Abstract
Purpose
To analyze the long-term clinical outcomes of men with large prostate sizes of 80 mL and greater who were managed conservatively.
Materials and Methods
We retrospectively analyzed men with prostate sizes of 80 mL and greater from our electronic hospital database. Clinical parameters such as age, International Prostate Symptom Score (IPSS), quality of life (QoL) scoring, serum prostate-specific antigen (PSA), uroflowmetry variables, and transabdominal ultrasound findings were evaluated. These parameters were compared at entry to our study and at the patient's latest follow-up visit.
Results
For the 50 men included in our analysis, mean age was 68 years, median PSA was 9.9 ng/mL, and median prostate volume was 94 mL. Seven men underwent upfront prostate surgery, whereas the other 43 were managed conservatively, predominantly with pharmacotherapy (98%). Only serum PSA, QoL scores, and postvoid residual urine demonstrated a significant reduction at the end of a median follow-up period of 62 months. Fourteen men (33%) were considered to have progressed clinically, with 8 experiencing retention of urine and 6 having symptomatic deterioration. Of the 35 men who were still receiving conservative treatment at the end of the follow-up period, 24 men (69%) had a peak flow rate of 10 mL/s or greater, a QoL score of 3 or less, and mild to moderate (IPSS, 0–19) symptoms.
Benign prostatic hyperplasia (BPH) is a common cause of bladder outlet obstruction that occurs in men above the age of 50 [1]. In community-dwelling men from the Olmsted County (Minnesota) Study aged 40 to 79 years, overall mean prostate volume was about 28 mL [2]. With age, the prostate gland enlarges, most commonly due to BPH. However, not all men develop lower urinary tract symptoms (LUTS) or bladder outlet obstruction. Moreover, the severity of their LUTS tends to correlate poorly with the presence of bladder outlet obstruction [34].
Men with BPH can be managed with watchful waiting, pharmacotherapies such as alpha-blockers or 5-alpha reductase inhibitors, or prostate surgery. For very large prostate glands such as those larger than 80 mL, open prostatectomy and holmium laser enucleation of the prostate (HoLEP) are options for surgical management. A few randomized controlled trials have shown HoLEP to have outcomes similar to open surgery with a significantly lower complication rate [567]. There is, however, little information on the natural history of very large prostate glands that have been managed without surgical intervention.
To address this gap in the literature, we conducted a retrospective analysis of our BPH database of men with prostate sizes larger than 80 mL. The objective of our study was to assess the long-term clinical outcomes in these men, in particular those who were managed without surgical intervention.
A prospectively maintained electronic database for a single institution was reviewed for men diagnosed with BPH. As of July 2016, there were 1,367 men in our records. Clinical information was collected from both electronic and paper records when the men had prostate sizes that equaled or exceeded 80 mL (as their point of entry into our analysis) and also at their last follow-up visit (or last visit before any surgical intervention). Exclusion criteria were a diagnosis of prostate cancer at any one point of time or a history of prostate surgery prior to evaluation.
Clinical parameters such as age, comorbidities, International Prostate Symptom Score (IPSS), quality of life (QoL) score, serum prostate-specific antigen (PSA), uroflowmetry, and transabdominal ultrasound findings were evaluated. Other information such as the development of acute urinary retention, gross hematuria, urinary tract infection, bladder calculi, hydronephrosis, overflow incontinence, and obstructive uropathy was also analyzed. A bedside transabdominal ultrasound scan was mainly performed by a single operator (KTF) to measure prostate volume, intravesical prostatic protrusion (IPP), and postvoid residual urine for all patients. The method of measurement of IPP and grading was previously reported and has been shown to correlate well with transrectal measurement when bladder volume is less than 400 mL [8].
Clinical progression was defined as symptomatic deterioration of 4 or more points using IPSS, development of acute retention of urine, recurrent urinary tract infection (2 or more episodes in a year), bladder calculi, overflow incontinence, hydronephrosis, or obstructive uropathy. These parameters were then compared at entry to our study and at the patient's latest follow-up.
Taking the above parameters into consideration, these patients were staged and treated according to our system previously described [9]. All treatment options had to take into account the patients' age, preferences, and competing comorbidities. Hence, the actual treatment given may not have conformed entirely to our proposed system.
