Abstract
Purpose
Rigid and flexible cystoscopies are both routinely used in female patients. Literature is conflicting whether flexible cystoscopy is less painful compared to rigid cystoscopy. The aim of this study was therefore to investigate whether using flexible cystoscopy leads to less discomfort and pain compared to rigid cystoscopy in female patients who underwent first time cystoscopy.
Materials and Methods
One hundred eighty-nine female patients, who never had undergone cystoscopy, were randomized into 2 groups: 92 patients underwent rigid cystoscopy and 97 patients flexible cystoscopy. Directly after the cystoscopy procedure all patients were asked to fill out their pain experience on a 100-mm visual analogue pain scale (VAS).
Results
Median VAS score was significantly lower for women undergoing flexible cystoscopy (0 [0–20]) compared to rigid cystoscopy (15 [0–38], p<0.001). In addition, age was inversely associated with VAS score, indicating that younger females experienced more pain (R=−0.30, p=0.001). The use of flexible cystoscopy was associated with a decrease in VAS score and remained significant after adjustment for age, sex of urologist, performing urologist and indication (standardized β=−0.17, p=0.048).
Office based cystoscopy is one of the most common procedures in daily urology practice, as it allows adequate and feasible visualization of the bladder and urogenital system. It is used in the diagnosis and follow-up of urogenital malignancies, as well as for noncancer related diagnoses. In men flexible cystoscopy is the first choice procedure in the outpatient clinic, since this method is less painful compared to rigid cystoscopy [1]. However, in women rigid and flexible cystoscopy are both still routinely used in an office based setting. The underlying theory is that both rigid and flexible instruments can easily pass the short female urethra without much discomfort. Cystoscopy, however, is an invasive procedure which can be associated with pain and discomfort [2]. Literature is conflicting whether type of cystoscopy is associated with pain in women. A number of studies have investigated pain perception and degree of discomfort in women undergoing an office based cystoscopy [234567891011]. Only in 2 of these studies, female patients were randomized for rigid and flexible cystoscopy to compare pain perception in both groups [810]. These 2 relatively small studies did not find any difference in discomfort and pain perception between rigid and flexible cystoscopy procedures. Another study demonstrated that both rigid and flexible cystoscopies were well tolerated, but the use of flexible cystoscopy was preferred by the majority of patients [9]. One large analysis of 1,320 patients showed that cystoscopy procedures were not associated with distressing levels of pain [11]. In addition, this study found that using flexible cystoscopy was associated with a lower pain level in both men and women.
The question arises whether the conflicting data in literature may be explained by the fact that all aforementioned studies varied in methodology and data collection. In addition, in both randomized controlled trials, some patients have already undergone previous cystoscopy procedures, which may influence patient's pain perception. Therefore, we investigated in a large case control study of female patients, who underwent first time cystoscopy, whether using flexible cystoscopy leads to less discomfort and pain compared to rigid cystoscopy.
This prospective study was performed over the course of 12 months at the urological outpatient clinic of the Ziekenhuis Groep Twente Hengelo, The Netherlands. All female patients were asked to participate when they had a first time cystoscopy for the indications hematuria, urinary incontinence, lower urinary tract symptoms (LUTS) and recurrent urinary tract infections. Exclusion criteria for participation were having a history of previous cystoscopy procedures, requiring other procedures apart from cystoscopy, current urinary tract infection, anatomic urethral abnormalities, presence of current pain in the pelvic region (e.g., bladder pain syndrome or interstitial cystitis), known with pain syndromes, for example vaginismus or fibromyalgia, and any analgesic use during the 24 hours before procedure.
Patients were randomized into 2 groups by choosing an envelope; by finding a note of RIGID group in the envelope, the patient underwent a rigid cystoscopy, and by finding a note of FLEX group, the patient underwent a flexible cystoscopy. Patients were not blinded for procedure. All cystoscopies were performed by one of 4 experienced urologists (2 female and 2 male). All these urologists have done more than 500 cystoscopies and could therefore be considered as experienced in this procedure. Patients were placed in a lithotomy position. Disinfection was performed with water. No lubricant, including anesthetic or antiseptic gels, was utilized [12]. Flexible cystoscopy was performed with the 16.2-Fr flexible digital chip CYF-5 cystoscope (Olympus, Tokyo, Japan) and rigid cystoscopy with the Frigid Stortz cystoscope with 30-degree lens. Both flexible and rigid cystoscopes were introduced with running NaCl 0.9% solution, using this liquid as a natural lubricant. All patients received the same real-time explanation during procedure. No prophylactic antibiotics were administrated. Of note, washing cytology was not performed during the procedure. All patients were asked to void in a small container before cystoscopy. In this way cytology could be easily performed without the risk for cytological artefacts caused by instrumentation of the urinary tract.
