Abstract
Purpose
Placement of pre-operative ureteral catheters for colorectal surgery can aid in the identification of ureteral injuries. This study investigates whether simultaneous ureteral catheterization with surgery skin preparation can minimize operating room times without increasing post-operative complications.
Materials and Methods
Patients undergoing simultaneous colorectal surgery skin preparation and placement of pre-operative ureteral catheters (n=21) were compared to those who underwent these events sequentially (n=28). Operative time-points of anesthesia ready (AR), surgery procedure start (PS), dorsal lithotomy and catheter insertion (CI) times were compared to assess for differences between groups. Complications were compared between groups.
Results
There were no differences in age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA), comorbidities, current procedure terminology (CPT) or International Classification of Diseases, 9th revision (ICD-9) codes between groups. Simultaneous catheterization saved 11.82 minutes of operative time between CI to PS (p=0.005, t-test). There was a significant difference in mean time between CI to PS (11.82 minutes, p=0.008) between simultaneous and sequential ureteral catheterization groups in a linear regression multivariate analysis controlling for age, BMI, CPT and ICD-9 codes. There were 4 complications in the simultaneous (19%) and 3 in the sequential group (11%) (p=0.68).
Conclusions
Ureteral catheterization and colorectal surgery skin preparation in a simultaneous fashion decreases the time between CI and PS without significant increase in complications. Mean time saved with simultaneous ureteral catheterization was 11.82 minutes per case. Simultaneous ureteral catheterization may be an option in colorectal surgery and may result in cost savings without additional complications.
The use of pre-operative ureteral catheters for colorectal surgery has increased in recent years, particularly with laparoscopic colorectal surgery [1]. This is despite the reported intraoperative and post-operative complications of ureteral catheterization, which include ureteral laceration/perforation, urinary tract infections (UTIs), anuria or oliguria [2]. While ureteral catheters have not been shown to reduce the incidence of ureteral injury, they do help to identify ureteral injuries, allowing for prompt intervention [3]. A retrospective review of the National Surgical Quality Improvement Participant (NSQIP) files from 2005–2011 found that when ureteral catheters are employed, there is a small increase in median operative time (44 minutes); however, no significant differences in morbidity or mortality exists [1]. Approximately 4% of abdominal/colorectal surgeries within the NSQIP database were found to have utilized ureteral catheters, with diverticular disease, radical resection, recent chemotherapy and more recent calendar use as predictors of use [1]. Prophylactic ureteral catheterization has also been described in the gynecology literature. Eighteen cases of prophylactic ureteral catheters were identified amongst 792 major gynecological procedures (2.3% utilization rate) at a single institution for a cost-analysis study [4]. At the calculated additional cost of 1,580 United States dollar (USD) for the utilization of prophylactic ureteral catheters, the profit margin for a major gynecological case for a hospital drops from 2,400 USD to 380 USD [4]; however, this does not account for the costs associated with ureteral injury. Opponents of prophylactic ureteral catheters cite the “cost factor”; however, the increased anesthesia time may also play a major role in deciding to place prophylactic ureteral catheters.
As up to 5%–15% of ureteral injuries occur during surgeries for the colon and rectum [5], prophylactic ureteral catheterization may be warranted in complicated abdominal surgeries or re-operations. However, in a recent large European retrospective analysis of 42,570 patients, there was only a 0.18% incidence of iatrogenic ureteral injury, with prior radiation and chemotherapy administration as major contributing factors [6]. In one study, the process of ureteral catheterization averages 11 minutes in both right and left laparoscopic hemi-colectomies [3]. The increase in mean operative times may be secondary to an associated delay in operating room (OR) time, such as the need to coordinate multiple surgical teams, equipment setup and communicational delays [1]. Additionally, the safety and efficacy of sequential versus simultaneous intra-operative ureteral catheterization have been previously evaluated; suggesting that simultaneous ureteral catheterization during complicated abdominal procedures can reduce mean operative times without substantial risk to the patient [7]. Our study aims to compare the anesthesia and operative time saved when simultaneous ureteral catheters are placed vs. sequential catheterization when pre-operative ureteral catheterization is required. As simultaneous ureteral catheterization with colorectal surgery skin preparation and procedure start (PS) time may increase the rate of wound infections, we expanded our post-operative complication analysis to include wound infections. Furthermore, other easily identifiable complication such as hematuria and urinary retention were also included in the analysis.
