Abstract
Purpose
We aimed to investigate the current management status of urologic diseases in geriatric hospitals in South Korea.
Materials and Methods
Questionnaire surveys and in-depth person-to-person interviews were conducted at 13 hospitals within the Seoul and Incheon areas.
Results
The study was carried out from July to December 2014; 75.6% of patients (1,858/2,458) and 77.5% (779/1,031) of medical personnel responded to our survey. All surveys and interviews were performed by urology specialists, fellows, residents, or nurses. The hospitals included in the study had an average of 215.2 beds (range, 110–367), 189.1 patients (range, 90–345), and 40.2 nurses (range, 10–83). The average number of physicians was 6.2 (range, 3–11), but none of these were certified urologists. Only 4 hospitals provided consultation services for urological disorders. In total, 64% of patients had urological disorders, although only 20.7% of patients were receiving medication. Most patients were being treated using urological interventions; diapers (49.7%), indwelling catheters (19.5%), clean intermittent catheters (12.2%), and external collection urinary drainage (7.9%). However, most interventions were inadequately implemented, and only 17% of the patients had been examined by a certified urologist. Urological complications were found in 20.2% of patients, and secondary complications occurred in 18.8%. Excluding redundant cases, the total prevalence of urological complications was 39.0%.
Urologic diseases are more prevalent in geriatric hospitals than in other hospitals. Dementia, stroke, cerebral infarction, and spinal disc herniation are common diagnoses in geriatric hospitals, and these conditions cause concomitant neurogenic bladder and other voiding difficulties [12]. In addition, most patients in geriatric hospitals have difficulty walking or are bedridden [3456], which also contributes to the prevalence of urologic diseases.
To manage urologic disease properly, a urologist must be involved. Indeed, one study showed that urologists are critical in improving urinary continence after bladder training [7]. Despite this, of the 3,326 medical specialists working in geriatric hospitals in December 2013, only 38 were urologists [8]. Such a paucity of urologists leads to poor management of voiding problems. In fact, according to previous research of South Korea, 84.4% of patients in geriatric hospitals received inadequate management for urinary incontinence [9]. Improper management of voiding disorders decreases quality of life and can even exacerbate existing conditions and comorbidities in the long term. The primary goal of geriatric hospitals is not to treat acute illness, but rather to manage chronic disorders and prevent the decline of daily function. To this end, it is essential that these hospitals manage voiding disorders properly.
Recently, no field studies have been carried out into urologic disease management in South Korean geriatric hospitals. Furthermore, given that the number of geriatric hospitals has risen exponentially, and that few such institutions employ an in-house urologist, voiding disorders in geriatric hospitals may not be well managed. On a different note, data from the National Health Insurance Service (NHIS) provide limited information, because they represent medical insurance data rather than the actual state of the field. For these reasons, we aimed to assess, using a field survey, the actual management status of urologic diseases in South Korean geriatric hospitals.
We analyzed 13 hospitals, of which 2 were in Seoul and 11 were in Incheon. We conducted patient surveys and in-depth interviews with medical personnel, between January 2014 to December 2014. The surveys and person-to-person interviews were all performed by urology specialists, fellows, residents, or nurses. Basic information regarding the hospitals and patients was gathered using a written questionnaire, and interviews with medical personnel were conducted in the same way (Supplementary materials 1,2,3). Importantly, we did not gather any information that identified the patients or medical staff. The person-to-person interviews were given by the patients themselves, except when they were unable to communicate; in such cases, the interviews were given by caregivers or nurses on the patients' behalf.
This study was approved by the Institutional Review Board of Seoul National University Hospital (approval number: E-1410-080-618).
We used IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA) for statistical analysis. The following additional information was also surveyed: the availability of urological consultation and outsourced medical care, as well as the number of (1) hospital beds, (2) staffed beds, (3) medical staff members, (4) geriatric care workers, and (5) physicians (numbered according to their medical specialties). The patient assessment included medical history, history of urological diagnoses, current urogenital problems, voiding symptoms, and urological intervention. In-depth interviews with medical personnel consisted of questions about the current management of urological disorders, as well as possible strategies for improvement.
We included geriatric hospitals that were established between 2006 and 2014: 2 in Seoul and 11 in Incheon. Ten of the 13 institutions were certified geriatric hospitals; the mean hospital capacity was 215.2 beds (range, 110–367), with an average of 189.1 patients (range, 90–345) at the time of the study. Regarding healthcare staff, the hospitals had an average of 6.2 doctors (range, 3–11), and 40.2 nurses (range, 10–83). Of the 80 medical specialists across all institutes, there were no certified urologists. Only four of the hospitals (30.8%) provided routine urological consultation services, while 8 (61.5%) provided outsourced consultation on an as-needed basis (Table 1).
