Abstract
Purpose
To report our outcomes with the use of a thermo-expandable metallic intraprostatic stent (Memokath) for patients with bladder outlet obstruction (BOO) secondary to prostatic obstruction, and to assess it is a feasible option for many frail and elderly men unsuitable for surgery.
Materials and Methods
We reviewed patients who underwent insertion of a Memokath stent for BOO over 17 years (January 1999 to December 2015) at one regional center over a long follow-up period (median, 7 years). Patients were selected if they had obstructive urinary symptoms or urinary retention with an indwelling catheter in situ, and were ineligible for transurethral resection of the prostate (TURP) under general or spinal anesthesia. Primary outcomes assessed were the improvement in urinary symptoms and voiding parameters, as well as the ability to void spontaneously if catheterized, along with complications.
Results
One hundred forty-four patients who presented with BOO or urinary retention had a Memokath stent inserted. Ninety patients (62.5%) had a successful stent insertion with a significant difference between the median preoperative (550 mL) and postoperative residual volume (80 mL, p<0.0001). Nearly two-thirds of men (64%) returned to unassisted voiding with no increased risk of complications over time. Fifty-four patients (37.5%) experienced stent failure. Main complications requiring stent removal or repositioning were migration, occlusion, refractory urinary retention and irritative voiding symptoms.
Bladder outlet obstruction (BOO) secondary to benign prostatic hyperplasia (BPH) or prostate cancer (PCa) is a common cause of bothersome lower urinary tract symptoms (LUTS). The incidence of clinical and histological BPH increases with age, affecting 50% of men at 60 years of age and 90% by 80 years [1]. Advancing age increases the incidence of BPH, as well as medical comorbidities that may prevent a man from undergoing surgical treatment [2]. Even though the use of medical therapy for LUTS has decreased the rates of surgery for BPH, this has lead to patients presenting at an older age for surgery [3], with the risk of surgery related to BPH considerably greater for men aged 80 years and over [4]. Frail health and comorbidities such as cardiovascular or respiratory disease, stroke, diabetes and chronic kidney disease may increase a patient's risk by up to 11% for a major cardiac event during surgery [5]. Endoscopic treatment such as transurethral resection of the prostate (TURP), together with the use of anticoagulants, put this vulnerable group of patients at an increased risk of both early and late complications [6].
In men who are deemed medically unfit to undergo TURP, enucleation or ablation via general or spinal anesthesia, there are few therapeutic options are left. In those with urinary retention, long-term suprapubic or urethral indwelling catheters (IDCs) are often employed if unable to perform intermittent self-catheterization. There are however significant bio-psychosocial impacts of such treatment. These include recurrent urinary tract infections, catheter blockage, need for frequent replacement, trauma to the urinary tract, meatal erosion, psychological distress, and negative impact on sexual function [789]. For men who desire an alternative option to long-term catheterization or troublesome BOO, and are precluded from surgery due to medical comorbidities, a thermo-expandable metallic intraprostatic stent (Memokath, Pnn Medical, Kvistgaard, Denmark) may be a practical and underutilized alternative.