We reviewed a prospectively maintained database of a single colorectal surgeon, AG, from January 2014 to September 2015. This study was included in the colorectal surgeon's (AG) Icahn School of Medicine at Mount Sinai Institutional Review Board's list of approved studies (approval number: IF2104148). All subjects signed informed consent to participate in the study. As this was an observational study, a power calculation was not performed. Patients who underwent simultaneous colorectal surgery skin preparation and urology team placement of pre-operative ureteral catheters (n=21) were compared to a group who underwent these events sequentially (n=28). Urine cultures were not collected peri-operatively, but all symptoms of UTI, if present, were treated before concurrent surgery based on appropriate urine culture and sensitivities. All ureteral catheters were placed solely for prophylaxis and identification of ureters and not for extrinsic compression and or hydronephrosis and were presumed to have normal ureteral anatomy and did not require C-arm fluoroscopy. Of note, only 1/21 patients (4.8%) in the simultaneous group and 2/28 patients (7.1%) in the sequential group requiring prophylactic ureteral catheterization at the time of surgery had colon cancer. As such, tumor characteristics, location, or grade of pre-operative hydronephrosis were not explicitly studied. From January 2014 to December 2014, all pre-operative ureteral catheters were placed sequentially. All ureteral catheter placements were performed by the urology team (residents, post graduate year [PGY] 2 to 5) and were placed bilaterally. Sequential ureteral catheterization consisted of cystoscopy and bilateral ureteral catheter placement (5 or 6 French whistle tip catheters) followed by Foley catheter insertion (CI) (14 or 16 French) based on product availability at the time of procedure. The patient was then completely re-prepped and re-draped for colorectal surgery abdominal incision. From January 2015 to September 2015, pre-operative ureteral catheters were placed simultaneously. In this scenario, the field for cystoscopy as well as the surgical field was prepped simultaneously. Cystoscopy and ureteral catheterization was then performed at the same time as abdominal incision time after a surgical time-out. In this simultaneous scenario, a small-time difference between cystoscopy/ureteral stent placement and colorectal skin incision may be accounted for by a small delay from the start of cystoscopy to actual ureteral catheterization. Placement of ureteral catheters did not increase pre-established duration of peri-operative antibiotics for colorectal surgery. Demographic information such as age, sex, American Society of Anesthesiologists (ASA) score, body mass index (BMI), comorbidities such as diabetes, hypertension and coronary artery disease, diagnosis (by International Classification of Diseases, 9th revision, ICD-9 code) and procedure (by current procedure terminology [CPT] code) were collected by chart review. Additional medical characteristics such as prior chemoradiation, prior abdominal surgery or abdominal radiation were also collected by chart review. Operative timepoints included anesthesia start (AS), anesthesia ready (AR), surgery PS, dorsal lithotomy (DL), CI, procedure end, anesthesia end and total anesthesia time were collected from OR records which were independently recorded and maintained by a single circulating nurse. The number of additional operating staff was unchanged in either arm as all existing OR staff was fully trained in acquisition and preparation of cystoscopy. Patients with missing records, unplanned/intraoperative ureteral catheterization, one-sided catheterization or emergency surgeries were excluded. Thirty-day complication rates were collected by examining the discharge summaries and 30-day post-operative visit notes. We then calculated mean values between these timepoints (AR-PS, AR-CI, DL-PS, CI-PS) between simultaneous and sequential catheterization groups using a two-tailed t-test. Age, BMI, CPT and ICD-9 codes were chosen as independent variables for a multivariate analysis as these are each individual factors which may contribute to increased operative time and peri-operative complications. Multivariate analysis using linear regression was performed to evaluate the effect of simultaneous vs. sequential ureteral catheter placement on the observed differences in operative timepoints (AR-PS, AR-CI, DL-PS, CI-PS, dependent variables) while controlling for age, BMI, CPT and ICD-9 codes (independent variables). The p-value significance was placed at 0.05 as per convention. Statistics were calculated using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA).
