Abstract
Vesicoureteral reflux (VUR) management must be tailored based on the risk for further infections and renal scarring, gender, likelihood of spontaneous resolution, and parental preferences. Because we now understand that sterile VUR is benign and most reflux spontaneously resolves over time, the initial approach in majority of children is non-surgical with continuous antibiotic prophylaxis (CAP) and correction of bladder and bowel dysfunction. Despite increasing utilization of CAP over the past four decades, the efficacy of antibiotic prophylaxis has been questioned due to conflicting results of studies plagued with design flaws and inadequate subject sample size. The Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) trial, which was designed to address many of the limitations from previous studies, provided much needed answers. In this review, we sought to describe the controversy surrounding VUR management, highlight the results of RIVUR trial, and discuss how the RIVUR findings impact our understanding of CAP in the management of VUR.
Vesicoureteral reflux (VUR) is the retrograde flow of urine from the bladder to the upper urinary tract during urine storage and/or emptying. It is an important risk factor for renal scarring in children who present with urinary tract infection (UTI). There is a high prevalence of reflux in children with UTI less than 5 years of age with an estimated incidence of 25%–40% [1]. Among infants less than 1 year of age presenting with UTI, incidence of reflux is as high as 70%. This incidence declines with age [2].
Multiple factors contribute to VUR. Primary reflux is presumed to arise from abnormal ureteric bud formation leading to abnormal ureterovesical junction flap valve submucosal tunnel mechanism [3]. Functional (e.g., bladder bowel dysfunction and neurogenic bladder) and anatomic outlet obstruction (e.g., posterior urethral valve) abnormalities of the lower urinary tract can also overwhelm the normal anti-reflux mechanism, resulting in secondary reflux [4].
Diagnostic modalities of VUR include voiding cystourethrography (VCUG). Contrast VCUG is the gold standard modality, but it has risks, including the need for bladder catheterization, radiation exposure, and possible introduction of infection. Radionuclide cystography is associated with less radiation exposure but lacks associated anatomical details such as periureteral diverticulum and urethral interrogation in boys. The specificity and sensitivity for VUR diagnosis is lower in radionuclide cystography compared to VCUG [5]. Although the American Academy of Pediatrics recommends renal bladder ultrasound to be performed as an initial screening modality in children with UTI and possible VUR, ultrasound has low sensitivity and poor negative predictive value for determining reflux [6].
Five grades of VUR, as determined by contrast VCUG, are used to prognosticate the behavior of disease and reflux resolution [7]. In a longitudinal study of 2,462 patients diagnosed with reflux, the grade distribution was: 6% grade I, 28% grade II, 51% grade III, 11% grade IV, 4% grade V [8]. Although fairly reproducible, there can be considerable inter-observer variability in reflux grading [9].
The majority of VUR resolves spontaneously. Bladder dynamics stabilize, and the ureterovesical junction remodels as the intramural ureter progressively elongates with bladder growth over time. For children presenting at birth, the probability of spontaneous resolution of primary reflux is inversely proportional to the initial grade, but additional factors significantly impact the resolution rates, including age at presentation, mode of clinical presentation (prenatal hydronephrosis/sibling screening vs. UTI), gender, laterality, and ureteral anatomy. Nomograms were proposed for predicting VUR resolution, taking into account the aforementioned factors (Fig. 1) [8]. Several reports have also suggested that voiding dysfunction or impaired bladder dynamics negatively impact the resolution of reflux [101112].
The primary concern of VUR is the risk of recurrent pyelonephritis and secondary long-term clinical consequences of renal scarring, including chronic kidney disease, hypertension, and complications of pregnancy. Although there have been suggestions of “water-hammer” renal damage from high-grade reflux of sterile urine against the renal papilla, this theory has not been demonstrated clinically [13]. It is parenchymal renal infection that is clearly associated with postinfectious renal scarring, which can be assessed by dimercaptosuccinic acid (DMSA) scintigraphy. There is debate whether cortical defects seen on DMSA scintigraphy originates from congenital dysplasia versus true postinfectious scarring [14].