Stents have been used in various settings in the urinary tract for nearly four decades (for strictures of ureter, urethra, as an alternative to sphincterotomy and for BOO) [910]. Prostatic stents have been utilized since 1980, and have evolved over time with improvements in the composite materials, the degree of urothelial reaction generated along with their shape, plasticity and method of insertion. This has helped minimize complications such as difficult removals under local anesthesia, urethral injury, encrustation and migration [9]. The Memokath 028 (Pnn Medical) stent is a third generation nonepithelializing (inert) thermo-expandable (24 to 42F) stent that is made of a memory alloy of nickel and titanium [1112]. The Memokath stent has been previously shown to reduce International Prostate Symptoms Score by 13 points, increase peak flow (Qmax) by 7 mL/s and reduce mean postvoid residual (PVR) by 126 mL [10]. The aim of our study is to report the outcomes of using the Memokath stent over a long follow-up period, and to assess whether it is a feasible option for many frail and elderly men unsuitable for surgery.
Ballarat Health Ethics committee approval number HREC/15/BHSSJOG/68. Written informed consent was waived by the ethics committee. We reviewed all patients who underwent insertion of a Memokath stent for BOO over 17 years (January 1999 to December 2015) across 2 hospitals at 1 regional center. We defined BOO as obstructive LUTS or urinary retention due to BPH or PCa. Patients did not routinely undergo urodynamic studies prior to Memokath insertion and an assessment was made by the clinician on the likely underlying detrusor function based on voiding pattern, sensation and PVR. Patients were included in the study if they had BOO or urinary retention with an IDC in situ, and were ineligible for TURP under general or spinal anesthesia based on a clinical decision (by surgeon or anesthesiologist) in consultation with the patient. Data collection was performed in accordance with the principles of the Helsinki Declaration.
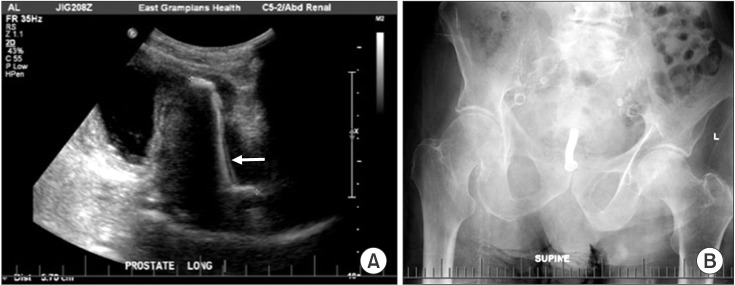
The technique for Memokath insertion was reproduced on each occasion. Patients were given a single dose of intravenous antibiotics (either aminoglycoside or cephalosporin) and placed in the supine position. A flexible cystoscopy (16F) was performed in order to measure the distance between the bladder neck and verumontanum using measuring calipers. This measurement was taken 3 times to obtain a median length for selecting the most appropriate prostatic stent length. The Memokath stent system was then loaded over the flexible cystoscope and deployed at the bladder neck whilst injecting warmed saline at 57 degrees Celsius [10]. This expanded the stent from a diameter of 24 to 42F. The patient then underwent observation or trial of void and a postoperative ultrasound was obtained to check position within the prostatic urethra (Fig. 1).
Patients were clinically reviewed on an annual basis along with an ultrasound to monitor stent position. Primary outcomes assessed post Memokath insertion were the improvement in symptoms and PVR measurements, the ability to void spontaneously if catheterized, and complications. Stent failure was defined as removal, replacement or repositioning of the Memokath. These adjustments were all performed under local anesthesia +/− sedation. Complications that lead to stent failure were recorded as acute urinary retention, migration, occlusion from stones or encrustation, recurrence of obstructive LUTS/BOO, irritative LUTS and de novo urge incontinence. The outcomes before and after stent insertion were compared by paired t-test (InStat, GraphPad Software Inc., La Jolla, CA, USA), subgroup analyses by Student t-test and stent failure and complications were compared to published data.
One hundred forty-four men underwent insertion of a Memokath stent over a period of 17 years. The demographical and clinical information of this cohort is summarized in Tables 1 and 2. The median age was 80 years (range, 34 to 96 years). One hundred thirty-four (93%) patients had clinical BPH and 10 (7%) had known PCa as a cause of BOO. Patients were followed up for a median period of 84 months (7 years; range, 4 to 197 months). The median prostatic volume was 75 mL and median stent size utilized was 4 cm (range, 3 to 9 cm). Of the 144 patients who presented with BOO, 62 (43%) presented with LUTS, and 82 (57%) had urinary retention. Ninety patients (62.5%) had a successful stent insertion, and 65 out of 82 patients in urinary retention (79.2%) had a return of unassisted voiding (odd ratio, 1.75; 95% confidence interval, 1.17–2.63; p=0.007). There was a significant difference between the mean preoperative PVR measured (571 mL) and the mean postoperative PVR (100 mL, p<0.0001).