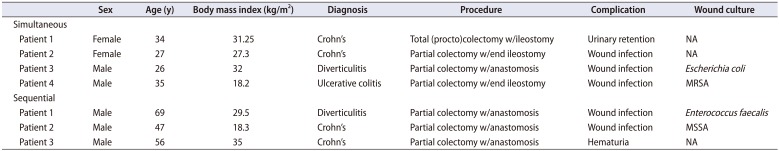
There were no differences in age, gender, BMI, ASA, comorbidities, primary CPT or ICD-9 codes between the two groups (Table 1). There were also no differences in factors which may contribute to a hostile abdomen, including chemotherapy, prior abdominal surgery or radiation between groups (Table 1). The mean AR-PS time was 24.95 and 31.53 minutes (p=0.102), mean AR-CI time was 22.81 and 17.57 minutes (p=0.205), mean DL-PS time was 21.90 and 29.00 minutes (p=0.06) and mean CI-PS was 2.14 and 13.96 minutes (p=0.005) for the simultaneous and sequential groups respectively (Table 2). Simultaneous ureteral catheterization saved 11.82 minutes of operative time between CI to PS (p=0.005, t-test). Simultaneous ureteral catheterization was associated with a significant difference in CI to PS time in a multivariate analysis (p=0.008; 95% confidence interval, −22.5 to −3.75 minutes) (Table 3). There were 4 complications in the simultaneous group (19%, 3 wound infections, 1 urinary retention) and 3 complications in the sequential group (11%, 2 wound infections, 1 prolonged hematuria), none greater than Clavien II (p=0.68) (Table 4). There appeared to be a proportional increase in wound infections in the simultaneous group (3/21, 14.3%) vs the sequential group (2/28, 7.1%), however, this was not statistically significant (p=0.329). There were no complications which resulted in ureteral or upper tract damage from stent placement in either group, either immediate or delayed.
Prophylactic pre-operative ureteral catheterization is used in many different fields including general surgery, colorectal and gynecological procedures. This has become common today with the increasing use of laparoscopic surgical techniques and the loss of tactile feel that some consider crucial in avoiding urological complications such as ureteral injury. Pre-operative ureteral catheterization may also be used in difficult cases such as patients with large tumors, diverticulitis, Crohn's, fistulas, previous radiation therapy and or re-operations [78]. As the reported incidence of ureteral injury varies widely, with some reporting 1% and others as high as 7% [2], some surgeons will selectively choose to utilize pre-operative ureteral catheters for patients who are at an increased risk of ureteral injury. Opponents of pre-operative ureteral catheterization quote the low incidence of ureteral injury, possibility of iatrogenic injury from the catheterization itself, increased financial burden to the healthcare system, decreased profit margin, and increased anesthesia time the patient would be subjected to. The national Medicare average facility fee for placement of ureteral stents (CPT 52332) averaged 1,254.53 USD in 2016 [9]. Regardless, when pre-operative ureteral catheters are utilized, the goal is to maximize efficiency while preserving safety. In our study, there were no ureteral injuries in either group. It is important to note that despite not having any ureteral injuries identified in our study, our case numbers are small and reflect a single surgeon's experience. Collectively, the risks and benefits of prophylactic ureteral catheter placement are still hotly debated and as such, being examined in this study.
Recently, Pokala et al. [7] have designed a randomized controlled study to compare the time saved with simultaneous (n=12) versus sequential (n=12) placement of pre-operative stents for difficult colorectal surgeries as well as a safety profile study in regard to UTIs. The authors found an approximate 19-minute time difference between the two with no differences in rates of UTI. Our study aimed to ask the same question but with the added investigation of whether simultaneous ureteral catheter placement increases the rate of wound infection and other complications. Although we did not find a statistically significant difference in overall complications between groups, we did note a proportional increase in wound infections in the simultaneous group; however, larger numbers in future studies are required to tease out this relationship.
Strengths of our study include higher numbers in each group (21 in simultaneous, 28 in sequential) as well as analyzing multiple complications as compared to the only randomized trial which showed that similarly, timed saved with no increase in UTI complications. Limitations of this study are that this is a non-randomized controlled study raising the possibility of selection bias. Patients that were anticipated to have higher morbidities may have been chosen to have the ureteral catheters placed sequentially as the safety profile of that procedure has already been well established. However, this bias is limited by the fact that all cases performed before January 2015 were placed in a sequential manner and all cases after January 2015 were done in a simultaneous manner regardless of the patient's co-morbidities/prior surgery status. This is even in complex colorectal cases in the inflammatory bowel disease populations that frequently involve reoperations in a hostile abdomen. An additional limitation is that since the ureteral catheters were placed by different urology residents varying from PGY2 to PGY5, it is possible that the observed time saved may be skewed towards more time saved with more experienced urology residents and less time saved with more novice urology residents. Unfortunately, this study did not take PGY of urology resident into account. Additionally, subjective ease of stent placement was not assessed but would be difficult to assess and analyze across training years. Of note, none of the prophylactic ureteral catheter placements in either group required additional manipulation for placement (i.e., usage of hydrophilic or sensor wires and or ureteroscopy) and as such, have been presumed to be straight-forward placements. Future studies may evaluate urology year of training and stratification of the analysis to determine if time saved is dependent on experience.