Pediatric urologists utilize a wide array of approaches for management of VUR, including prophylactic antibiotics for infection prevention, treatment of bladder dysfunction, endoscopic injection of bulking agents, and ureteroneocystostomy (open and laparoscopic). Historically, children with any degree of VUR were thought to be under significant risk of long-term sequelae and underwent definitive surgical intervention with ureteroneocystostomy. Because we now understand that sterile reflux is benign and that the majority of reflux spontaneously resolves over time, reflux management is now individualized based on the risk for further infections and renal scarring, gender, likelihood of spontaneous resolution, and parental preferences.
For the majority of patients, the initial approach is non-surgical with prophylactic antibiotics and correction of bladder and bowel dysfunction. Surgical intervention is reserved for those in whom continuous antibiotic prophylaxis (CAP) is ineffective at preventing recurrent UTIs or in those who have persistent reflux at an older age with long-term concern for further renal damage.
Despite increasing utilization of CAP for the past 4 decades, the efficacy of CAP has been questioned. Several prospective randomized controlled trials from 2006 to 2008 failed to demonstrate the superiority of CAP in UTI prevention compared to observation alone [15161718]. Although studies by Craig et al. [19] and Brandstrom et al. [20] did reveal efficacy of CAP, the benefits were modest (absolute risk reduction of only 6%) and limited to girls less than 2 years of age with grades III and IV reflux, respectively. Importantly, these studies were plagued with study design limitations, including small sample size [1516171820], lack of placebo controls or blinding [1516171820], inclusion of patients without reflux [1519], and inconsistent urine collection methods for determining UTI [16171820]. The studies did not distinguish between febrile and nonfebrile UTIs, and there was reliance on unsubstantiated local readings of VCUG. In addition, none of the studies evaluated patient and family compliance to administering CAP.
The Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) trial, which was funded by the National Institute of Diabetes and Digestive and Kidney Disease, was designed to address many of the limitations from previous studies that examined the controversy surrounding the role of CAP in VUR management [21].
Nineteen centers across the United States from a variety of clinical settings enrolled 607 children 2 to 71 months of age. Children diagnosed with grades I–IV reflux after a first or second febrile or symptomatic UTI were randomized to trimethoprim-sulfamethoxazole prophylaxis or placebo that was identical in color, taste, smell, and consistency. Children with index infection occurring >112 days before randomization and other coexisting urological anomalies and relevant medical conditions were excluded. Providers and parents were double blinded to the study drug. Urine specimens were collected via catheterization or suprapubic aspiration among non-toilet-trained children, and clean voided specimens were obtained from toilettrained children. Bagged specimens were not permitted. Index and outcome infections met stringent diagnostic criteria, including evidence of pyuria on urinalysis, cultureproven infection, and fever (≥38℃) or urinary tract symptoms within 24 hours before or after urine collection. Bladder and bowel dysfunction was assessed according to standardized measures. Renal DMSA scintigraphy was performed at baseline and after 1 and 2 years. Two pediatric nuclear-medicine physicians interpreted DMSA scans using stringent standardized criteria. The primary outcome was the effectiveness in CAP in preventing UTI recurrence, and secondary outcomes included renal scarring, antimicrobial resistance, and treatment failure (defined by 2 febrile recurrences, 1 febrile and 3 symptomatic recurrences, 4 asymptomatic recurrences, or new or worsening kidney scarring).
Approximately 81% of patients had grades II and III reflux, 11% had grade I, and 8% had grade V reflux. Over half (56%) of patients presented with bladder and bowel dysfunction. There was very stringent follow-up and high level of adherence. However, almost a third of study participants discontinued the drug and were withdrawn from the analysis (91 of 302 children in treatment group and 76 of 305 children in placebo group).
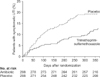
After 2 years of follow-up, the treated (CAP) group had a 50% lower risk of UTI recurrence (hazard ratio [HR], 0.50; 95% confidence interval [CI] ,0.34–0.74). Treatment reduced absolute risk of recurrence by 12%. The investigators calculated that eight non-UTI children would need treatment for 2 years for one episode of febrile or symptomatic UTI prevention. The difference in recurrence rates between the treated and placebo group widened progressively over time (Fig. 2). Interval between trial enrollment and 10% incidence of recurrence was 336 days in the treated group versus 106 days in the placebo group. Treatment reduced risk by 79% (HR, 0.21; 95% CI, 0.08–0.58) in children with bowelbladder dysfunction and 39% (HR, 0.41; 95% CI, 0.26–0.64) in children presenting with febrile or symptomatic index infection. There was increased antimicrobial resistance among treatment group with first febrile or symptomatic recurrence with Escherichia coli compared to placebo counterparts (63% vs. 19%, p<0.001).
