Abstract
Nephrolithiasis is a disease common in both the Western and non-Western world. Several population based studies have demonstrated a rising prevalence and incidence of the disease over the last several decades. Recurrence occurs frequently after an initial stone event. The influence of diet on the risk of nephrolithiasis is important, particularly dietary calcium and fluid intake. An increasing intake of dietary calcium and fluid are consistently associated with a reduced risk of incident nephrolithiasis in both men and women. Increasing evidence suggests that nephrolithiasis is associated with systemic diseases like obesity, diabetes, and cardiovascular disease. Nephrolithiasis places a significant burden on the health care system, which is likely to increase with time.
Nephrolithiasis is one of the most common urological conditions. In fact, recent estimates place the prevalence in the United States (US) population at 10.6% for men and 7.1% for women [1]. In addition, the lifetime risk of developing a systematic stone event has continued to increase over the last several decades [2]. With these trends likely to continue, it is important for urologists, nephrologists, and primary care physicians to be familiar with the epidemiology of this disease. In this review, we discuss the prevalence, incidence, recurrence, impact of environmental factors, association of diet, and the burden on the health care system of nephrolithiasis.
Several investigations have reported an increased prevalence of nephrolithiasis. The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional probability survey of the civilian noninstitutionalized US population, which is used to estimate the prevalence of kidney stones [13]. An analysis of the survey in 1994 demonstrated an increase in the lifetime prevalence in 20- to 74-year-old adults from 3.2% in 1976–1980 to 5.2% in 1988–1994 [3]. A contemporary analysis of the 2007–2010 survey revealed a continued increase in the overall unadjusted prevalence to 8.8% [1]. Men were more likely to report a history of kidney stones than were women (10.6% vs. 7.1%) (Table 1) [1]. There was also an increase in the prevalence with increasing age group [1]. For example, the prevalence in 20- to 29-year-old adults was 3.1% for both men and women, which then increased and peaked in 60- to 69-year-old adults at 19.1% in men and 9.4% in women [1]. Differences were also observed in race and ethnicity. White, non-Hispanic individuals had the highest prevalence followed by Hispanic individuals and then non-Hispanic Black individuals (10.3% vs. 6.4% vs. 4.3%, respectively) [1]. Compared to individuals earning more than US $75,000 those individuals earning <US $19,999 were associated with an increased risk of reporting a history of kidney stone disease (odds ratio [OR], 1.57; 95% confidence interval [CI], 1.17–2.09) [1].
One limitation of the NHANES study was that it is subject to recall bias, as the diagnosis of kidney stones was self-reported. Furthermore, patients tend to recall only symptomatic stone events. We do know that asymptomatic stones are relatively common. In a retrospective study of 5,047 patients who underwent computed tomography colonography screening at a single institution between 2004 and 2008, a total of 395 patients (7.8%) were identified with urolithiasis (391 renal stones, 6 ureteral stones, and 2 bladder stones) [4]. This represented a total of 814 stones with a mean stone size of 3.0 mm and a mean number of stones per patient of 2.1 [4]. Of the 395 patients with urolithiasis, only 36 (9.1% or 0.7% of the entire cohort), developed a future symptomatic stone event at a mean of 1.3 years following detection [4].
The incidence of symptomatic nephrolithiasis is best approximated from the community based cohort in Rochester Minnesota. At initial diagnosis, the mean age was 44.8 years in men and 40.9 years in women [5]. In the original investigation which examined residents from 1950–1974, the overall age-adjusted rate was 109.5 and 36.0 per 100,000 population per year for males and females, respectively [2]. In the update, which included data from 1970–2000, the overall age-adjusted annual rate increased to 140.6 and 65.8 per 100,000 population for males and females, respectively (Table 1) [5]. Therefore, the male to female ratio decreased from 3.1 in 1974 to 1.3 in 2000, which was attributed to a relative decline in male (1.7% per year), but an increase in female (1.9% per year) symptomatic stone events [5]. This relative change led to a stable age- and gender-adjusted overall rate of 121.0 per 100,000 population over the 30 year study period [5]. Although not all patients had a stone available for analysis (only 62% of the total cohort), the primary stone type was calcium oxalate, calcium phosphate, and uric acid in 74%, 20%, and 4% of patients, respectively [5].