An increase in wound complications would be the feared outcome in simultaneous ureteral catheter placement alongside colorectal surgery skin prep and incision as there is an increase risk of contamination of the two surgical fields. We did not observe a statistically significant increase in overall complications between groups but this could be secondary to an extensive “colon bundle” protocol used on all colorectal patients, which includes chlorhexidine bath, pre-operative antibiotics, pre-operative shaving of body hair, complete switch of instruments and re-draping for abdominal closure and a betadine wash of fascia [10]. The overall wound infection rate was low in this study, but proportionally, there were more patients within the simultaneous group that had wound infections (14.3%) vs. sequential group (7.1%), however, further studies with larger numbers are needed to confirm these results.
Nonetheless, our study shows an average of 11.82 minutes saved per case when ureteral catheters are placed simultaneously with colorectal surgery skin preparation/abdominal incision vs. sequential ureteral catheter placement (as represented by CI to PS time, Table 2) in a multivariate analysis, which can account to significant cost savings. Regardless, there continue to be obstacles which may prevent further extension of these savings, primarily, that simultaneous ureteral catheterization requires coordination between multiple groups, including OR staff, anesthesiology, colorectal surgery and urology teams. A major obstacle is the coordination of teams and their arrival to the OR to minimize waiting times. Anecdotally, the urology team has been called into the room on multiple occasions to help place ureteral catheters before the patient is anesthetically ready or positionally ready, increasing the waiting time by the urologists. The study initially included the time when the urology resident entered the room and an analysis was attempted in regard to “urology in room” time to CI time. However, records were incomplete and frequently, “urology in room” time was not recorded/colorectal surgery room time was listed instead, and as such, this sub-analysis was not performed. DL time was instead used as a proxy for Urology in room time. This could potentially be rectified if a prospective study was performed.
Equipment preparedness by the OR ancillary staff may also contribute to time wasted when malfunctioning or mismatched equipment is initially used. Our institution uses two different and non-interchangeable cystoscope trays. Occasionally, an equipment for the cystoscopy trays are brought down and are incompatible and it is not until the patient is already under anesthesia and draped that the mismatched equipment is noted, thus affecting our AS and AR time-points. As our study has found, “time saved is money saved” and as such, a protocol needs to be put into place to ensure that the proper equipment is utilized and better coordination between anesthesiology, colorectal surgery and urology teams to narrow the window of time that the patient may be getting anesthesia. A proper timeout can usually catch these problems before they occur; however, that is also dependent on the right equipment being brought into the room as dictated by the equipment card.
Finally, this study does not delve into a full cost analysis, instead, choosing only to describe the cost savings based on the common figure of 62 USD /minute to run an OR [11], which can account to savings of 731.60 USD per case. This figure is likely higher in 2017 monetary terms and may be drastically different when different hospitals are studied in that higher volume centers may have faster turnovers and thus, be able to reduce the minute-cost value. As services were performed by urology residents under the supervision of an attending urologist on record, the individual billing policies of individual surgeons were not included or analyzed in this study. Additionally, with the 2016 Medicare facility fee of 1,254.53 USD for temporary ureteral stent insertion [8], simultaneous ureteral catheterization with colorectal skin prep can help to partially negate the added costs of prophylactic ureteral catheter placement.
Ureteral catheter placement and colorectal surgery skin preparation in a simultaneous fashion decreases the time between ureteral CI and procedure start without a significant increase in post-operative complications. There was no statistical difference of post-operative complications between the two groups with a trend toward increased wound infections in the simultaneous group; however, all wound complications were Clavien II or less. The mean time saved with simultaneous ureteral catheterization equates to 11.82 minutes per case. In situations where prophylactic ureteral catheterization is required or requested, performing it in a simultaneous fashion with colorectal skin incision can partially negate the added costs of cystoscopy/ureteral stenting without a significant increase in post-operative complications.
ACKNOWLEDGMENTS
We would like to acknowledge Dr. Rollin Say (Department of Urology, Icahn School of Medicine at Mount Sinai) for providing statistical support for this manuscript.
References
1. Speicher PJ, Goldsmith ZG, Nussbaum DP, Turley RS, Peterson AC, Mantyh CR. Ureteral stenting in laparoscopic colorectal surgery. J Surg Res. 2014; 190:98–103. PMID: 24656474.

2. Leff EI, Groff W, Rubin RJ, Eisenstat TE, Salvati EP. Use of ureteral catheters in colonic and rectal surgery. Dis Colon Rectum. 1982; 25:457–460. PMID: 7094783.