Most of our data are expressed as medians with respective interquartile ranges because our sample was small and without a normal distribution. Statistical analysis was performed by using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Any differences in medians between paired data were analyzed by using Wilcoxon's signed rank test. Differences were considered significant if p<0.05. This study was approved by Centralised Institutional Review Board, Singhealth, Singapore (DSRB reference number: 2012/311/D).
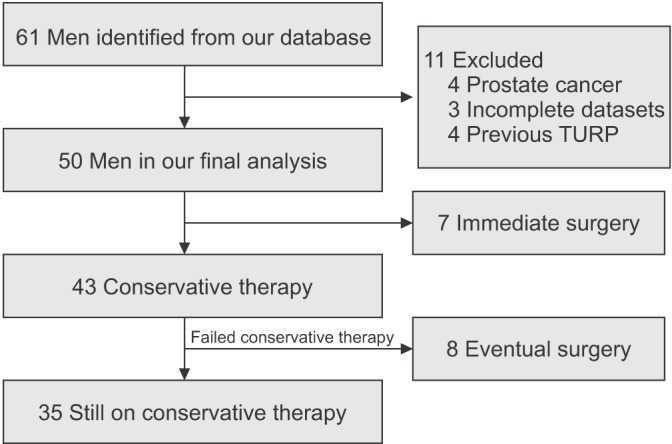
Of the 1,367 men in our database, only 61 (4.5%) had a prostate size of 80 mL or larger. However, 11 patients were excluded: 4 had prostate cancer, 4 had a history of previous prostate surgery, and 3 had missing data (Fig. 1). The baseline characteristics of the 50 men included in our final analysis are summarized in Table 1. The patients' mean age was 68 years, their median PSA was 9.9 ng/mL, their median prostate volume was 94 mL, and the median IPP was 15 mm. Most men presented with LUTS (46%), followed by raised PSA (24%) and acute urinary retention (14%). Based on uroflowmetric evaluation, the median peak flow rate (Qmax) was 11.4 mL/s with a median postvoid residual urine (PVRU) of 58 mL.
Seven men underwent upfront prostate surgery. Their indications were acute retention of urine (2 men), chronic retention of urine with persistently high PVRU (2 men), bladder stones (2 men), and bothersome LUTS (1 man). Of the remaining 43 men, 24 were treated with only 5-alpha reductase inhibitors, 2 with only alpha-blockers, 16 with both drugs, and 1 with watchful waiting.
The 43 patients on conservative therapy were followed up for a median of 62 months (interquartile range [IQR], 20–127 months; range, 3–221 months). When their clinical parameters were compared at entry and at the end of followup, only serum PSA, QoL scores, and PVRU demonstrated a significant reduction (Table 2). Prostate volume, total IPSS, and Qmax did not differ significantly at the end of the follow-up period. Thirty-three percent of the men had symptomatic improvement of 4 or more points, whereas 49% had stable symptom scores (within 3 points of the score at entry).
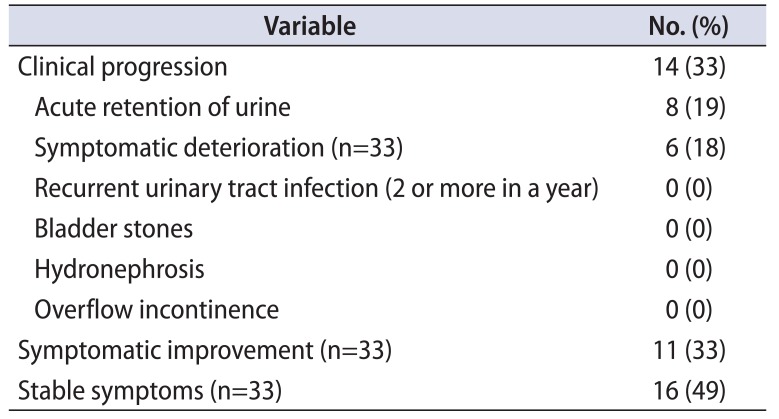
A total of 14 men (33%) on conservative management showed clinical progression (Table 3). Of those who progressed, 8 developed acute retention of urine, whereas 6 had symptomatic deterioration of 4 or more points. Six of the 14 with clinical progression opted for surgery. None developed recurrent urinary tract infection, bladder stones, gross hydronephrosis, renal impairment, or overflow incontinence. All who developed retention were either successfully trialed off the catheter or underwent surgical intervention. None were placed on clean intermittent self-catheterization or a long-term indwelling urinary catheter at the end of the follow-up period.