A total of 1,858 patients were enrolled in this study, among whom there were 358 (19.3%) in Seoul and 1,500 (80.7%) in the Incheon province. Nine hundred 2 patients (48.5%) were men, 955 (51.4%) were women, and 1 was of undetermined sex. The mean age was 69.6±15.1 years, and the average hospital stay was 10.0±9.1 months. The primary complaints upon admission were stroke (37%), dementia (26%), and gait disturbance (17%). There were also degenerative neurological disorders (8%), organic neurological disorders (6%), fractures (3%), pulmonary disease (2%), and neuropsychiatric disorders (1%). Common comorbidities were hypertension (62.0%), diabetes (49.4%), cardiac disorders (9.6%), spinal disorders (5.9%), and hepatic disorders (1.9%). Only 418 patients (22.5%) could walk unsupported; 515 (27.7%) required either a wheelchair or braces, and 252 (13.6%) required assistance from at least one person, and 644 (34.7%) were bedridden. On admission, 531 patients (28.6%) had at least one diagnosed urological disorder, such as urinary tract infection (UTI), benign prostatic hyperplasia, or neurogenic bladder.
With regard to the prevalence of urological disorders, 900 patients (48.4%) had voiding difficulty, 930 (50.1%) had urinary incontinence, and 1,190 (64%) had both conditions. Almost half of incontinence patients (45.8%) suffered severe incontinence; requiring at least five pads per day. Three hundred eighty-four patients (20.7%) were on voiding disorder-related medications, and 1,109 patients (59.7%) were managed using a urinary intervention; namely diapers, indwelling catheters, clean intermittent catheters (CICs), or External collection urinary drainage (Table 2). Only 7% of patients were managed by urologist and 83% of patient had no medical advice for voiding problems (Fig. 1).
Urologic complications related to voiding difficulty were found in 375 patients (20.2%), and 350 patients (18.8%) had secondary complications related to urological disease. The total prevalence of urological complications was 39.0%, including duplicates (Table 3).
A total of 779 medical personnel participated in our survey, with a mean age of 40.1±8.5 years (range, 22–62 years). Most participants was female (90.4%) and 2 were of unknown sex. With regard to occupation, nurses (58.3%) and geriatric care givers (27.3%) were most common. About 43.5% of medical personnel recognized “over half” of patients in geriatric hospitals has urologic problem, but only 29.8% were planned routinely check-up by urologist. None of the patients received care from a certified urologist employed in the same hospital. Surprisingly, 0.9% of medical personnel replied that either the patient or their personal care giver were responsible for genitourinary care. Medical personnel reported that patient's genitourinary problems were relatively well managed. However, almost all of them agreed to needs of urologist (Table 4).
From 13 geriatric hospitals in the Seoul and Incheon areas, 1,858 patients and 779 medical caregivers participated in our survey. The reply rate among patients was 75.6% (1,858/2,458), while that among medical personnel was 77.5% (779/1,031). Considering many patients in geriatric hospitals either have difficulty communicating or co-operate poorly because of their coexisting medical condition, the present study was quite well encompassing. To increase response rate, we simplified questions and sometimes discuss with patient's family and care-giver. For example, we evaluated the prevalence of voiding disorders and incontinence using the following simple questions: “Have (you) experienced voiding difficulty or problems during the last 1 month?”, and “Have (you) experienced incontinence, regardless of self-will, during the last 1 month?”
We discovered several problems with the management of voiding dysfunctions in geriatric hospitals. Firstly, urinary incontinence was too often managed using urological interventions. Current literature recommend that geriatric patients be treated using behavior modification or bladder relaxant medication [21011]. Special undergarments such as diapers are only useful for patients with refractory incontinence [12]. In this study however, about a half of all admitted patients used a diaper to manage voiding problems. Secondly, the urologic interventions were not properly preformed. For instance, CICs can relieve urinary incontinence in the elderly, but they are inadequately used in geriatric hospitals. It is recommended that the CIC be used at a minimum of every 4 to 6 hours to minimize bacterial dwell time [13]; however, none of patients in the present study catheterized more than 3 times a day. Moreover, 16.2% of the patients performed inadequate external collection urinary drainage by tying a plastic bag around the penile glans, primarily to prevent diaper expenditure.
