This article has been
cited by other articles in ScienceCentral.
Abstract
Given that both orchidopexy and circumcision are commonly done in a single operative setting, we adopted a technique of combined orchidopexy and circumcision using a single circumcision incision. We applied this new technique to boys with palpable, low inguinal cryptorchidism. Here we describe a case series of 7 boys who underwent concurrent orchidopexy via the circumcision site. We present this novel technique and discuss our preliminary outcomes, including the anatomic basis and feasibility. The technique appears to be an alternative for concurrent circumcision and cryptorchid cases with palpable, low inguinal testes.
Go to :

Keywords: Case reports, Cryptorchidism, Male circumcision, Orchidopexy, Reconstructive surgical procedures
INTRODUCTION
Cryptorchidism is one of the most common congenital urogenital anomalies diagnosed at birth in boys [
1]. According to the latest guidelines published by the Pediatric Section of the European Association of Urology, both inguinal and scrotal orchidopexy are accepted standard treatment options for cryptorchidism [
2].
Infant circumcision has been shown to reduce the incidence of urinary tract infections in infant males during the first year of life. It also eliminates the need for a potentially medically indicated circumcision later in childhood for the treatment of phimosis, paraphimosis, or recurrent balanoposthitis [
3]. Furthermore, recent literature reports circumcision to be protective against the acquisition of various sexually transmitted infections in adult males [
3]. In the local setting, due to religious and cultural reasons, a circumcision is commonly requested to be done by parents for boys who will require a general anesthesia for another surgical procedure.
Given the above, circumcision and orchidopexy procedures are both commonly done in a single surgical setting. We adopted a technique of orchidopexy using a circumcision incision for palpable, low inguinal undescended testes. We herein present our retrospective case series on all patients who underwent concurrent circumcision and orchidopexy by a single surgeon in a tertiary specialized institution.
Go to :