To objectify patient's pain experience during procedure, all patients filled out their pain experience using the 100-mm visual analogue pain scale (VAS) directly after cystoscopy. Before procedure an assisted nurse explained to the patient this scale. Patients had time to ask questions and underwent only the cystoscopy by completely understanding the VAS. When a patient asked about the expecting pain experience during procedure, the nurse answered that pain perception was individual-dependent to avoid potential bias. Immediately after cystoscopy patients were asked, by a nurse (in absence of the urologist), to record their pain experience during the procedure on a VAS.
This prospective study was performed in adherence to the Declaration of Helsinki, and all patients gave approval to participate in this study. For this study, approval of the institutional board of directors was taken.
A power analysis was performed to determine how many participants were to be included in this study. We powered this study based on the VAS score in women after cystoscopy in a previous study [8]. These data, adopting a 5% two-sided alpha and 80% power, indicated that at least 56 patients in each treatment group were needed to show a significant difference in VAS score between both treatment groups. Taking into account the possibility of 20% protocol violators and/or dropouts, inclusion of 72 subjects per group was aimed. About 144 subjects needed therefore to be enrolled in this study.
Normally distributed variables are expressed as mean±standard deviation, whereas nonnormally distributed variables are given as median (interquartile range). Differences in baseline characteristics between both treatment groups were calculated with a chi-square test for categorical data, and for continuous data with Student t-test or a Mann-Whitney U-test in case of nonnormally distributed data. To investigate whether type of cystoscopy correlated with pain experience (expressed as VAS score) univariate and multivariable linear regression analyses were performed. VAS score was logarithmic transformed to fulfill the requirement of normal distribution of the residuals for regression analysis. The multivariable linear analyses were subsequently adjusted for age, cystoscopy performing urologist, sex of the performing urologist and indication for cystoscopy. All analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA), and a 2-sided p<0.05 was considered to indicate statistical significance.
Patient characteristics are presented in Table 1. A total of 189 patients were included, of which 97 underwent flexible cystoscopy and 92 rigid cystoscopy. Overall, female patients were 58±17 years old and the most common indications, for which a cystoscopy was performed, were hematuria (29.1%), LUTS (27.5%) and recurrent urinary tract infections (26.5%). Cystoscopy had in 76 patients no effect on their pain experience and the overall median VAS score was 9 (0–25) mm. None of all patients had any pain feelings 30 minutes after procedure. Table 1 also shows the patient characteristics stratified for treatment group. Patients who underwent rigid cystoscopy, reported significantly more frequent pain compared to the flexible cystoscopy group (71.7% vs. 48.5%, p=0.001). Their pain experience, expressed as VAS score, was also significantly higher in the rigid cystoscopy group compared to the flexible cystoscopy group (15 [0–38] vs. 0 [0–20], p<0.001) (Table 1).
In addition, we investigated whether other patient characteristics were associated with their pain experience. Overall, age was inversely associated with VAS score (overall R=−0.30, p=0.001) (Fig. 1). This association was also seen in patients who underwent rigid cystoscopy (R=−0.35, p=0.004), whereas a trend was found in the flexible cystoscopy group (R=−0.23, p=0.075), likely due to the relatively small number of patients per treatment group. Indication for cystoscopy, performing urologist and sex of urologist were all not associated with pain experience (p=0.253, p=0.136, and p=0.474 respectively).
Lastly, we performed univariate and multivariable linear regression to investigate whether type of cystoscopy was associated with pain experience in female patients (Table 2). As expected, flexible cystoscopy was univariately associated with a decrease in VAS score (standardized β=−0.22, p=0.002) and remained significant after adjusted for age (standardized β=−0.23, p<0.001) (Table 2, model 2). In the final model, flexible cystoscopy was still associated with a decrease in VAS score after adjustment for age, performing urologist, sex of urologist and indication (standardized β=−0.17, p=0.048) (model 3). Moreover, age remained inversely associated with VAS score (standardized β=−0.30, p<0.001).