3. Nam YS, Wexner SD. Clinical value of prophylactic ureteral stent indwelling during laparoscopic colorectal surgery. J Korean Med Sci. 2002; 17:633–635. PMID: 12378014.

4. Fanning J, Fenton B, Jean GM, Chae C. Cost analysis of prophylactic intraoperative cystoscopic ureteral stents in gynecologic surgery. J Am Osteopath Assoc. 2011; 111:667–669. PMID: 22182952.
5. Delacroix SE Jr, Winters JC. Urinary tract injures: recognition and management. Clin Colon Rectal Surg. 2010; 23:104–112. PMID: 21629628.

6. Eswara JR, Raup VT, Potretzke AM, Hunt SR, Brandes SB. Outcomes of Iatrogenic genitourinary injuries during colorectal surgery. Urology. 2015; 86:1228–1233. PMID: 26368509.

7. Pokala N, Delaney CP, Kiran RP, Bast J, Angermeier K, Fazio VW. A randomized controlled trial comparing simultaneous intra-operative vs sequential prophylactic ureteric catheter insertion in re-operative and complicated colorectal surgery. Int J Colorectal Dis. 2007; 22:683–687. PMID: 17031654.

8. da Silva G, Boutros M, Wexner SD. Role of prophylactic ureteric stents in colorectal surgery. Asian J Endos Surg. 2012; 5:105–110.
9. Temporary ureteral stent placement or removal [Internet]. Chicago: American Medical Association;updated 2016. cited 2017 Nov 30. Available from: https://www.cookmedical.com/wp-content/uploads/2016/06/RG_URO_USPRRG_RE_201602.pdf.
10. Tanner J, Padley W, Assadian O, Leaper D, Kiernan M, Edmiston C. Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8,515 patients. Surgery. 2015; 158:66–77. PMID: 25920911.
11. Macario A. What does one minute of operating room time cost. J Clin Anesth. 2010; 22:233–236. PMID: 20522350.

Table 1
Demographics and characteristics of groups
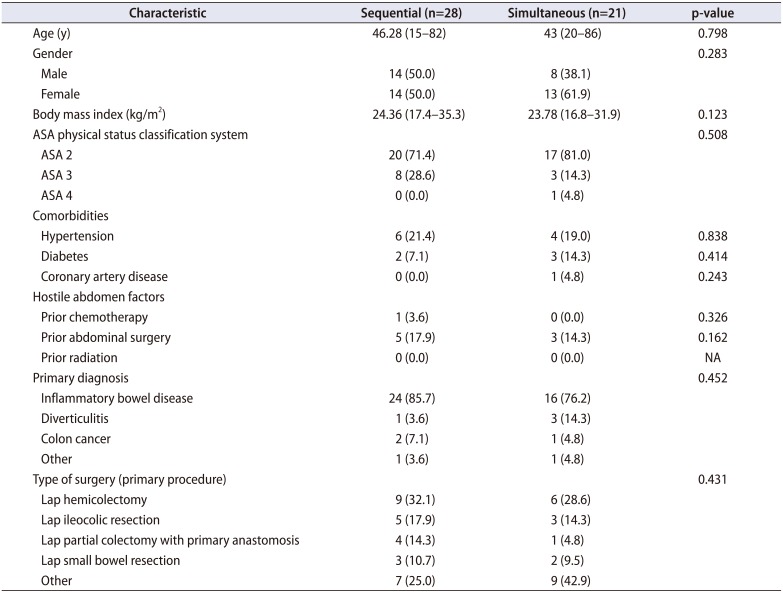
Table 2
Operative time differences between simultaneous and sequential groups (univariate analysis)
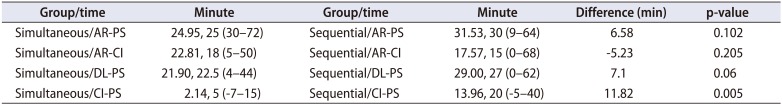
Table 3
Operative time differences between simultaneous and sequential groups (multivariate analysis [linear regression model])
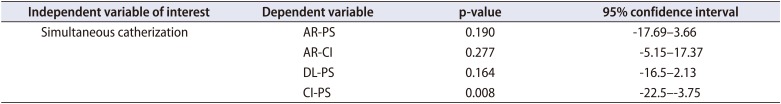
Table 4
Demographics of patients with complications after ureteral catheter placement




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download