knowledge of the maximum dose based on body weight. Doctors should start with aspiration before injecting anesthetics, and inject slowly [19]. Rapid recognition of toxicity is important for an effective response. If toxic symptoms are present, administration of local anesthetic should be discontinued immediately [20].
Krikava et al. [3] described the effects of bupivacaine and lidocaine. After administration of bupivacaine, lidocaine, or a mixture of the two to the heart of an isolated rat, electrophysiological parameters and QRS duration were followed. In the group that received a mixture of bupivacaine and lidocaine, heart rate was significantly decreased, and the administration of bupivacaine induced significant elongation of QRS and prolongation of PQ [3].
Significant prolongation (p<0.05) of QRS was seen in the bupivacaine (6 µg/mL) group in comparison with the group given a mixture of bupivacaine (6 µg/mL) and lidocaine (12 µg/mL) [3]. However, after 60 minutes of stabilization, QRS enlargement rapidly recovered in both groups given bupivacaine [3].
Our study showed that a mixture of bupivacaine and lidocaine alters the ventricular conduction parameters, particularly the QRS interval, which is prolonged. QRS is the most prominent waveform in ECG parameters [21]. It is an electrical signal that appears during the heart's ventricular contraction; hence, its interval and shape represent a lot of information about the current state of the heart [21]. Abnormal width of these QRS indicates ventricular conduction disturbances, such as ventricular arrhythmia, bundle branch blocks, WPW and heart failure [21]. QRS widening can be the result of ventricular remodeling in cardiomyopathy, ventricular fibrosis secondary to myocardial injury or infarction [21]. Clinically significant QRS widening in children under 5 years is usually 2 small boxes or more (0.08 seconds or 80 msec). For patients older than 5 years, the QRS widening is defined as 0.09 seconds or more [6]. In infants and young children under 2 years, a PR interval of 0.16 seconds (≥160 msec or 4 small boxes) is associated with AV block [6]. The normal value of the QT interval in pediatric ECG is 0.44 seconds or less [6].
In this study, significant electrocardiographic changes were observed in some groups, 30 minutes after administration, when compared to just before local anesthesia. However there was no clinically significant QRS widening, PR interval, QT interval, or clinically adverse side effects due to these changes. It is well known that the QRS interval increases with age [21]; In our study, we also observed a slight increase according to age.
The electrocardiographic changes are proportional to the concentration of local anesthesia. It is considered that the electrocardiographic changes can be safely applied in clinical situations below the appropriate concentration.
Increases in systolic blood pressure and respiratory rate, prolonged QRS interval were observed after administration of local anesthesia. However, these symptoms disappeared completely without causing clinical adverse effects. Also, the prolonged QRS interval was less than 0.08 seconds, which was not clinically significant. No patient in any group developed nausea, vomiting, pruritus, sedation, or respiratory depression, and the mixture was especially safe for infants younger than 2 years.
Lidocaine is a short-acting drug, but its limited duration of action is less than ideal for use in many procedures. Bupivacaine has a much longer duration of action. However, owing to its slow onset, it is not an ideal sole agent for procedural analgesia in most situations [22]. So, combining the two agents in one syringe offers the patient the best effects of both drugs: the very rapid onset of lidocaine and the prolonged duration of bupivacaine. In addition, lidocaine competes with bupivacaine at the sodium channel binding site, and blocks most of the binding of bupivacaine, which is the basis for suggesting that lidocaine be used to treat cardiac toxicity caused by bupivacaine [5]. We previously investigated the effect of bupivacaine and lidocaine on patients who underwent urologic surgery in the penoscrotal and inguinal regions [23].
This was the first prospective study on the safety of a mixture of bupivacaine and lidocaine in children who underwent urologic inguinal and scrotal surgery.
In the present study, we propose that a mixture of bupivacaine and lidocaine is a safe local anesthesia for postoperative pain management. An appropriately selected dose of a mixture of bupivacaine and lidocaine can be used in children who have undergone urologic inguinal and scrotal surgery, without any clinically significant hemodynamic changes or any adverse effects.
ACKNOWLEDGMENTS
This study was supported by research grants of Pusan National University Yangsan Hospital.
References
1. Machoki MS, Millar AJ, Albetyn H, Cox SG, Thomas J, Numanoglu A. Local anesthetic wound infusion versus standard analgesia in paediatric post-operative pain control. Pediatr Surg Int. 2015; 31:1087–1097. PMID: 26407616.

2. Jarraya A, Elleuch S, Zouari J, Smaoui M, Laabidi S, Kolsi K. Postoperative analgesia in children when using clonidine in addition to fentanyl with bupivacaine given caudally. Pan Afr Med J. 2016; 24:182. PMID: 27795779.

3. Krikava I, Jarkovský J, Stourac P, Nováková M, Sevcík P. The effects of lidocaine on bupivacaine-induced cardiotoxicity in the isolated rat heart. Physiol Res. 2010; 59(Suppl 1):S65–S69. PMID: 20626222.

4. Bamigboye AA, Hofmeyr GJ. Local anaesthetic wound infiltration and abdominal nerves block during caesarean section for postoperative pain relief. Cochrane Database Syst Rev. 2009; (3):CD006954. PMID: 19588413.

5. Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97:534–540. PMID: 12873949.

6. Evans WN, Acherman RJ, Mayman GA, Rollins RC, Kip KT. Simplified pediatric electrocardiogram interpretation. Clin Pediatr (Phila). 2010; 49:363–372. PMID: 20118092.

7. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–1625. PMID: 16698416.

8. American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012; 116:248–273. PMID: 22227789.
9. Ruggiero A, Barone G, Liotti L, Chiaretti A, Lazzareschi I, Riccardi R. Safety and efficacy of fentanyl administered by patient controlled analgesia in children with cancer pain. Support Care Cancer. 2007; 15:569–573. PMID: 17146653.

10. Jarzyna D, Jungquist CR, Pasero C, Willens JS, Nisbet A, Oakes L, et al. American Society for Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011; 12:118–145.e10. PMID: 21893302.

11. Aubrun F, Langeron O, Heitz D, Coriat P, Riou B. Randomised, placebo-controlled study of the postoperative analgesic effects of ketoprofen after spinal fusion surgery. Acta Anaesthesiol Scand. 2000; 44:934–939. PMID: 10981569.

12. Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012; 172:425–430. PMID: 22412106.
13. Sahgal N, Khirwadkar R, Banerjee A. Single-dose intravenous paracetamol or propacetamol for prevention or treatment of postoperative pain. Br J Anaesth. 2011; 107:638. author reply 638-9. PMID: 21903646.

14. Ekman EF, Wahba M, Ancona F. Analgesic efficacy of perioperative celecoxib in ambulatory arthroscopic knee surgery: a double-blind, placebo-controlled study. Arthroscopy. 2006; 22:635–642. PMID: 16762702.

15. Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth. 2008; 101:700–704. PMID: 18716003.

16. Chang SH, Lee HW, Kim HK, Kim SH, Kim DK. An evaluation of perioperative pregabalin for prevention and attenuation of postoperative shoulder pain after laparoscopic cholecystectomy. Anesth Analg. 2009; 109:1284–1286. PMID: 19641054.

17. Laskowski K, Stirling A, McKay WP, Lim HJ. A systematic review of intravenous ketamine for postoperative analgesia. Can J Anaesth. 2011; 58:911–923. PMID: 21773855.

18. Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008; 95:1331–1338. PMID: 18844267.

19. Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, et al. Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth. 2011; 58:22–37. PMID: 21061107.

20. Taddio A, Stevens B, Craig K, Rastogi P, Ben-David S, Shennan A, et al. Efficacy and safety of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. 1997; 336:1197–1201. PMID: 9110906.

22. Lee JY, Jo YY. Attention to postoperative pain control in children. Korean J Anesthesiol. 2014; 66:183–188. PMID: 24729838.

Table 1
Patients' characteristics
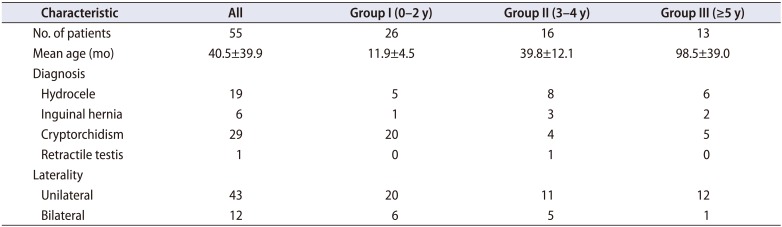
Table 2
Hemodynamic changes (blood pressure, pulse rate, respiration rate) between pre-injection and post-injection (30 min, 60 min)
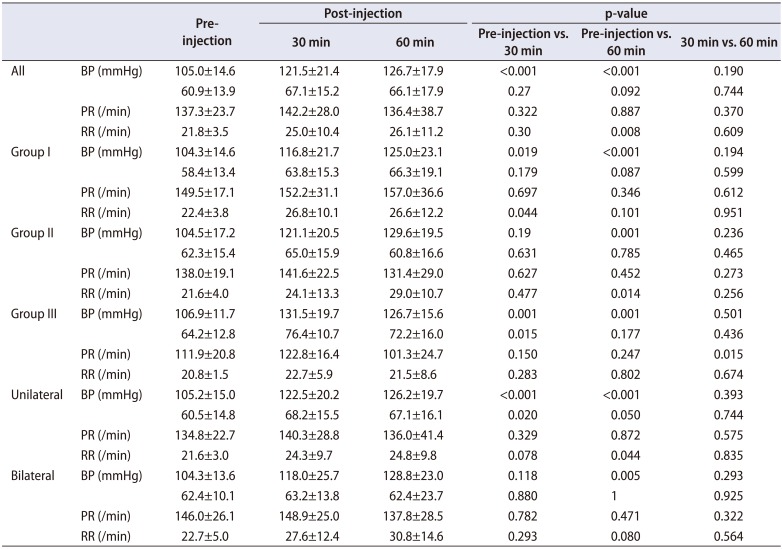
Table 3
Electrocardiographic changes (PR interval, QRS interval, QT interval) between pre-injection and post-injection (30 min, 60 min)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download