MATERIALS AND METHODS
We retrospectively reviewed a series of patients who consecutively underwent a concomitant orchidopexy and circumcision via a single incision from September 2013 to December 2014 in Institute of Urology, St. Luke's Medical Center, Philippines. The study protocol was reviewed and approved by the Institutional Ethics Review Board (approval number: SLMC-2014 [SLIU] SL-IERC CT-14059). Patient confidentiality was ensured. The protocol was registered in Clinicaltrials.gov (NCT Identifier: NCT02249637).
The novel technique was performed by a single surgeon (MEC) at a tertiary care institution with standard preoperative evaluation, preparation, and postoperative care. Consent for the operations was obtained from the parents prior to the surgery, in which the parents confirmed understanding of the possible complications associated with the new procedure. Perioperative outcomes were reviewed, including operative time and 48-hour postoperative pain score (assessed with the pediatric visual analogue scale), and the parent's satisfaction was measured at 3 months after the procedure by use of an ordinal scale with 1 indicating unsatisfied and 5 indicating very satisfactory. Postoperative complications were likewise assessed at 1 week, 3 months, and 1 year after the surgical procedure.
1. Description of the surgical technique
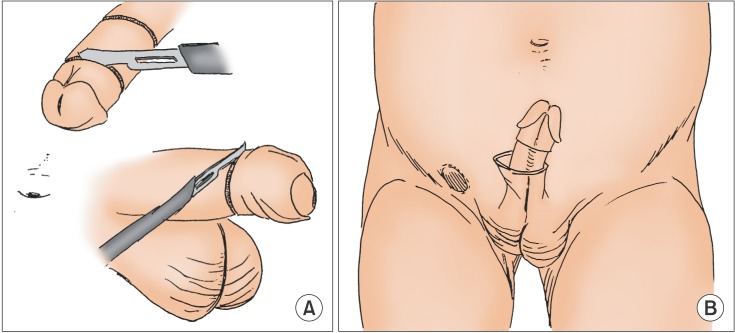
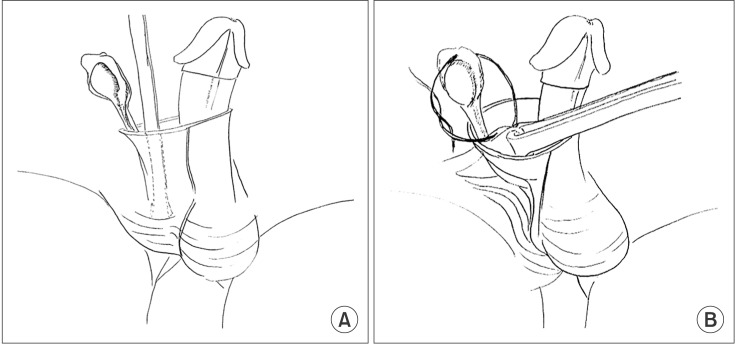
We performed the circumcision by using a sleeve-like technique; however, the mucosa was spared (
Fig. 1A). Partial degloving of the penis was done on the side of the undescended testis. With use of a mosquito clamp, the dissection was taken in the avascular plane of Dartos tissue down to the base of the penis, where the tissue layer allows dissection into the inguinal area (
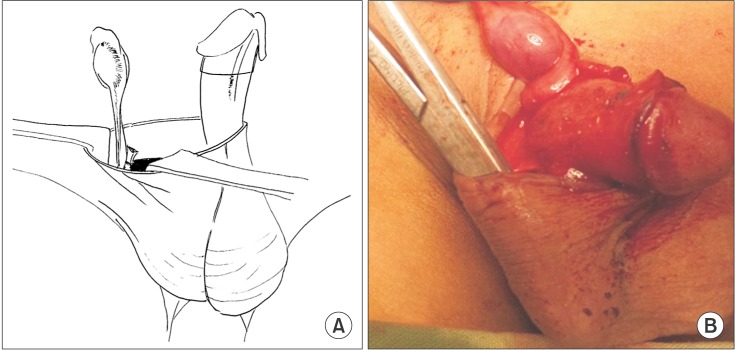
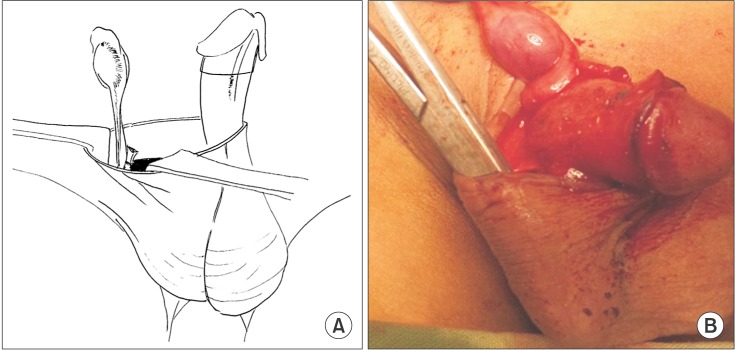
Fig. 1B). While being careful not to skive into the skin, small retractors were gently placed into the peno-inguinal space superficial to the pelvic bone, where the palpable testicle was easily identified and taken down distally (
Fig. 2A). A mosquito clamp was used to grasp the gubernaculum and mobilize the testicle from the surrounding cremasteric muscle fibers (
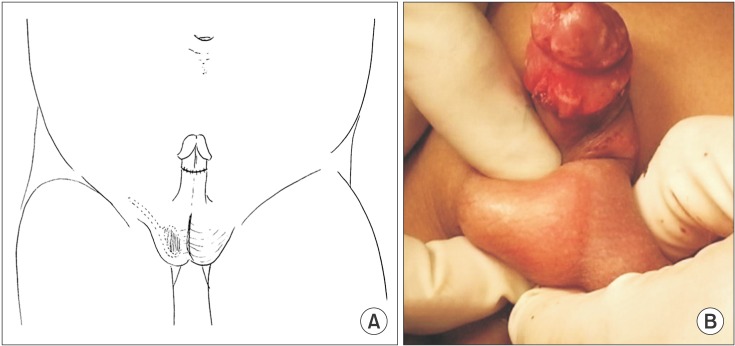