Again, the best estimation of the incidence of a recurrent symptomatic renal stone event comes from the Rochester Minnesota community based cohort. The population of Olmsted County, Minnesota was examined from 1984 to 2003 for all validated incident kidney stone formers, which were then followed for a second episode [6]. From this data, the authors were able to develop a prediction tool for stone formers to estimate the risk of a second symptomatic episode [6]. For the first episode, 48% spontaneously passed their stone with confirmation, 33% required surgery for removal, 8% presumably spontaneously passed their stone without confirmation, and 12% had no documentation of passage [6]. This cohort was followed for a median of 11.2 years with recurrence in 11%, 20%, 31%, and 39% at 2, 5, 10, and 15 years, respectively (Table 2) [6]. The prediction tool (Recurrence of Kidney Stone or ROKS nomogram) utilizes only factors known at the time of the initial stone event such as age, male gender, white race, family history, gross hematuria, uric acid stone composition, stone location, additional asymptomatic stone, and prior stone event [6]. Using these variables, a score is generated which provides the individual patient with an estimate of their risk of recurrence at 2, 5, and 10 years [6].
Nephrolithiasis is not isolated to the US, and several other countries, particularly in Asia have started to quantify the burden of this disease in their populations. For example, in an analysis of the 2009 Health Insurance and Review and Assessment Service-National Patient Sample which is representative of the Korean population, the overall annual incidence of nephrolithiasis was estimated to be approximately 457 per 100,000 population [7]. Men had a higher incidence of approximately 589 per 100,000 population as compared to women with an incidence of approximately 326 per 100,000 population [7]. This equated to a male to female ratio of approximately 1.80 [7]. Interestingly, these rates are significantly higher than what was observed in the US population [5]. However, the estimated lifetime prevalence in Korea of 6.0% for men, 1.8% for women, and 3.5% overall was significantly lower than what was observed in the US population [8].
In Taiwan, a similar population based analysis using the Longitudinal Health Insurance Database 2005 demonstrated that the prevalence in 2010 was 9.0%, 5.8% and 7.4% in males, females, and overall, respectively [9]. The overall prevalence peaked at 19.4% in 60- to 69-year-old adults in that country [9]. Recurrence was also common; observed in 6.1%, 15.8%, 22.8%, 29.1%, and 34.7% adults at 1, 2, 3, 4, and 5 years, respectively [9]. Recurrence was more frequent in males as compared to females [9]. These estimates are very similar to what was observed in the US population [16].
In Japan, a cross-sectional study of the population demonstrated a rise in the annual overall incidence of nephrolithiasis from 54.2 per 100,000 population in 1965 to 114.3 per 100,000 population in 2005 [10]. Again, men had a higher incidence than woman at all time points from 1965 to 2005 [10]. In 2005, the peak incidence was 40–49 for men and 50–59 for woman with a rate of 315.3 and 129.8 per 100,000 population, respectively [10]. Stone analysis demonstrated that over 90% of the stones were calcium based, similar to what was observed in the US population [510].
One of the first investigations into the geographic variation of nephrolithiasis was the second Cancer Prevention Survey (CPS), which was conducted in 1982 and had over 1 million participants [11]. In this study, individuals were asked if they ever had a diagnosis of kidney stones. Stone prevalence was stratified by latitude and region. According to latitude, men living in the southern most latitude were 60% more likely to report a history of stones than those living in the northern most latitude (prevalence ratio [PR], 1.60; 95% CI, 1.49–1.72) [11]. A similar trend was also observed for women (PR, 1.45; 95% CI, 1.31–1.61) [11]. When compared by region, both men and women living in the Southeast were nearly twice as likely to have a history of kidney stones as compared to those living in the Northwest (men: PR, 1.79; 95% CI, 1.69–1.89 and women: PR, 1.84; 95% CI, 1.69–2.00) [11]. Overall, stone prevalence increases from west to east, but also, and more pronounced form north to south in the US (Table 3) [11]. This is why the states of North Carolina, South Carolina, Georgia, Alabama, Mississippi, and Tennessee are considered in the “stone belt.”