During follow-up, 8 men eventually underwent surgical management, of which 6 were for acute retention of urine. For the remaining 2 men, both had moderate LUTS that were bothersome and not responding to pharmacotherapy and one had a prior episode of acute retention of urine and had a successful trial of voiding. Median months to surgery was 30.5 months (IQR, 21–103 months). In both the univariate and the multivariate analyses, baseline age, prostate volume, PSA, IPSS, QoL, IPP, Qmax, and PVRU were not significant predictors of clinical progression.
Of the 35 men who were still on conservative treatment at the end of follow-up, 24 men (69%) had a Qmax 10 mL/s or more, QoL score of 3 or less, and only mild to moderate (IPSS, 0–19) symptoms.
A total of 15 patients underwent prostate surgery, of which 7 were performed soon after they presented and 8 were performed in those who had failed a period of conservative therapy. Eight patients underwent transurethral enucleation and resection of the prostate and the other seven underwent transurethral resection of the prostate. Median resection time was 165 minutes (IQR, 100–190 minutes), median resected prostate weight was 64 g (IQR, 55–78 g). Only one patient needed a single perioperative transfusion. Median hospitalization stay and postoperative catheter days were 3 days each. No other complications were reported (e.g., transurethral resection syndrome, prostatic capsular perforation). All patients were discharged without a urinary catheter after a successful trial of voiding.
Several population-based studies such as the Olmsted County Study have provided information on the natural history of BPH [10]. Prostate volume was noted to increase by a median of 1.9% per year and this growth appears to be related to baseline prostate volume [11]. In the same cohort of men, men with a baseline prostate volume of 30 mL or less had prostate growth of 1.7% per year compared to 2.2% per year in men with prostate volumes greater than 30 mL [11]. An analysis comprising data from 3 of the largest and longest multinational, placebo-controlled trials also demonstrated that a larger baseline prostate volume is associated with greater risk of acute retention of urine [12]. Further meta-analysis also suggests that a 5-alpha reductase inhibitor such as finasteride is most effective in men with larger prostates above 40 mL [13]. In men with prostate volumes above 80 mL, surgical options include open prostatectomy, HoLEP, and transurethral prostatectomy. However, there is a dearth of long-term clinical data regarding men with prostate volumes of 80 mL and above who have been managed conservatively.
To address this gap in the literature, we performed a retrospective review of men with prostate sizes of 80 mL and above to assess their long-term clinical outcomes and progression. Of the 43 men who were initially managed conservatively, all except 1 man were managed with pharmacotherapy, for which a 5-alpha reductase inhibitor was most commonly prescribed. Over a median follow-up of 62 months, prostate volume, Qmax, and total IPSS scores did not appear to change significantly. Thirty-three percent of the men showed clinical progression, for which 57% was due to acute retention of urine and the other 43% was due to the symptomatic deterioration of 4 or more points on the IPSS. Despite the relatively high rate of clinical progression, 33% of men showed improvement of 4 or more points on the IPSS whereas 49% had stable symptom scores. At the end of follow-up, median QoL scores also demonstrated a 1-point improvement (from “mixed” to “mostly satisfied”).
This study provides a unique perspective regarding clinical outcomes in men with prostate volumes of 80 mL or larger. Not surprisingly, the clinical progression rate in this group of men was high compared with other studies of men with smaller prostates. For example, Marberger et al. [12] performed a pooled analysis of men enrolled in the placebo arm of 3 large, multinational placebo-controlled trials which revealed that the 2-year incidence of spontaneous acute urinary retention was 1.6% in men with a prostate size less of than 40 mL in contrast to 4.2% in men with prostate sizes of 40 mL or more. Despite the high rate of progression, one cannot ignore the fact that a significant proportion (69%) of these men still have QoL scores of 3 and below, mild to moderate symptoms (IPSS, 0–19), and peak flow equal to or greater than 10 mL/s while being managed conservatively, predominantly with pharmacotherapy. Moreover, none suffered other complications of BPH such as recurrent urinary tract infections, bladder stones, or hydronephrosis with obstructive uropathy. This set of results serves as evidence to suggest that conservative management of men with large prostates may be a viable treatment option. In the authors' opinion, it allows clinicians to better counsel these men on the natural history of their conditions should they opt for nonsurgical treatments. In our study, the men were managed according to our staging system previously described [9] and our results suggest that this system can also be applied to this unique subset of men with very large prostates.
