1. Rogo-Gupta L, Rodriguez LV, Litwin MS, Herzog TJ, Neugut AI, Lu YS, et al. Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol. 2012; 120:1105–1115. PMID:
23090529.

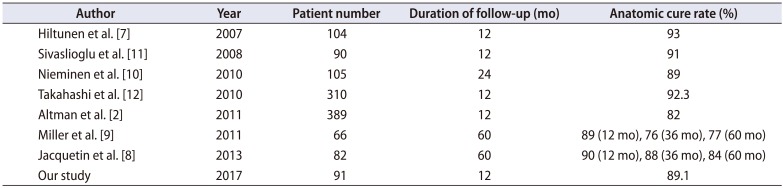
2. Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C. Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011; 364:1826–1836. PMID:
21561348.

3. Maher C, Baessler K. Surgical management of anterior vaginal wall prolapse: an evidencebased literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:195–201. PMID:
15915320.

4. Takeyama M. Basic procedures in tension-free vaginal mesh operation for pelvic organ prolapse. Int J Urol. 2011; 18:555–556. PMID:
21711397.

5. Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol. 2009; 113:367–373. PMID:
19155908.
6. Marcus-Braun N, Bourret A, von Theobald P. Persistent pelvic pain following transvaginal mesh surgery: a cause for mesh removal. Eur J Obstet Gynecol Reprod Biol. 2012; 162:224–228. PMID:
22464208.

7. Hiltunen R, Nieminen K, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol. 2007; 110:455–462. PMID:
17666627.
8. Jacquetin B, Hinoul P, Gauld J, Fatton B, Rosenthal C, Clavé H, et al. Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 5-year prospective follow-up study. Int Urogynecol J. 2013; 24:1679–1686. PMID:
23563891.

9. Miller D, Lucente V, Babin E, Beach P, Jones P, Robinson D. Prospective clinical assessment of the transvaginal mesh technique for treatment of pelvic organ prolapse-5-year results. Female Pelvic Med Reconstr Surg. 2011; 17:139–143. PMID:
22453786.

10. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010; 203:235.e1–235.e8. PMID:
20494332.

11. Sivaslioglu AA, Unlubilgin E, Dolen I. A randomized comparison of polypropylene mesh surgery with site-specific surgery in the treatment of cystocoele. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:467–471. PMID:
17901910.

12. Takahashi S, Obinata D, Sakuma T, Nagane Y, Sato K, Mochida J, et al. Tension-free vaginal mesh procedure for pelvic organ prolapse: a single-center experience of 310 cases with 1-year follow up. Int J Urol. 2010; 17:353–358. PMID:
20202001.

13. Altman D, Mikkola TS, Bek KM, Rahkola-Soisalo P, Gunnarsson J, Engh ME, et al. Pelvic organ prolapse repair using the Uphold™ Vaginal Support System: a 1-year multicenter study. Int Urogynecol J. 2016; 27:1337–1345. PMID:
26874525.

14. Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006; 195:1837–1840. PMID:
17132485.

15. Summers A, Winkel LA, Hussain HK, DeLancey JO. The relationship between anterior and apical compartment support. Am J Obstet Gynecol. 2006; 194:1438–1443. PMID:
16579933.

16. Kim MS, Lee GH, Na ED, Jang JH, Kim HC. The association of pelvic organ prolapse severity and improvement in overactive bladder symptoms after surgery for pelvic organ prolapse. Obstet Gynecol Sci. 2016; 59:214–219. PMID:
27200312.

17. Lee DM, Ryu YW, Lee YT, Ahn SH, Han JH, Yum SH. A predictive factor in overactive bladder symptoms improvement after combined anterior vaginal wall prolapse repair: a pilot study. Korean J Urol. 2012; 53:405–409. PMID:
22741049.

18. Sekiguchi Y, Kinjo M, Maeda Y, Kubota Y. Reinforcement of suspensory ligaments under local anesthesia cures pelvic organ prolapse: 12-month results. Int Urogynecol J. 2014; 25:783–789. PMID:
24318563.

19. Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG. Systematic Review Group of the Society of Gynecologic Surgeons. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011; 22:789–798. PMID:
21424785.

20. Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:315–320. PMID:
16228121.

21. Cespedes RD. Anterior approach bilateral sacrospinous ligament fixation for vaginal vault prolapse. Urology. 2000; 56(6 Suppl 1):70–75. PMID:
11114566.

22. Long CY, Lo TS, Wang CL, Wu CH, Liu CM, Su JH. Risk factors of surgical failure following transvaginal mesh repair for the treatment of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2012; 161:224–227. PMID:
22326614.

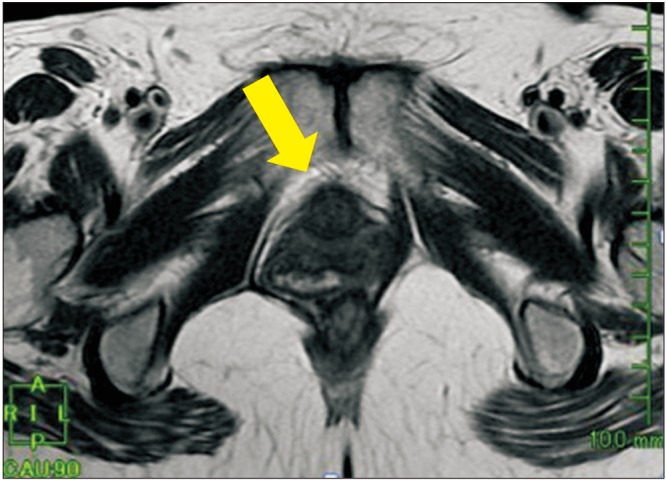
23. Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008; 115:979–984. PMID:
18503571.

24. Wong V, Shek K, Rane A, Goh J, Krause H, Dietz HP. Is levator avulsion a predictor of cystocele recurrence following anterior vaginal mesh placement? Ultrasound Obstet Gynecol. 2013; 42:230–234. PMID:
23404827.

25. Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017; 217:11–26.e3. PMID:
28188775.

26. Abbott S, Unger CA, Evans JM, Jallad K, Mishra K, Karram MM, et al. Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. Am J Obstet Gynecol. 2014; 210:163.e1–163.e8. PMID:
24126300.

27. Kuribayashi M, Kitagawa Y, Narimoto K, Urata S, Kawaguchi S, Namiki M. Predictor of de novo stress urinary incontinence following TVM procedure: a further analysis of preoperative voiding function. Int Urogynecol J. 2013; 24:407–411. PMID:
22801938.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download