Fig. 2B). After the cord was dissected beyond the external ring, the hernial sac was separated from the cord, transected, and suture ligated as proximally as possible (
Fig. 3A). A Dartos pouch via the circumcision site was made by using a mosquito clamp (
Fig. 3B), and the inner surface of the developed pouch was grasped and everted by using an Allis clamp (
Fig. 4A). Testicular fixation was performed by using a Polyglactin 3-0 simple interrupted or figure 8 suture to the inner surface of the everted Dartos pouch (
Fig. 4B). The testicle was then placed in the correct anatomical position in the Dartos pouch and the scrotum was inverted (
Fig. 5A). Lastly, the procedure was completed with circumferential reapproximation of the mucosal collar to the penile shaft skin by use of Chromic 4-0 interrupted sutures (
Fig. 5B).
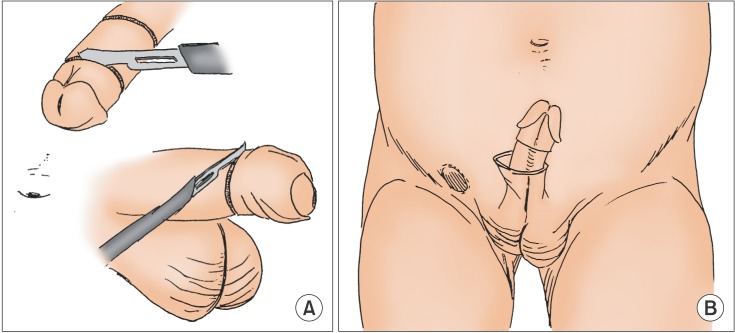 | Fig. 1(A) Double-incision circumcision mucosal-sparing approach. (B) Partial degloving of the penis on the side of the undescended testis. Dissection was made via the plane of the Dartos layer down to the penile base.
|
 | Fig. 2(A) Small retractors were gently placed into the peno-inguinal space. (B) The palpable testicle was extracted distally and the gubernaculum was grabbed with the mosquito clamp.
|
 | Fig. 3(A) After lengthening of the spermatic cord, the hernia sac was separated from the cord, transected, and suture ligated as proximally as possible. (B) The Dartos pouch was made via the circumcision site by use of a mosquito clamp.
|
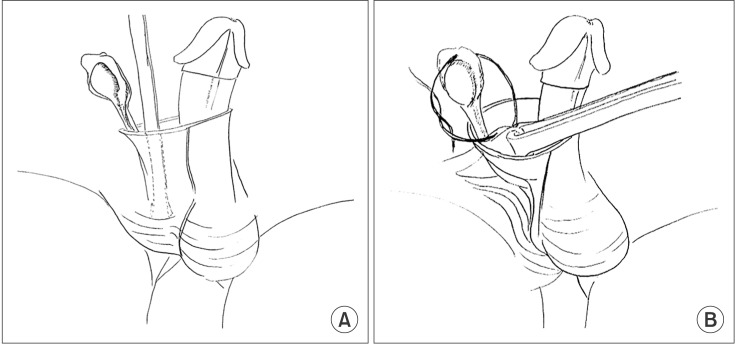 | Fig. 4(A) The inner surface of the developed Dartos pouch was grasped by using an Allis clamp. (B) Testicular fixation was done with a figure 8 suture to the inner surface of the everted Dartos pouch.
|
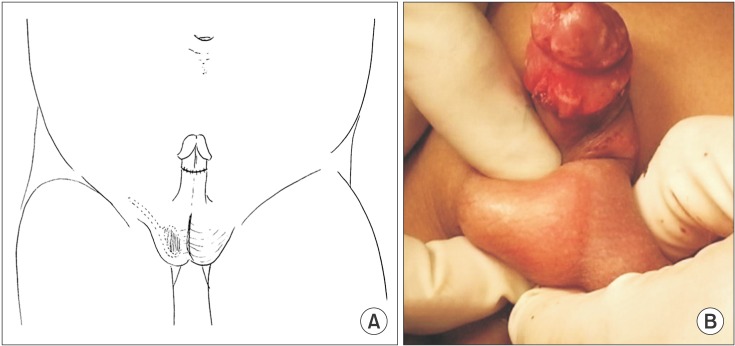 | Fig. 5(A) The testicle was placed into the Dartos pouch as the inner surface of the scrotum was inverted. (B) Completion of the circumcision closure by use of Chromic 4-0 interrupted sutures.
|
All patients were advised to return for follow-up after 1 week for a wound check, and then at 1 month and 3 months for a postoperative physical examination (
Fig. 6). A yearly follow-up visit was done to evaluate for testicular reascent or hernia occurrence.
 | Fig. 6Follow-up condition at 1 to 3 months.
|
Go to :