At least part of this observed variation is likely related to ambient temperature. In a follow-up analysis to the CPS, additional data related to mean temperature, sunlight index, and beverage consumption was collected for both men and women [12]. Both an increase in ambient temperature and sunlight index were independently associated with an increased prevalence of kidney stone disease [12]. Furthermore, when controlling for these factors, the regional variation in kidney stones was either eliminated or reduced [12]. This further supports their role in the development of kidney stones especially in the Southeast, where both ambient temperature and sunlight index tend to be higher [12]. This may also explain the seasonal variation in the rate of incident stone events, which are higher during the warmer summer months than the colder winter months [13]. In yet another analysis, utilizing ambient temperature and a cohort of commercially insurance patients, the relative risk of kidney stone presentation was demonstrated to increase for 4 major cities during a 20-day period associated with a mean daily temperature of 30℃ compared with 10℃ [14]. For example, the relative risk was 1.37 in Chicago (95% CI, 1.07–1.76) and 1.47 in Philadelphia (95% CI, 1.00–2.17) at temperatures of 30℃ compared with 10℃ [14]. There was also a gradient observed for each 2℃ increase in ambient temperature above 10℃ [14]. Lastly, the lag between a high daily temperature and an observed increase in kidney stone events was short, only 3 days [14].
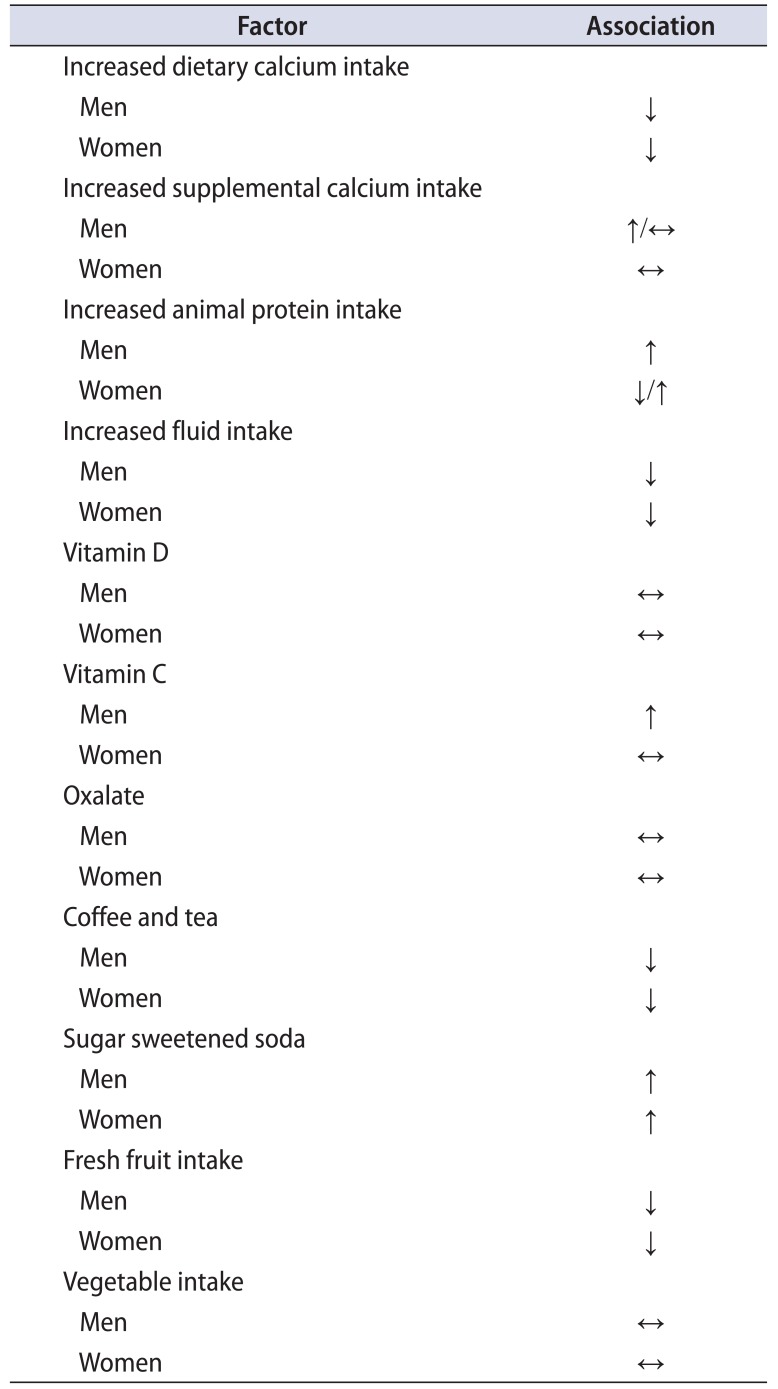
Several investigations have attempted to answer the question of how diet influences the development of kidney stones (Table 4). Restriction of dietary calcium was once thought to be a prevention strategy. However, in 1986, researchers utilizing the Health Professionals Follow-Up Study (HPFS) determined that men who later developed kidney stones had a lower mean calcium intake than men who never developed a kidney stone [15]. In fact, the relative risk for men in the highest quintile for calcium intake as compared to the lowest intake was 0.56 (95% CI, 0.43–0.73) [15]. In contrast to increased dietary calcium intake, supplemental calcium intake increased the risk of kidney stones with a relative risk of 1.23 (95% CI, 0.84–1.79) [15]. Additional dietary factors associated with the risk of kidney stones in men included increased animal protein intake (RR, 1.33), potassium intake (RR, 0.49), and fluid intake (RR, 0.71) [15] .The intakes of sodium, magnesium, phosphorus, fiber, sucrose, and sugared cola were not associated with kidney stone formation [15].