After years of uncertainty regarding the efficacy of antibiotic prophylaxis, the RIVUR study demonstrated that CAP decreased the risk of recurrent UTI in patients with grades I–IV reflux, particularly in those with history of febrile index UTI and bladder and bowel dysfunction.
Although the study population was mostly representative of the population of patients seen clinically in terms of age and reflux grade, there was a significant discrepancy between males and females. Females represented 92% of the RIVUR study population, although the prevalence in population seen clinically is closer to 80% [8].
Given the stringent follow-up and high adherence rates, there are concerns that results of the RIVUR trial may not translate well to clinical practice. In RIVUR, 77% of parents reported administering the study medication at least 75% of the time and 85% reported administering study medication at least 50% of the time. Copp et al. [22] previously reported that only 40% of children take CAP at least 80% of time, raising concerns whether this decreased rate of medication adherence would still provide efficacy in real-life clinical practice.
In light of the study findings, the RIVUR Trial investigators suggested that the 2011 AAP Guidelines of not routinely obtaining a VCUG after the first UTI “warrant reconsideration” [21]. The evidence supporting CAP strengthens the argument for early diagnosis and treatment. Nonetheless, the RIVUR study did not definitively address the issue of screening for reflux after initial UTI. The objective of RIVUR was not to determine when a child with a UTI should be screened for reflux. The ongoing CUTIE (Careful Urinary Tract Infection Evaluation) study may shed further light into the matter [23].
The RIVUR trial failed to reveal between-group differences in the incidence of new renal scarring, whether in terms of proportion of children (6% and 7%) or renal units (4% vs. 4%) [24]. While the Swedish trial did show benefit of CAP in reducing new renal scarring for girls less than 2 years of age with grades III–IV reflux [20], other recent randomized studies failed to reveal the efficacy of CAP in reducing risk of renal scarring [15161719]. However, none of these studies, including the RIVUR trial, were powered to study the efficacy of CAP in renal scarring prevention. Hence, the results cannot be interpreted as conclusive evidence against the role of CAP in renal scarring prevention. It has been estimated that 8,000 patients would be required for such an analysis [25].
In addition, the lack of new renal scarring found in the RIVUR study may be a reflection of extremely close follow-up and treatment by the physicians, nurse coordinators, and families. The families were repeatedly educated to assess for signs and symptoms of UTI. Urine cultures were obtained within 48 hours of onset of the febrile episodes in all children. The aggressive follow-up and treatment may have prevented the onset of some pyelonephritis episodes, which would have otherwise led to scarring. The lack of difference in renal scarring between the treatment and placebo groups may suggest the possibility of managing children with reflux off of antibiotics with very close and careful follow-up. However, such an approach is likely unrealistic in real-life clinical practice [25].
Two meta-analyses studying the efficacy of CAP have been published since the RIVUR trial [2627]. The first meta-analysis by Wang et al. [26] included 8 randomized, controlled trials [1516171819202128]. Pooled results demonstrated that CAP significantly reduced the risk of recurrent febrile or symptomatic urinary tract infection (pooled odds ratio [OR], 0.63; 95% CI, 0.42–0.96). If UTI occurred, there was an increase in the risk of antibiotic resistant organism (pooled OR, 8.75; 95% CI, 3.52–21.73). There was no decrease in new renal scarring or difference in reported adverse events. de Bessa et al. [27] analyzed 7 randomized, controlled trials comparing CAP and no prophylaxis/placebo in children with reflux [151617192021]. Analysis prior to RIVUR trial revealed benefit only to children with high-grade reflux, but addition of data from RIVUR study revealed pooled data that supports CAP in all children with reflux. As discussed previously, the studies included in these meta-analyses have significant flaws, so the results must be interpreted with caution.