This study showed that in female patients, who underwent first-time cystoscopy, pain experience was significantly lower in the flexible cystoscopy group compared to the rigid cystoscopy group. We found that age was inversely associated with pain experience during cystoscopy. The association between flexible cystoscopy and pain experience remained significant after adjustment for age, cystoscopy performing urologist, sex of the urologist and cystoscopy indication.
Literature is conflicting whether type of cystoscopy is associated with pain experience. Only 2 randomized controlled trials were performed that compare flexible and rigid cystoscopy on pain experience [810]. These studies found that flexible as well as rigid cystoscopy were well tolerated in women and discomfort and pain were minimal during procedure. Clinicians should therefore perform cystoscopy in women based on their preference and skill level. In contrast to their results, we found that female patients experienced less pain using flexible cystoscope compared to rigid cystoscope.
Four reasons came to mind which may possibly explain this contrast. In both studies, some patients have already undergone previous cystoscopy procedures, which may influence patient's pain perception. Indeed, studies found that pain levels during first cystoscopy procedures were higher than those for repeated ones [1113]. Our results were based on patients with no history of previous cystoscopy treatments, to avoid a source of bias based on preconceived notions. Secondly, in our study all procedures were performed by urologists with great experience in performing cystoscopies. In the study of Gee et al. [10], a large part of the procedures was performed in a teaching setting. Despite flexible and rigid cystoscopy could be performed adequately by resident urologists, such a result is presumably dependent on good instruction and supervision [14]. Thirdly, an urethral local anesthetic (lidocaine gel or Xylocaine 2% respectively) was used in both studies, whereas this was not the case in our study. Lastly, the lack of significant differences and associations may be due to the small sample size. Gee et al. [10] performed a prospective randomized single blind 2 arm study with only 31 out of 36 participating women, to determine whether office based flexible cystoscopy was better tolerated than rigid cystoscopy in women. Although one hundred women were enrolled primarily in the study of Quiroz et al. [8], a drop out of 15% occurred.
Our study indicates that also age plays a role on pain experience. This is in accordance with an earlier study. They found a trend that age was associated with pain during cystoscopy in a large population of men and women [11]. The reason why age seems to play an important role in causing pain symptoms cannot be concluded from the present data. However, we hypothesize that indication for cystoscopy might be important. In young women, cystoscopy is performed in many cases to evaluate recurrent urinary tract infections, whereas in older women the indication for cystoscopy is more frequently to evaluate incontinence or hematuria.
In our study, per protocol, no lubricant, including anesthetic or antiseptic gels, was utilized [12]. Both the flexible and rigid cystoscopes were introduced with running NaCl 0.9% solution, used as a natural lubricant. We decided not to use any lubricant gel, because it has been suggested that lubricant gel itself could induce pain due to distension of the urethra and the sphincter [1516]. It is intriguing that 51% of our flexible cystoscopy treatment group had a VAS score of 0 mm. These results suggest that performing a flexible cystoscopy in women, except for young women, lubricant with or without anesthesiological component is not really necessary. Excluding lidocaine jelly or plain lubricant may lead to significant cost savings.
This study has strengths and limitations. A limitation of our study is that it was not performed blinded to the cystoscopical procedure. However, since all patients had no experience with the procedure, we think this might not bias our results. Another limitation is that significant more male urologists performed rigid cystoscopy procedures. Although, after adjustment for sex of performing urologist, flexible cystoscopy was still associated with a decrease in VAS score. In addition, no interaction was found between VAS score and sex of performing urologist. So, a possible (sub) conscious bias in favor of female doctors being more gentle seems to be excluded. The main strength of our study is the systematic and prospective nature of data collection that resulted in a well-phenotyped population.
We found that female patients who underwent flexible cystoscopy for the first time had a significantly lower VAS score compared to rigid cystoscopy. This association remained significant after adjustment for age, performing urologist, sex of urologist and indication for cystoscopy. Based on patient's pain experience, our study implicates that physicians may use flexible cystoscopy as first choice procedure in female patients who undergo first time cystoscopy.