In 2000, the HPFS was re-evaluated with now 14 years of follow-up in the men. In the updated analysis, there still existed an association between the intake of dietary calcium and the risk of incident kidney stones. However, it was age-specific. In men younger than 60 years of age, the RR for stone formation in the highest quintile of dietary calcium as compared with the lowest quintile was 0.69 (95% CI, 0.56–0.87) [16]. In men older than 60 years of age, there was no association [16]. Additional factors associated with the risk of kidney stones in men at longer follow-up included vitamin C intake (RR, 1.41), magnesium intake (RR, 0.71), potassium intake (RR, 0.54), fluid intake (RR, 0.71), and animal protein intake only in men with a body mass index<25 kg/m2 (RR, 1.38) [16]. Sodium, phosphorus, sucrose, phytate, vitamin B6, vitamin D, and supplemental calcium intake had no association [16].
Similar to the HPFS, which only examined men, the Nurses' Health Study (NHS) II provided epidemiologic data on women. This analysis confirmed the same finding in women that a higher dietary calcium intake was associated with a reduced risk of kidney stones [17]. The relative risk among women in the highest quintile of calcium intake compared with women in the lowest quintile was 0.54 (95% CI, 0.45–0.63) [17]. Interestingly, unlike in men, intake of supplemental calcium was not significantly associated with the risk of kidney stones in women [17]. Additional dietary factors associated with the risk of kidney stones in woman included increased animal protein intake (RR, 0.84), phytate intake (RR, 0.63), fluid intake (RR, 0.68), and sucrose intake (RR, 1.31) [17]. The intakes of sodium, potassium, magnesium, and phosphorus were not associated with kidney stone formation [17].
The Women's Health Initiative Observational Study was recently analyzed to determine the association of calcium, sodium, and protein intake with the risk of incident nephrolithiasis [18]. Similar to the NHS II analysis, increasing dietary calcium and water intake were both associated with a reduced risk of incident kidney stones [18]. Specifically, an increasing quintile of dietary calcium and fluid intake was associated with a 5%–28% and a 13%–31% decreased risk, respectively [18]. An increasing quintile of dietary sodium intake was associated with a 11%–61% increased risk, but animal protein showed no association [18].
Additional dietary factors thought to be associated with kidney stones include vitamin D, oxalate, and various beverages. Although the data is limited, there appears to be no increased risk associated with vitamin D supplementation when the goal is to return vitamin D to normal levels [19]. Oxalate is of concern as it is a common component of stones. It is obtained both exogenously and endogenously. Although increased ingestion of oxalate rich foods does result in increased urinary oxalate excretion, the balance is also influenced by dietary calcium intake [19]. Therefore, its true association with kidney stone formation is likely variable, and difficult to quantify. Lastly, various beverages are associated with kidney stones. As discussed earlier, increased fluid intake is associated with a reduced risk [151617]. Coffee and tea are also associated with a reduced risk, while various sodas are associated with an increased risk [19]. Interestingly, an analysis of the HPFS and NHS I and II demonstrated no association of increasing total energy intake or physical activity with incident symptomatic nephrolithiasis [20].