The benefits of CAP must be weighed against the proven risk of increased bacterial resistance and drug related side effects [2930]. Providers should also be aware of suggested but uncertain effects of long-term antibiotic exposure to children. Early-life antibiotic exposure has been associated with increased adiposity in animal models, mediated through the gut microbiome alteration. Although short-term antibiotic exposure within the first 6 months of life did not reveal increase in weight gain through 7 years of age, no studies have investigate the effects of long-term CAP with regards to weight gain [31]. Several studies report prenatal or early-life exposure to antibiotics may slightly increase the risk of childhood asthma [32]. A prospective study suggests association between antibiotic use and inflammatory bowel disease in childhood, although causality was not proven [33].
Our understanding of the relationship between anatomic VUR, bladder bowel dysfunction and UTI has shed much insight into the factors resulting in renal parenchymal scarring and the associated long-term chronic health issues. The armamentarium of therapeutic approaches in managing VUR continues to expand and improve, including the advances in surgical options such as endoscopic subureteric injection of bulking agent and innovative ureteroneocystostomy techniques. CAP has been demonstrated to reduce the UTI recurrence risk and will play a critical role in UTI prevention in the care of children with VUR since the majority will resolve reflux without surgery over time. A well-designed study such as RIVUR has provided much needed answers, but designing and executing such studies are expensive and time consuming. For these reasons, critical questions such as long-term renal scarring prevention and other side effects of CAP continue to remain beyond our reach. The modern management of VUR now has a much stronger scientific foundation on which to build our decisions; however, it still remains a clinical “Art” of incorporating many interdependent variables, especially that of parents’ concerns and the realistic assessment of compliance.
Figures and Tables
Fig. 1
VUR resolution nomogram tables. Predicted rates of cumulative annual spontaneous resolution of primary VUR and 95% confidence intervals tabularized and expressed as percentage of cases. Resolution rates are shown for boys with unilateral or bilateral reflux and girls with unilateral reflux (A), and for girls with bilateral reflux (B). Adapted from Estrada et al. J Urol 2009;182:1535-41 [8], with permission of Elsevier Inc.

Fig. 2
Continuous antibiotic prophylaxis (trimethoprim-sulfamethoxazole) versus placebo, time to symptomatic urinary tract infection in Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) Trial. UTI, urinary tract infection. Adapted from RIVUR Trial Investigators., et al. N Engl J Med 2014;370:2367-76 [21], with permission of Massachusetts Medical Society.
References
1. Tullus K. Vesicoureteric reflux in children. Lancet. 2015; 385:371–379.
2. Baker R, Barbaris HT. Comparative results of urological evaluation of children with initial and recurrent urinary tract infection. J Urol. 1976; 116:503–505.
3. Mackie GG, Stephens FD. Duplex kidneys: a correlation of renal dysplasia with position of the ureteric orifice. Birth Defects Orig Artic Ser. 1977; 13:313–321.
4. Khoury AE, Bägli DJ. Vesicoureteral reflux. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 11th ed. Philadelphia: Saunders;2016. p. 3138–3139.
5. Gordon I, Peters AM, Morony S. Indirect radionuclide cystography: a sensitive technique for the detection of vesico-ureteral reflux. Pediatr Nephrol. 1990; 4:604–606.
6. Massanyi EZ, Preece J, Gupta A, Lin SM, Wang MH. Utility of screening ultrasound after first febrile UTI among patients with clinically significant vesicoureteral reflux. Urology. 2013; 82:905–909.
7. Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985; 15:105–109.
8. Estrada CR Jr, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA, et al. Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2,462 children. J Urol. 2009; 182:1535–1541.
9. Schaeffer AJ, Greenfield SP, Ivanova A, Cui G, Zerin JM, Chow JS, et al. Reliability of grading of vesicoureteral reflux and otherfindings on voiding cystourethrography. J Pediatr Urol. 2016; 09. 06. [Epub]. DOI: 10.1016/j.jpurol.2016.06.020.
10. Silva JM, Diniz JS, Lima EM, Vergara RM, Oliveira EA. Predictive factors of resolution of primary vesico-ureteric reflux: a multivariate analysis. BJU Int. 2006; 97:1063–1068.