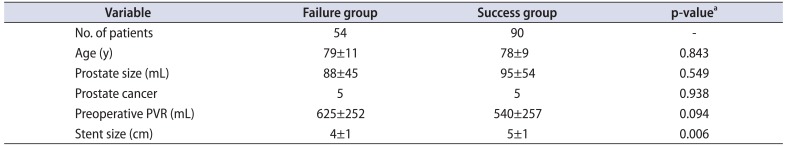
The overall failure and complication rates are shown in Table 3. Fifty-four patients (37.5%) experienced stent failure. The median time to stent failure was 6 months (interquartile range, 1–13 months). Amongst this group of patients, 17 (11.8%) had acute urinary retention immediately post insertion; 9 (6.25%) had early or late migration on ultrasound; 23 (16%) had recurrence of BOO; 11 (7.6%) had stent occlusion due to stones or encrustation; 2 patients had irritative LUTS; 1 patient had urge incontinence and another had recurrent urinary infection. As a result of these complications, 42 Memokath stents (36%) were removed without attempting repositioning, 10 (6.95%) were removed after failed repositioning and 2 were repositioned successfully. Removal occurred mostly by flexible cystoscopy under local anesthesia, with the addition of sedation as required. Three patients required simple stent removal with a 20F rigid cystoscope under general anesthesia, and a further two patients underwent a general anesthesia for stent related bladder calculi requiring cystolitholapaxy. There was no difference in stent failure rates based on prostatic size (p=0.55) but there was correlation to stent size (p=0.006) with larger stents less likely to fail. An analysis of potential predictors on outcome based on age, prostate and stent size is shown in Table 4.
Long-term IDC may impose significant limitations on a man's quality of life due to considerable associated morbidity. Twenty-eight percent (28%) of men experience catheter blockages, 37% experience bypassing requiring continence pads, 30% experience hematuria, and 18% experience recurrent urinary tract infection [7]. Recurrent infection poses a significant issue due to the emergence of bacterial resistance to available antibiotics [8].
This study is the longest known follow-up for efficacy, safety and durability of thermo-expandable prostatic Memokath stents. Whilst there is evidence that the clinical outcomes of Memokath stent insertion are comparable to TURP [9], it is important to state that comparison of the Memokath stent should be made against long-term catheterization and not surgical therapy, which remains the definitive treatment of BPH. The focus of the stent is on return to unassisted voiding, improvement in quality of life, cost benefit, durability and improved sexual function compared with catheterization.
Our series demonstrates Memokath to be a safe, and cost-effective intervention for men with BOO. The overall complication rate of 37.5% is comparable to other publishes series (20%–48%) as is the removal rate of 36% [9101112131415]. Stent migration has been cited as a reason for prostatic stents being an unfavorable option for patients with BOO [1617].
Our rate of stent migration was low at 6.25% compared to other series (13%–19%) [9101112131415]. This may be due to the repeated measurement of prostatic length on insertion enabling accuracy in stent lengths used. In our experience, larger prostates may hold the stents in a better position and limit migration, and this was partially proven this analysis by stent size rather than prostate size. We found no difference in subgroup analyses when comparing operative difficulty or outcomes between the BPH and PCa groups.
The Memokath encrustation rate compares favorably to frequency of reported catheter blockages (7.6% vs. 28%) and the rate of recurrent infection is significantly less than an IDC (0.69% vs. 18%) [7]. Complications requiring removal were done with ease as an outpatient procedure under flexible cystoscopy and cold irrigation with minimal discomfort.