The associations observed in these epidemiological studies in the US also hold true in other developed nations. In the United Kingdom (UK), the Oxford arm of the European Prospective Investigation into Cancer and Nutrition cohort was utilized to assess the relationship of dietary factors to incident kidney stones in over 51,000 individuals from 1993–1999 [21]. In their analysis, individuals were compared based on the quantity of meat in their diet. When compared to high meat-eaters (100 g/d), those who were moderate meat-eaters (50–99 g/d), low meat-eaters (<50 g/d), fish-eaters, and vegetarians all demonstrated a significantly reduced risk of nephrolithiasis (hazard ratio [HR], 0.80, 0.52, 0.73, and 0.69, respectively) [21]. Interestingly, neither total protein nor fat were associated with kidney stones [21]. Additional food groups were also associated with kidney stones. For example, fresh fruit intake in the highest as compared to the lowest third demonstrated a reduced risk with a HR of 0.70 [21]. However, the same trend was not observed for intake of vegetables [21]. In terms of mineral intake, there were no associations between dietary consumption of sodium or calcium [21].
Traditionally, nephrolithiasis was thought to be a disease related to diet and abnormal renal handling of electrolytes. However, recent investigations have suggested that kidney stones may in fact be a marker of more serious systemic disorders like diabetes, hypertension, and cardiovascular disease.
NHANES III conducted from 1988–1994 was a cross-sectional survey study designed to obtain nationally representative estimates of the health and nutritional status of the US population [22]. NHANES III included data on bone mineral density (BMD). An analysis of NHANES III, demonstrated that a history of kidney stones was significantly associated with a lower BMD in men, but not women [22]. Similarly, men, but not women with a reported history of kidney stones were more likely to report wrist (OR, 1.68) and spine fracture (OR, 2.32) [22].
In a more contemporary retrospective cohort study using The Health Improvement Network from the UK, the authors found a significant association of a history of urolithiasis with incident fracture [23]. This was not age dependent in men with an overall HR of 1.13 (95% CI, 1.08–1.18) for fracture [23]. However, age dependence was noted in women with an increase from the third through seventh decades of life [23]. This peaked in women aged 30–39 years with a HR of 1.55 (95% CI, 1.26–1.90) [23]. After adjustment for various medications such as Thiazides and systemic diseases such as diabetes, a diagnosis of urolithiasis remained significantly associated with an incident risk of fracture [23].
A concern of patients is the potential renal loss and subsequent need for dialysis after a kidney stone event. Using the Olmsted County cohort via the Rochester Epidemiology Project, a case-control study demonstrated that stone formers were more likely to receive a diagnosis of clinical chronic kidney disease (CKD) as compared to control subjects (HR, 1.67; 95% CI, 1.48–1.88) [24]. However, there was not an increased risk for ESRD or death with CKD in stone formers as compared to controls [24]. Another prospective US population based cohort study demonstrated conflicting results. In their analysis of the Atherosclerosis Risk in Communities study, there was no association with a history of nephrolithiasis and incidence CKD stage III or greater after multivariable adjustment [25].
However, the opposite was again demonstrated in a population based cohort study in Canada. In this population, there was a significantly higher risk of incident end-stage renal disease (ESRD) with one or more episodes of kidney stones (HR, 2.16; 95% CI, 1.79–2.62) as compared to those without a history of stones [26]. A similar increased risk was also observed for CKD, stages IIIB-IV (HR, 1.74; 95% CI, 1.61–1.88) and for a doubling of creatinine from baseline (HR, 1.94; 95% CI, 1.56–2.43) [26]. Although significant, the magnitude of events was small. For example, the unadjusted rate of ESRD was 2.48 and 0.52 per million person days in people with a history of stones as compared to those without stones, respectively [26].