RESULTS
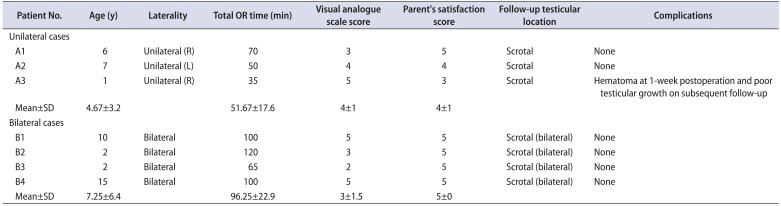
A total of seven boys aged 1 to 15 years underwent the novel circumcision-incision orchidopexy. All patients included had indications for circumcision and palpable, low, inguinal undescended testes diagnosed in the clinic. Four of the cases presented with bilateral cryptorchidism (
Table 1). No hormonal therapy was given pre- or postoperatively. None of the patients were diagnosed with retractile testes. Likewise, there were no previous scrotal or inguinal surgeries. All patients received a pain regimen of acetaminophen and ibuprofen as needed until postoperative day 3; no additional narcotic pain medications were needed. All patients had a 1-week follow-up in the outpatient clinic for evaluation of the wound; no wound infections were noted. One patient developed a self-limiting hematoma that was managed conservatively. Another postoperative evaluation was done at 1 month, 3 months, and 1 year; all testicles were positioned scrotally with no occurrence of hernias. The same patient with the postoperative hematoma was noted to have poor testicular growth on subsequent follow-up.
Table 1
Patient data and perioperative outcomes
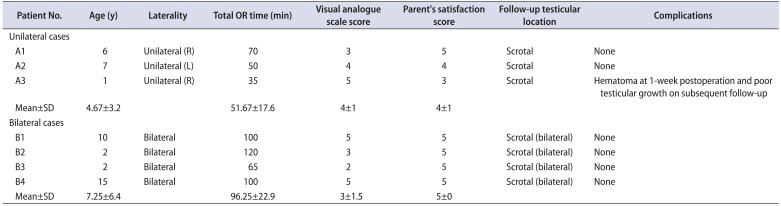
|
Patient No. |
Age (y) |
Laterality |
Total OR time (min) |
Visual analogue scale score |
Parent's satisfaction score |
Follow-up testicular location |
Complications |
|
Unilateral cases |
|
|
|
|
|
|
|
|
A1 |
6 |
Unilateral (R) |
70 |
3 |
5 |
Scrotal |
None |
|
A2 |
7 |
Unilateral (L) |
50 |
4 |
4 |
Scrotal |
None |
|
A3 |
1 |
Unilateral (R) |
35 |
5 |
3 |
Scrotal |
Hematoma at 1-week postoperation and poor testicular growth on subsequent follow-up |
|
Mean±SD |
4.67±3.2 |
|
51.67±17.6 |
4±1 |
4±1 |
|
|
|
Bilateral cases |
|
|
|
|
|
|
|
|
B1 |
10 |
Bilateral |
100 |
5 |
5 |
Scrotal (bilateral) |
None |
|
B2 |
2 |
Bilateral |
120 |
3 |
5 |
Scrotal (bilateral) |
None |
|
B3 |
2 |
Bilateral |
65 |
2 |
5 |
Scrotal (bilateral) |
None |
|
B4 |
15 |
Bilateral |
100 |
5 |
5 |
Scrotal (bilateral) |
None |
|
Mean±SD |
7.25±6.4 |
|
96.25±22.9 |
3±1.5 |
5±0 |
|
|