The median patient survival in our series was 6 years, and 57 patients (39.5%) died during their follow-up course from events unrelated to Memokath placement. This is consistent with other reports in that the majority of men died with their stents rather than outlive the usefulness of the stent itself [14]. This is an important point when comparing against men with long-term IDC who may require numerous catheter changes in their remaining years and the prospect of catheter related mortality of 2.3% [18].
Long-term catheterization can also incur a significant financial cost. The average health care cost for a patient with an IDC is over AUD $2,500 per year in Australia [1920] when taking into account supplies and medical treatment for complications, compared to the current AUD $3,800 cost of the Memokath. The costs of stent against catheterization in this patient cohort would be comparable within a short duration, not taking into account complications associated with stent placement. This cost needs to be weighed against the median survival of a patient with a prostatic stent, and is likely to deliver a substantial saving per patient.
Whilst there at least 20 other types of prostatic stents are available [12], our study did not compare the efficacy other stents. Our center is well experienced with Memokath use and this is appearing to be the trend in Australia and Europe [913]. Other stents, such as the Urolume have not fared better than the Memokath stent with epithelialization posing challenges with removal [9].
The reasons that intraprostatic stents may be an underutilized treatment option for frail and elderly men are likely multifactorial. There may be limited training and exposure to intraprostatic stent devices, but with a knowledge of the cost benefit and short learning curve in application, can be widely employed [21]. The landscape of LUTS has changed dramatically during the lifetime of the prostatic stent with the improvement in the efficacy and reduction in the side effects of medical therapy. Improvements in anesthesia over the years plus the emergence of laser ablation, has resulted in various minimally invasive surgical techniques carrying less morbidity than the standard electrocautery of TURP, with the benefit of performing surgery on anticoagulated patients [22].
A more recent technique of prostatic urethral lift has proved successful in an ambulatory day case setting under topical or regional anesthesia [2324].
Its use is becoming widespread but requires a longer learning curve and still necessitates the use of rigid cystoscopy.
There are some limitations of this study. Data was recorded retrospectively and other than patient response and PVR, no other objective data was recorded. Improvement was largely measured by patient reporting. Patients with a diagnosis of BOO from PCa were also included in this study together with those with BPH and, whilst it is unlikely that this distorted the outcomes, this mild heterogeneity in etiology may present a confounding factor in analyzing outcomes. The rate of men with PCa may have been underestimated as the majority of patients had a clinical, not histological diagnosis of BPH. Given that all patients were not suitable to proceed to TURP to obtain a formal diagnosis of PCa, men with PCa were included into the study as it reflected the case-mix of clinical practice. Fitness for surgery was assessed by specialist opinion only (surgical or anesthetic) and no performance status scales were used.
In elderly and frail men with BOO, who are not suitable to undergo TURP and have preserved detrusor function, the thermo-expandable metallic intraprostatic stent (Memokath) is a safe, cost-effective, potentially underutilized and practical alternative to long-term catheterization. This is supported by an excellent result of the majority of men returning to unassisted voiding who are otherwise left with the long-term morbidity of an IDC. In this study with long patient follow-up, the use of Memokath stent demonstrated no increase in complications over time, and a significant number of men outlive the functional duration of the stent.
References
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PMID: 6206240.