Utilizing data from NHANES III researchers attempted to confirm a graded association of an increasing number of metabolic syndrome traits with the risk of kidney stone disease [27]. In the NHANES III population, 33.3% were confirmed to have the metabolic syndrome, but only 4.7% had a history of kidney stones [27]. However, there was a clear association of metabolic syndrome traits with nephrolithiasis. Kidney stone disease was reported in 3%, 7.5%, and 9.8% of individuals with 0, 3, and 5 traits of the metabolic syndrome, respectively [27]. This trend was also observed in a multivariate analysis where 1, 2, 3, 4, and 5 traits of the metabolic syndrome resulted in increasing ORs of 1.19 (95% CI, 0.74–1.93), 1.54 (95% CI, 1.02–2.32), 1.70 (95% CI, 1.06–2.72), 2.31 (95% CI, 1.54–3.48), and 1.93 (95% CI, 1.08–3.43), respectively [27]. A similar association was also demonstrated in the updated NHANES cohort. In an analysis of the 2007–2010 NHANES, components of the metabolic syndrome were associated with a reported history of kidney stones: obesity (OR, 1.54; 95% CI, 1.25–1.94), diabetes (OR, 1.59; 95% CI, 1.22–2.07), and gout (OR, 1.92; 95% CI, 1.44–2.56) [1].
The association of the metabolic syndrome with kidney stone disease is not isolated to Western populations. For example, in a cross-sectional study of Japanese individuals who were divided into 3 groups based on stone status (controls, a past stone, and a current stone), there was a positive association between nephrolithiasis and the traits of overweight/obesity, hypertension, and gout/hyperuricemia [28]. Interestingly, there was no association with the trait of diabetes [28]. There was a dose-response relationship observed with an increasing risk between the control, past, and current stone groups [28].
Again, utilizing the updated NHANES cohort from 2007–2010 researchers were able to demonstrate a similar graded association of diabetes severity with a history of kidney stone disease. Overall, a self-reported history of diabetes resulted in over a twofold increased odds of a reported history of kidney stone disease (OR, 2.44; 95% CI, 1.84–3.25) [29]. This was even more pronounced for a reported history of insulin use (OR, 3.31; 95% CI, 2.02–5.45) [29]. When factoring in the severity of diabetes using fasting plasma glucose and glycosylated hemoglobin (HbA1c) levels there was also a clear association. For individuals with a fasting plasma glucose of 100–126 mg/dL, the OR of having kidney stone disease was only 1.28 (95% CI, 0.95–1.72), but when the level was >126 mg/dL the OR increased to 2.29 (95% CI, 1.68–3.12) [29]. This was even more pronounced with HbA1c, which at values of 5.7%–6.4% demonstrated an OR of 1.68 (95% CI, 1.17–2.42), increasing to an OR of 2.82 (95% CI, 1.98–4.02) at a HbA1c >6.5% [29].
Equally as concerning is the association of cardiovascular disease with nephrolithiasis. In the HPFS, men with a history of nephrolithiasis as compared to those without had a 29% increased odds of incident hypertension during the 8 years of follow-up (OR, 1.29; 95% CI, 1.12–1.41) [30]. The converse, however, was not observed. In men with a history of hypertension, there was no association with later development of nephrolithiasis (OR, 0.99; 95% CI, 0.82–1.21) [30]. Interestingly, in men with both nephrolithiasis and hypertension at baseline, almost 80% reported that their kidney stones proceeded or were concomitant with the diagnosis of hypertension [30]. A similar association was observed in women. Using the NHS cohort there was a 24% increased risk of developing incident hypertension in women with a history as compared to those without a history of kidney stone disease (RR, 1.24; 95% CI, 1.13–1.37) [31]. There was no association between baseline hypertension and later development of kidney stones [31]. In a larger analysis of both the HPFS and NHS there was no association of a history of nephrolithiasis with cardiovascular disease in men, but there was an association in women after multivariable adjustment [32]. In women with a history of kidney stones there was an increased risk of cardiovascular disease (HR, 1.30; 95% CI, 1.04–1.62), fatal and non-fatal myocardial infarction (HR, 1.26; 95% CI, 1.11–1.43), and revascularization (HR, 1.29; 95% CI, 1.07–1.55) [32]. Other cohort studies have demonstrated a consistent association of kidney stone disease with cardiovascular outcomes [33].