The main limitation of our study would be that of our small sample size. However, the subset of men with very large prostate sizes (80 mL and above) are the minority within our pool of patients diagnosed with BPH and even more so in the general population. To the authors' knowledge, this is a unique study specifically studying the outcomes of conservative management in this select group of men, in contrast to the readily available data on surgical outcomes involving HoLEP and simple prostatectomy for such large prostates. Perhaps, subanalyses of the larger, multi-institutional trials involving men with BPH could be performed to add further information to the current body of evidence, which appears to be inadequate.
References
1. Arrighi HM, Metter EJ, Guess HA, Fozzard JL. Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. Urology. 1991; 38(1 Suppl):4–8. PMID: 1714657.
2. Rhodes T, Girman CJ, Jacobsen SJ, Roberts RO, Guess HA, Lieber MM. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999; 161:1174–1179. PMID: 10081864.

3. Steele GS, Sullivan MP, Sleep DJ, Yalla SV. Combination of symptom score, flow rate and prostate volume for predicting bladder outflow obstruction in men with lower urinary tract symptoms. J Urol. 2000; 164:344–348. PMID: 10893581.

4. Yalla SV, Sullivan MP, Lecamwasam HS, DuBeau CE, Vickers MA, Cravalho EG. Correlation of American Urological Association symptom index with obstructive and nonobstructive prostatism. J Urol. 1995; 153(3 Pt 1):674–679. PMID: 7532231.

5. Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008; 53:160–166. PMID: 17869409.

6. Naspro R, Suardi N, Salonia A, Scattoni V, Guazzoni G, Colombo R, et al. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur Urol. 2006; 50:563–568. PMID: 16713070.
7. Zhang Y, Du CJ, Xu G, Chen JM, Jing X. Transurethral holmium laser enucleation for prostate adenoma greater than 100 g. Zhonghua Nan Ke Xue. 2007; 13:1091–1093. PMID: 18284057.
8. Yuen JS, Ngiap JT, Cheng CW, Foo KT. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol. 2002; 9:225–229. PMID: 12010318.

9. Wang D, Foo KT. Staging of benign prostate hyperplasia is helpful in patients with lower urinary tract symptoms suggestive of benign prostate hyperplasia. Ann Acad Med Singapore. 2010; 39:798–802. PMID: 21063641.
10. Lieber MM, Rhodes T, Jacobson DJ, McGree ME, Girman CJ, Jacobsen SJ, et al. Natural history of benign prostatic enlargement: long-term longitudinal population-based study of prostate volume doubling times. BJU Int. 2010; 105:214–219. PMID: 19594737.

11. Rhodes T, Girman CJ, Jacobsen DJ, Roberts RO, Lerber MM, Jacobsen SJ. Longitudinal prostate volume in a community-based sample: 7 year followup in the Olmsted County Study of Urinary Symptoms and Health Status among Men [abstract]. J Urol. 2000; 163(Suppl 4):249. Abstract No. 1105. PMID: 10604369.
12. Marberger MJ, Andersen JT, Nickel JC, Malice MP, Gabriel M, Pappas F, et al. Prostate volume and serum prostate-specific antigen as predictors of acute urinary retention. Combined experience from three large multinational placebo-controlled trials. Eur Urol. 2000; 38:563–568. PMID: 11096237.
13. Boyle P, Gould AL, Roehrborn CG. Prostate volume predicts outcome of treatment of benign prostatic hyperplasia with finasteride: meta-analysis of randomized clinical trials. Urology. 1996; 48:398–405. PMID: 8804493.