2. Choi SY, Kim TH, Myung SC, Moon YT, Kim KD, Kim YS, et al. Impact of changing trends in medical therapy on surgery for benign prostatic hyperplasia over two decades. Korean J Urol. 2012; 53:23–28. PMID: 22323970.

3. Vela-Navarrete R, Gonzalez-Enguita C, Garcia-Cardoso JV, Manzarbeitia F, Sarasa-Corral JL, Granizo JJ. The impact of medical therapy on surgery for benign prostatic hyperplasia: a study comparing changes in a decade (1992-2002). BJU Int. 2005; 96:1045–1048. PMID: 16225526.

4. Glynn RJ, Campion EW, Bouchard GR, Silbert JE. The development of benign prostatic hyperplasia among volunteers in the Normative Aging Study. Am J Epidemiol. 1985; 121:78–90. PMID: 3964994.
5. Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999; 100:1043–1049. PMID: 10477528.

6. Brierly RD, Mostafid AH, Kontothanassis D, Thomas PJ, Fletcher MS, Harrison NW. Is transurethral resection of the prostate safe and effective in the over 80-year-old? Ann R Coll Surg Engl. 2001; 83:50–53. PMID: 11212452.
7. Kohler-Ockmore J, Feneley RC. Long-term catheterization of the bladder: prevalence and morbidity. Br J Urol. 1996; 77:347–351. PMID: 8814836.
8. National Clinical Guideline Centre (UK). Chapter 10, Long term urinary catheters. Infection: prevention and control of healthcare-associated infections in primary and community care: partial update of NICE clinical guideline 2. NICE Clinical Guidelines, No. 139. London: Royal College of Physicians (UK);2012.
9. Armitage JN, Rashidian A, Cathcart PJ, Emberton M, van der Meulen JH. The thermo-expandable metallic stent for managing benign prostatic hyperplasia: a systematic review. BJU Int. 2006; 98:806–810. PMID: 16879446.

10. Papatsoris AG, Junaid I, Zachou A, Kachrilas S, Zaman F, Masood J, et al. New developments in the use of prostatic stents. Open Access J Urol. 2011; 3:63–68. PMID: 24198637.

11. Poulsen AL, Schou J, Ovesen H, Nordling J. Memokath: a second generation of intraprostatic spirals. Br J Urol. 1993; 72:331–334. PMID: 7693295.
12. Minagawa T, Murata Y, Seki S. Placement of a shape-memory alloy intraurethral catheter (Memokath) using transrectal ultrasonography and fluoroscopy. Nihon Hinyokika Gakkai Zasshi. 2009; 100:508–512. PMID: 19348192.

13. Kimata R, Nemoto K, Tomita Y, Takahashi R, Hamasaki T, Kondo Y. Efficacy of a thermoexpandable metallic prostate stent (Memokath) in elderly patients with urethral obstruction requiring long-term management with urethral Foley catheters. Geriatr Gerontol Int. 2015; 15:553–558. PMID: 24852087.

14. Perry MJ, Roodhouse AJ, Gidlow AB, Spicer TG, Ellis BW. Thermo-expandable intraprostatic stents in bladder outlet obstruction: an 8-year study. BJU Int. 2002; 90:216–223. PMID: 12133055.

15. Lee G, Marathe S, Sabbagh S, Crisp J. Thermo-expandable intra-prostatic stent in the treatment of acute urinary retention in elderly patients with significant co-morbidities. Int Urol Nephrol. 2005; 37:501–504. PMID: 16307329.

16. Na HK, Song HY, Kim JH, Nam DH, Park JH, Jeong IG, et al. Evaluation of the anti-migration effect of barbed prostatic stents: in vitro study in urethra-mimicking bovine pericardium phantoms. Cardiovasc Intervent Radiol. 2013; 36:229–236. PMID: 22829302.

17. Woo CW, Song HY, Yoon CJ, Kim TH, Kim EY, Kim JH, et al. Is a flared stent effective for decreasing stent migration in canine prostatic urethra? Acta Radiol. 2008; 49:285–290. PMID: 18365816.

18. Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA, Brennan J, et al. Guideline for prevention of catheter-associated urinary tract infections. Atlanta (GA): Centres for Disease Control and Prevention;2009.
19. Booth CM, Chaudry AA, Lyth DR. Alternative prostate treatments: stent or catheter for the frail. J Manag Care. 1997; 1:24–26.

20. Australian Institute of Health and Welfare 2012. Health expenditure Australia 2010-11. Health and welfare expenditure series No. 47. Cat. No. HWE 56. Canberra (Australia): Australian Institute of Health and Welfare;2012.
21. Rashid P, Gianduzzo TR. Urology technical and non-technical skills development: the emerging role of simulation. BJU Int. 2016; 117(Suppl 4):9–16.