Go to :

DISCUSSION
In our local setting, the inguinal approach is still the primary mode of surgical treatment of cryptorchidism. A second incision on the scrotum for Dartos pouch development and testicular placement are common practice. A single-incision transscrotal technique was first introduced by Bianchi and Squire in 1989 [
4]. The considerable benefits of the Bianchi technique include a shorter operative time, less pain, and a cosmetically pleasing result with few complications [
5]. This approach is not well adopted in our local setting owing to inexperience and the presumed difficulty of dissection and identification of the undescended testis [
6].
As most patients who undergo orchidopexy for cryptorchidism also request circumcision in the same setting, we introduced a new technique using the circumcision incision site for the orchidopexy. We believe this technique may provide benefits similar to the Bianchi technique; anecdotally, it has shorter operative times, less pain, and a cosmetically pleasing result. The rationale for this technique is based on the anatomical contiguity of the penile Dartos layer with the inguinal Scarpa fascia of the abdomen and the scrotal space. The dissection of penile degloving on the side of the undescended testicle provides access to both spaces. The palpable undescended testicle can be easily located, mobilized, and fixed to its intended location in the scrotum. This novel technique also avoids potential trauma to the testis during transit through the inguinal canal as has been described by several authors with the conventional double-incision technique [
7].
Concerns regarding this approach may arise from its potential complications, such as testicular atrophy or ascent, hernia occurrence from persistence of the patent processus vaginalis, and possibility of cord trauma near the pelvic rim. These same concerns also arose when the Bianchi technique was first introduced. However, recent evidence from long-term follow-up data on Bianchi orchidopexy have shown that the rate of relapse is small (1.43%), as is the rate of testicular atrophy/hypotrophy (0.3%) and persistent/recurrent hernia (0.1%) [
5]. Novaes at al. [
5] have even proposed that in cases of undescended testicles in the low inguinal location, scrotal orchidopexy is the procedure of choice given its relatively low incidence of complications. Our results showed a similar complication rate, as hematoma can occur in any orchidopexy approach. The double-incision circumcision was previously described by Hittelman [
8] including partial penile degloving with mucosal preservation. We adapted the same principle, giving more attention to the laterality of the undescended testicle. Hence, the risk of general skin necrosis and neurovascular injury on the dorsal aspect may be prevented. Postoperative skin edema and ecchymosis are self-limiting conditions common with both conventional circumcision and the new technique
According to an anatomical study by Parnis et al. [
9] on the inguinal space in children, the inguinal segment of the processus vaginalis is short with a reported median length of 1 cm in children under 2 years of age and 1.1 cm in children over 4 years. Thus, owing to the pliable skin in children and additional traction of the spermatic cord distally, our technique can reasonably ligate the hernia sac at the same level of the internal inguinal ring as the inguinal orchidopexy. One advantage of our technique over scrotal orchidopexy is that the circumcision incision is closer to the internal ring and provides better exposure. In our series, there was no persistence or occurrence of any hernias.
In this preliminary series, we were able to report initial data on a novel technique of circumcision-incision orchidopexy with three follow-up exams. Given that complications with the novel technique were comparable to those with established operations and conversion to the conventional technique is always an option, we propose a new primary approach for the undescended testicle in a low inguinal position.
A limitation of the study was that the patients included were relatively older than the recommended age for orchidopexy. At this point, the outcome of circumcision-incision orchidopexy for children younger than 1 year cannot be extrapolated from the results of this study. Another limitation of this report was the small sample size. We are currently accumulating more cases with a younger patient population and longer surgical outcome follow-up for future publication. We also recommend a future larger scale and a prospective randomized study to be performed to further investigate the applicability of this novel procedure compared to the Bianchi and conventional inguinal approach.
Go to :