Table 1
Baseline characteristics of the men with prostate volume larger than 80 mL (n=50)
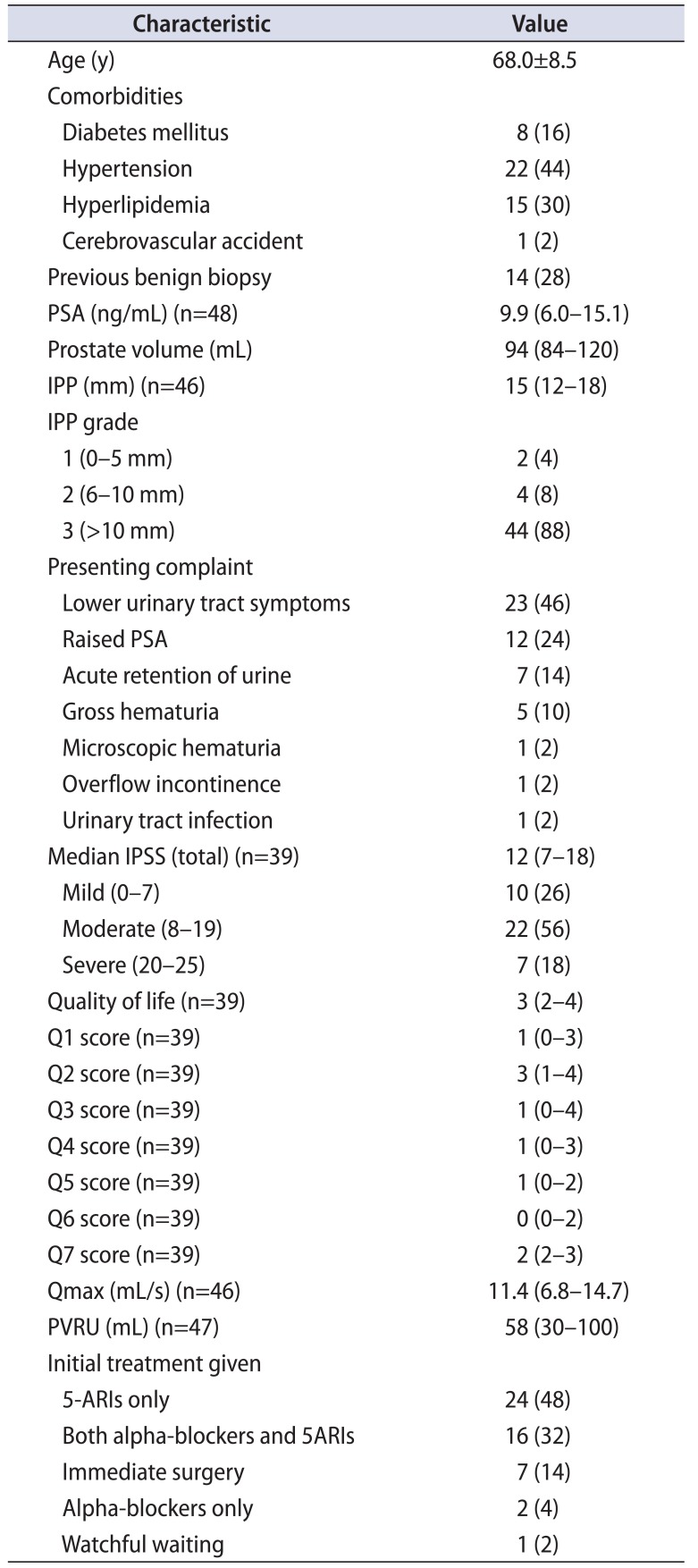
Table 2
Comparison between presentation and follow-up data (median follow-up 62 months) of the 43 men who were treated with conservative therapy
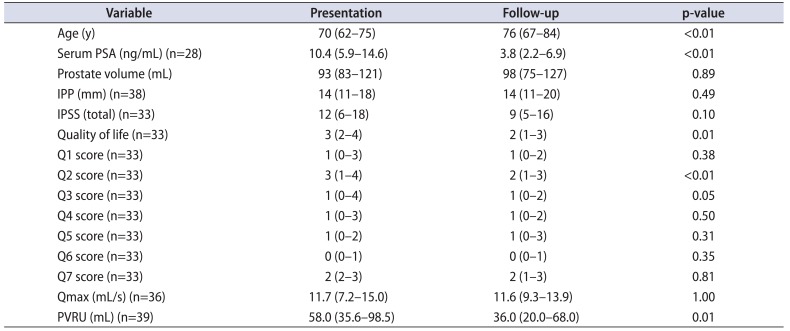
Table 3
Clinical progression of the 43 men who were managed with initial conservative therapy after a median follow-up of 62 months




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download