11. Yeung CK, Sreedhar B, Sihoe JD, Sit FK. Renal and bladder functional status at diagnosis as predictive factors for the outcome of primary vesicoureteral reflux in children. J Urol. 2006; 176:1152–1156.
12. Van Arendonk KJ, Madsen MT, Austin JC, Hawtrey CE, Graham MM, Cooper CS. Nuclear cystometrogram-determined bladder pressure at onset of vesicoureteral reflux predicts spontaneous resolution. Urology. 2007; 69:767–770.
13. Hodson CJ, Maling TM, McManamon PJ, Lewis MG. The pathogenesis of reflux nephropathy (chronic atrophic pyelonephritis). Br J Radiol. 1975; Suppl 13. 1–26.
14. Wennerström M, Hansson S, Jodal U, Stokland E. Primary and acquired renal scarring in boys and girls with urinary tract infection. J Pediatr. 2000; 136:30–34.
15. Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006; 117:626–632.
16. Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, et al. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, non-inferiority trial. Pediatrics. 2008; 122:1064–1071.
17. Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, et al. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics. 2008; 121:e1489–e1494.
18. Roussey-Kesler G, Gadjos V, Idres N, Horen B, Ichay L, Leclair MD, et al. Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol. 2008; 179:674–679.
19. Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, Mc-Taggart SJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009; 361:1748–1759.
20. Brandström P, Jodal U, Sillén U, Hansson S. The Swedish reflux trial: review of a randomized, controlled trial in children with dilating vesicoureteral reflux. J Pediatr Urol. 2011; 7:594–600.
21. RIVUR Trial Investigators. Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014; 370:2367–2376.
22. Copp HL, Nelson CP, Shortliffe LD, Lai J, Saigal CS, Kennedy WA, et al. Compliance with antibiotic prophylaxis in children with vesicoureteral reflux: results from a national pharmacy claims database. J Urol. 2010; 183:1994–1999.
23. Tasian G, Furth S. Narrowing the focus: what we now know (and still don't know) about antibiotic prophylaxis for children with vesicoureteral reflux. Am J Kidney Dis. 2015; 65:214–216.
24. Mattoo TK, Chesney RW, Greenfield SP, Hoberman A, Keren R, Mathews R, et al. Renal Scarring in the Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) Trial. Clin J Am Soc Nephrol. 2016; 11:54–61.
25. Greenfield SP. Editorial comment. J Urol. 2015; 193:5 Suppl. 1777.
26. Wang HH, Gbadegesin RA, Foreman JW, Nagaraj SK, Wigfall DR, Wiener JS, et al. Efficacy of antibiotic prophylaxis in children with vesicoureteral reflux: systematic review and meta-analysis. J Urol. 2015; 193:963–969.
27. de Bessa J Jr, de Carvalho Mrad FC, Mendes EF, Bessa MC, Paschoalin VP, Tiraboschi RB, et al. Antibiotic prophylaxis for prevention of febrile urinary tract infections in children with vesicoureteral reflux: a meta-analysis of randomized, controlled trials comparing dilated to nondilated vesicoureteral reflux. J Urol. 2015; 193:5 Suppl. 1772–1777.
28. Williams GJ, Lee A, Craig JC. Long-term antibiotics for preventing recurrent urinary tract infection in children. Cochrane Database Syst Rev. 2001; (4):CD001534.
29. Furuya EY, Lowy FD. Antimicrobial-resistant bacteria in the community setting. Nat Rev Microbiol. 2006; 4:36–45.
30. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008; 47:735–743.
31. Gerber JS, Bryan M, Ross RK, Daymont C, Parks EP, Localio AR, et al. Antibiotic exposure during the first 6 months of life and weight gain during childhood. JAMA. 2016; 315:1258–1265.
32. Murk W, Risnes KR, Bracken MB. Prenatal or early-life exposure to antibiotics and risk of childhood asthma: a systematic review. Pediatrics. 2011; 127:1125–1138.
33. Hviid A, Svanström H, Frisch M. Antibiotic use and inflammatory bowel diseases in childhood. Gut. 2011; 60:49–54.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download