22. Jumper C, Snyder P, Yap RL. Rapid ambulatory pathway laser prostatectomy is safe: results within the global period. BJU Int. 2012; 110:1190–1193. PMID: 22372831.

23. Roehrborn CG, Gange SN, Shore ND, Giddens JL, Bolton DM, Cowan BE, et al. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L.I.F.T. Study. J Urol. 2013; 190:2161–2167. PMID: 23764081.
Table 1
Summary of patient demographic and presentation and results of patients undergoing insertion of thermo-expandable intraprostatic (Memokath) stent
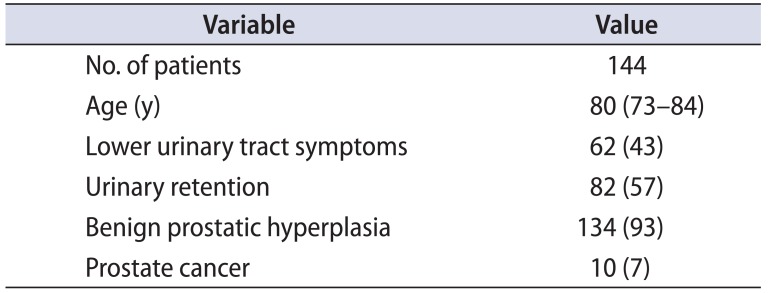
| Variable | Value |
|---|---|
| No. of patients | 144 |
| Age (y) | 80 (73–84) |
| Lower urinary tract symptoms | 62 (43) |
| Urinary retention | 82 (57) |
| Benign prostatic hyperplasia | 134 (93) |
| Prostate cancer | 10 (7) |
Table 2
Summary of patient outcomes and follow-up of patients undergoing insertion of thermo-expandable intraprostatic (Memokath) stent
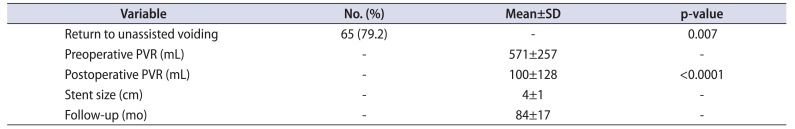
Table 3
Overall failure and complication rate of patients undergoing insertion of the thermo-expandable intraprostatic (Memokath) stent (n=144)
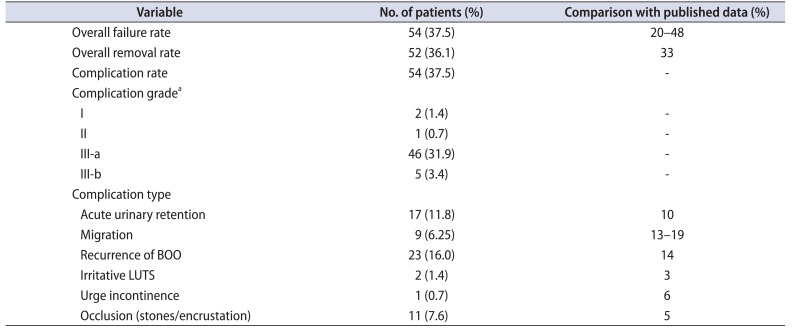
BOO, bladder outlet obstruction; LUTS, lower urinary tract symptoms.
a:Clavien-Dindo classification: grade I, any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions; grade II, requiring pharmacological treatment including blood transfusions and total parenteral nutrition; grade III-a, requiring surgical, endoscopic or radiological intervention without general anesthesia; grade III-b, requiring surgical, endoscopic or radiological intervention with general anesthesia.
Table 4
Assessing potential predictors of stent failure in patients undergoing insertion of the thermo-expandable intraprostatic (Memokath) stent




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download