Figures and Tables
Fig. 1
Association of age with VAS score, in women with pain during the procedure, stratified for flexible and rigid cystoscopy separately. In patients who underwent rigid cystoscopy VAS score was associated with age (R=−0.35, p=0.004; solid line), whereas a trend was found in patients who underwent flexible cystoscopy (R=−0.23, p=0.075; dashed line).
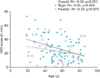
Table 1
Patients characteristics overall and stratified for study group
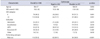
Table 2
Multivariate linear regression analyses investigating the association of flex scope with VAS score (as dependent variable) in 189 patients

References
1. Tsuchida S, Sugawara H. A new flexible fibercystoscope for visualization of the bladder neck. J Urol. 1973; 109:830–831.
2. Erkal S. Patients' experiences at home after day case cystoscopy. J Clin Nurs. 2007; 16:1118–1124.
3. Yerlikaya G, Laml T, Elenskaia K, Hanzal E, Kölbl H, Umek W. Pain perception during outpatient cystoscopy: a prospective controlled study. Eur J Obstet Gynecol Reprod Biol. 2014; 173:101–105.
4. Seklehner S, Engelhardt PF, Remzi M, Fajkovic H, Saratlija-Novakovic Z, Skopek M, et al. Anxiety and depression analyses of patients undergoing diagnostic cystoscopy. Qual Life Res. 2016; 25:2307–2314.
5. Choong S, Whitfield HN, Meganathan V, Nathan MS, Razack A, Gleeson M. A prospective, randomized, double-blind study comparing lignocaine gel and plain lubricating gel in relieving pain during flexible cystoscopy. Br J Urol. 1997; 80:69–71.
6. Goldfischer ER, Cromie WJ, Karrison TG, Naszkiewicz L, Gerber GS. Randomized, prospective, double-blind study of the effects on pain perception of lidocaine jelly versus plain lubricant during outpatient rigid cystoscopy. J Urol. 1997; 157:90–94.
7. Choe JH, Kwak KW, Hong JH, Lee HM. Efficacy of lidocaine spray as topical anesthesia for outpatient rigid cystoscopy in women: a prospective, randomized, double-blind trial. Urology. 2008; 71:561–566.
8. Quiroz LH, Shobeiri SA, Nihira MA, Brady J, Wild RA. Randomized trial comparing office flexible to rigid cystoscopy in women. Int Urogynecol J. 2012; 23:1625–1630.
9. Flannigan GM, Gelister JS, Noble JG, Milroy EJ. Rigid versus flexible cystoscopy. A controlled trial of patient tolerance. Br J Urol. 1988; 62:537–540.
10. Gee JR, Waterman BJ, Jarrard DF, Hedican SP, Bruskewitz RC, Nakada SY. Flexible and rigid cystoscopy in women. JSLS. 2009; 13:135–138.
11. Greenstein A, Greenstein I, Senderovich S, Mabjeesh NJ. Is diagnostic cystoscopy painful? Analysis of 1,320 consecutive procedures. Int Braz J Urol. 2014; 40:533–538.
12. Stein M, Lubetkin D, Taub HC, Skinner WK, Haberman J, Kreutzer ER. The effects of intraurethral lidocaine anesthetic and patient anxiety on pain perception during cystoscopy. J Urol. 1994; 151:1518–1521.
13. Ellerkmann RM, Dunn JS, McBride AW, Kummer LG, Melick CF, Bent AE, et al. A comparison of anticipated pain before and pain rating after the procedure in patients who undergo cystourethroscopy. Am J Obstet Gynecol. 2003; 189:66–69.
14. Nguyen CT, Babineau DC, Jones JS. Impact of urologic resident training on patient pain and morbidity associated with office-based cystoscopy. Urology. 2008; 71:782–786.
15. Ho KJ, Thompson TJ, O'Brien A, Young MR, McCleane G. Lignocaine gel: does it cause urethral pain rather than prevent it? Eur Urol. 2003; 43:194–196.
16. Carrion A, García-Cruz E, Fernandez C, D'Anna M, Melnick A, Peri L, et al. Prior lubrication of the urethra does not reduce pain perception in men undergoing flexible cystoscopy. Urol Int. 2016; 97:392–396.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download