Furthermore, the incidence of complications was much higher in the present investigation than in other studies, which have reported a point prevalence of 1.5%–1.6% in longterm care facilities [1415]. In the current study, about onethird of patients experienced voiding problems related to complications, and 12.5% suffered from a UTI. Indeed, UTI is the most common bacterial infection in the elderly, and the risks of sepsis and septic shock are higher than in younger patients [16]. In addition, cognitive impairment increases UTI risk in the elderly [17], and vice versa [18]. For this reason especially, it is important that UTIs be managed properly in geriatric hospitals. The duration of urinary catheterization is a well-known risk factor for catheter-associated UTIs [19], and suprapubic catheterization prevents catheter-associated bacteremia more effectively. Despite this, 19.5% of inpatients are subjected to long-term indwelling catheterization, and most catheterized patients have an indwelling urethral catheter. On a different note, dermatitis is associated with improper management of diapers or external collection urinary drainage. Indeed, incontinence-associated dermatitis can be reduced by changing pads more often, as well as by using the proper pad type [20].
Relatedly, few urologists work in geriatric hospitals. According to the 2013 statistics of South Korea [21], only 1.6% of doctors working in geriatric hospitals were urologists, which is much lower than the average 7.5% among the eight major specialties. Indeed, gynecologists (4.5%) and practitioners of Korean medicine (6.8%) each comprised a much higher proportion. The present field study revealed that, among patients who required urological care, 83% did not receive treatment; moreover, fewer than 5% of urological disorders were diagnosed, and the diagnosis was always carried out by a nonurologist. Medical personnel agreed that more urologists were needed. Of the 779 medical personnel surveyed, 56.4% replied either “yes” or “highly required” when asked if they thought a urologist would benefit their patients. The diagnosis and management of UTIs and incontinence are complicated in the elderly population, and inadequate treatment increases patient mortality [22].
The simplest and most efficient solution to this would be to employ certified urologists in geriatric hospitals around the nation. Failing that, we believe that there are limits to a hospital's ability to outsource consultations, and that routine visits from an urologist provide a more realistic solution. In addition, including urological assessment criteria in current hospital accreditation systems, or in the Health Insurance Review and Assessment, may provide sufficient incentives to self-implement such systems. For example, The Korean Urological Association Insurance Committee suggested adding queries regarding “incontinence improvement rate,” “UTI incidence,” and “diaper usage” to the 2015 6th Korean National Health Insurance Value Incentive Program. Similarly, urological problems could be evaluated by including categories like “urinary catheterization rate,” “assessment of voiding function,” “Foley indwelling catheter rate,” and “consultation rate for urological problems”; such changes would likely improve healthcare. Furthermore, these criteria could standardize the quality of urological management in geriatric hospitals, and would probably be useful in establishing long-term medical policy.
Previously our group reported of 11 hospitals survey report within capital area [23], about knowledge and management pattern of urinary incontinence who work in geriatric hospitals. This study based on same cohort with additional 2 hospitals medical personnel and all 13 hospitals patients survey reports. The current study includes actual field data and provides insight into the current incidence of voiding disorders, as well as their management in geriatric hospitals. The data may inform medical policy decisions in future. The purpose of our study was to assess the current management of urological disorders in geriatric hospitals in South Korea, and to improve the quality of care for patients who are denied basic urological treatment. If geriatric hospitals continue improper management, the prevalence of complications will increase, leading to decreased quality of life and unnecessary suffering. More importantly, neglect of voiding disorders leads to poor hygiene, essentially stripping patients of their right to proper medical care.
Because field studies were limited to hospitals located in the Seoul-Incheon areas, our data may not accurately represent care in geriatric hospitals around the nation. On the other hand, even fewer medical specialists are employed in the provincial areas, and we therefore fear that management may be even worse there. Previous literature has shown that research based solely upon data requested from hospitals is limited, especially when assessing disease prevalence and patient management. Nonetheless, we believe that this study may provide useful reference data in the assessment of urological disorders throughout the nation.
Two-thirds of patients in geriatric hospitals suffer from urological problems and above half of these are undergoing a urological intervention; however, none of them are managed by a certified urologist. We believe that assigning more urologists will improve the management of urologic diseases in geriatric hospitals.
Figures and Tables
Fig. 1
Twenty percent of patients replied that patients take urologic diagnosis before urologic intervention. However, there was no certified urologist working in geriatric hospitals we surveyed. So, only 7% of patients that consulted by urologist in other institution were exactly take urologic examination before treatment.

Table 1
List of participating hospitals
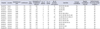
Table 2
Urologic disorder treatment patterns (n=1,858)
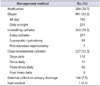
Table 3
Frequency of complications

Table 4
Medical personnel survey results (n=779)

ACKNOWLEDGMENTS
This study was supported by the Research Foundation for Korean Urological Association in 2014 (FKUA-2014-001).