CONCLUSIONS
In our preliminary series, there were no major complications related to the novel circumcision-incision orchidopexy technique. This new procedure appears feasible as an alternative for concurrent circumcision and palpable cryptorchidism.
Go to :

ACKNOWLEDGMENTS
The author group would like to acknowledge the substantial help of Dr. Jessica Megan C. Ming on the English revision of the manuscript.
Go to :

Notes
Go to :

References
1. Virtanen HE, Bjerknes R, Cortes D, Jørgensen N, Rajpert-De Meyts E, et al. Cryptorchidism: classification, prevalence and long-term consequences. Acta Paediatr. 2007; 96:611–616. PMID:
17462053.

2. Radmayr C, Dogan HS, Hoebeke P, Kocvara R, Nijman R, Stein R, et al. Management of undescended testes: European Association of Urology/European Society for Paediatric Urology Guidelines. J Pediatr Urol. 2016; 12:335–343. PMID:
27687532.

3. Sorokan ST, Finlay JC, Jefferies AL. Canadian Paediatric Society. Fetus and Newborn Committee. Infectious Diseases and Immunization Committee. Newborn male circumcision. Paediatr Child Health. 2015; 20:311–320. PMID:
26435672.

4. Bianchi A, Squire BR. Trans-scrotal orchiopexy: orchiopexy revised. Pediatr Surg Int. 1989; 4:189–192.
5. Novaes HF, Carneiro Neto JA, Macedo A Jr, Barroso Júnior U. Single scrotal incision orchiopexy - a systematic review. Int Braz J Urol. 2013; 39:305–311. PMID:
23849581.

6. Al-Mandil M, Khoury AE, El-Hout Y, Kogon M, Dave S, Farhat WA. Potential complications with the prescrotal approach for the palpable undescended testis? A comparison of single prescrotal incision to the traditional inguinal approach. J Urol. 2008; 180:686–689. PMID:
18554646.

7. Evans J, Cosgrove C, Huddart S, Lambert A. The unidirectional testicular tunneller: a simple, safe and novel device for orchidopexy in patients with palpable undescended testes. Pediatr Surg Int. 2012; 28:693–696. PMID:
22581126.

8. Hittelman A. Double technique circumcision. In : Hinman FJ, Baskin LS, editors. Hinman's atlas of pediatric urologic surgery. 2nd ed. Philadelphia: W.B. Saunders Co.;2009. p. 776–783.
9. Parnis SJ, Roberts JP, Hutson JM. Anatomical landmarks of the inguinal canal in prepubescent children. Aust N Z J Surg. 1997; 67:335–337. PMID:
9193267.

Go to :

The standard approach for a palpable undescended testis has long been an inguinal orchidopexy because double incisions allow for adequate mobilization of the spermatic cord, easy dissection of a patent processus vaginalis, and the creation of subdartos pouch. In 1989, high scrotal (single) incision orchidopexy was introduced by Bianchi and Squire [
1] as a potentially less invasive technique. Since then, many pediatric surgeons have reported good results with a low rate of intraoperative conversion to the inguinal approach [
2].
This preliminary study of circumcision incision orchidopexy is also interesting as showing an idea of “killing two birds with one stone,” although the number of cases is small and the age of the patients is relatively older than the recommended age for orchidopexy.
My only concern, however, is that fewer incisions are not always better in terms of surgical completeness and safety. I hope further studies can eliminate my concern in the near future.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download