References
1. Lee SH, Cho ST, Na HR, Ko SB, Park MH. Urinary incontinence in patients with Alzheimer's disease: relationship between symptom status and urodynamic diagnoses. Int J Urol. 2014; 21:683–687.
2. Jung HB, Kim HJ, Cho ST. A current perspective on geriatric lower urinary tract dysfunction. Korean J Urol. 2015; 56:266–275.
3. Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J Urol. 2011; 185:571–577.
4. Kirshen AJ. Urinary incontinence in the elderly: a review. Clin Invest Med. 1983; 6:331–339.
5. Ogama N, Yoshida M, Nakai T, Niida S, Toba K, Sakurai T. Frontal white matter hyperintensity predicts lower urinary tract dysfunction in older adults with amnestic mild cognitive impairment and Alzheimer's disease. Geriatr Gerontol Int. 2016; 16:167–174.
6. Chung RY, Leung JC, Chan DC, Woo J, Wong CK, Wong SY. Lower urinary tract symptoms (LUTS) as a risk factor for depressive symptoms in elderly men: results from a large prospective study in Southern Chinese men. PLoS One. 2013; 8:e76017.
7. Kim MS, Lee SH. Prevalence rate and associated factors of urinary incontinence among nursing home residents. J Korean Acad Nurs. 2008; 38:92–100.
8. Health Insurance Review & Assessment Service. 2013 Handbook of health insurance review & assessment service. 2014 [Internet]. Wonju: Health Insurance Review & Assessment Service;2016. cited 2016 Jul 5. Available at http://www.hira.or.kr/.
9. Lee SH, Kang JS, Kim JW, Lee SJ. Incontinence pad usage in medical welfare facilities in Korea. Int Neurourol J. 2013; 17:186–190.
10. Resnick NM. Voiding dysfunction and urinary incontinence. In : Beck JC, editor. Geriatric review syllabus: a core curriculum in geriatric medicine. New York: American Geriatrics Society;1991. p. 141–154.
11. Lee HS, Seo JT. Urinary incontinence and overactive bladder. J Korean Med Assoc. 2015; 58:886–891.
12. Resnick NM, Tadic SD, Yalla SV. Geriatric incontinence and voiding dysfunction. In : Kavoussi LR, Novick AC, Partin WA, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia (PA): W.B. Saunders;2011. p. 2204–2222.
13. Cespedes RD, Gerboc JL. Other therapies for storage and emptying failure. In : Kavoussi LR, Novick AC, Partin WA, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia (PA): W.B. Saunders;2011. p. 2186–2203.
14. Tsan L, Langberg R, Davis C, Phillips Y, Pierce J, Hojlo C, et al. Nursing home-associated infections in Department of Veterans Affairs community living centers. Am J Infect Control. 2010; 38:461–466.
15. Cotter M, Donlon S, Roche F, Byrne H, Fitzpatrick F. Healthcare-associated infection in Irish long-term care facilities: results from the First National Prevalence Study. J Hosp Infect. 2012; 80:212–216.
16. Koh H. Urinary tract infection in the elderly. J Korean Geriatr Soc. 2002; 6:243–252.
17. Caljouw MA, den Elzen WP, Cools HJ, Gussekloo J. Predictive factors of urinary tract infections among the oldest old in the general population. A population-based prospective follow-up study. BMC Med. 2011; 9:57.
18. Eriksson I, Gustafson Y, Fagerström L, Olofsson B. Urinary tract infection in very old women is associated with delirium. Int Psychogeriatr. 2011; 23:496–502.
19. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002; 113:Suppl 1A. 5S–13S.
20. Fujimura T, Makino M, Takagi M, Maki K, Murakami E, Tasaka Y, et al. The influence of incontinence on the characteristic properties of the skin in bedridden elderly subjects. Int J Dermatol. 2016; 55:e234–e240.
21. Korean Statistical Information Service. Number of medical personnel by specialized subjects [Internet]. Daejeon: Statistics Korea;2016. cited 2016 May 3. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_HIRA4K&vw_cd=&list_id=&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K1&path=#.
22. Esparcia A, Artero A, Eiros JM, Balaguer M, Madrazo M, Alberola J, et al. Influence of inadequate antimicrobial therapy on prognosis in elderly patients with severe urinary tract infections. Eur J Intern Med. 2014; 25:523–527.
23. Jang Y, Kwon BE, Kim HS, Lee YJ, Lee S, Kim SJ, et al. Knowledge and practice behaviors regarding urinary incontinence among korean healthcare providers in long-term care hospitals. Int Neurourol J. 2015; 19:259–264.
SUPPLEMENTARY MATERIALS
Scan this QR code to see the supplementary materials, or
visit http://www.icurology.org/src/sm/icurology-58-70-s001.pdf.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download