In 2005, the Urologic Diseases of America Project attempted to quantify the burden of urolithiasis on the US health care system. Utilizing the Healthcare Cost and Utilization Project (HCUP) data set the investigators demonstrated a rate of hospitalization for upper tract stones of 62 per 100,000 population in 2000 [34]. However, when using the Medicare data set, the investigators found a 2.5–3.0 times higher rate of hospitalization [34]. For example, in 1998, the overall rate was 71 per 100,000 population in the HCUP data set, while for Medicare beneficiaries the overall rate was 184 per 100,000 population [34]. There did appear to be a difference between males and females. Males had a higher rate of hospitalization than females, but the male-to-female ratio decreased from 1.86 in 1994 to 1.45 in 2000 [34]. In the HCUP data set, White individuals had the highest rate of hospitalization, which was also noted in the Medicare population [34]. The average length of stay was 2.2 days and 3.0 days in 2000 in the HCUP and Medicare groups, respectively [34].
Emergency Department visits in 2000 totaled 617,647 with an overall rate of 226 per 100,000 population [34]. The rate was twice as high for males than females [34]. When examining ambulatory visits, which included both outpatient hospital and physician office visits, the overall age-adjusted rate where urolithiasis was the primary diagnosis was 731 per 100,000 population in 2000 [34]. In only 8 years, the outpatient visit number nearly doubled from 950,000 in 1992 to 1,825,000 in 2000 [34]. For surgical procedures performed in an ambulatory surgery center, Medicare beneficiaries had 66,580 visits in 1998 with an age-adjusted overall visit rate of 199 per 100,000 population, which increased from 123 per 100,000 population in 1992 [34]. A similar trend was also observed in commercially insured patients [34]. Shock-wave lithotripsy, ureteroscopy, and percutaneous nephrolithotomy comprised 51%–54%, 40%–41%, and 3%–4% of procedures, respectively in 1998 in Medicare beneficiaries [34]. Again, similar results were also observed in the commercially insured population [34].
In 2000, the total cumulative costs for caring for patients with urolithiasis were estimated at US $2.1 billion. This included US $971 million, US $607 million, and US $490 million for inpatient, outpatient, and emergency services, respectively [34]. From 1994 to 2000, this cost increased 50% with outpatient services increasing to 53% of the total [34]. Due to population growth and the rising prevalence of obesity and diabetes, the cost to care for stone disease is estimated to increase by US $1.24 billion per year by 2030 [35]. At the individual level, the estimated annual additional cost of medical care including prescription coverage for a diagnosis of urolithiasis was US $4,472 per capita in 1999 [34]. This also resulted in 30% of employed individuals who made a claim for urolithiasis reporting missed days of work, which equated to a mean of 19 hours of missed work per year [34].
Epidemiological studies of nephrolithiasis have demonstrated increasing prevalence and incidence of the disease over the last several decades. Although men continue to be affected more often, women are increasingly closing the gender gap. Recurrence remains a significant cause of the morbidity of the disease. Environment continues to play a role. Dietary factors are important and are potentially modifiable. Nephrolithiasis is now thought of not only as a disease of morbidity, but as a marker of potentially lethal conditions, such as diabetes and cardiovascular disease. Lastly, kidney stone disease continues to be a significant burden on the health care system.
References
1. Scales CD Jr, Smith AC, Hanley JM, Saigal CS. Urologic diseases in America project. Prevalence of kidney stones in the United States. Eur Urol. 2012; 62:160–165. PMID: 22498635.

2. Johnson CM, Wilson DM, O'Fallon WM, Malek RS, Kurland LT. Renal stone epidemiology: a 25-year study in Rochester, Minnesota. Kidney Int. 1979; 16:624–631. PMID: 548606.

3. Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003; 63:1817–1823. PMID: 12675858.
4. Boyce CJ, Pickhardt PJ, Lawrence EM, Kim DH, Bruce RJ. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010; 183:1017–1021. PMID: 20092842.

5. Lieske JC, Peña de la Vega LS, Slezak JM, Bergstralh EJ, Leibson CL, Ho KL, et al. Renal stone epidemiology in Rochester, Minnesota: an update. Kidney Int. 2006; 69:760–764. PMID: 16518332.

6. Rule AD, Lieske JC, Li X, Melton LJ 3rd, Krambeck AE, Bergstralh EJ. The ROKS nomogram for predicting a second symptomatic stone episode. J Am Soc Nephrol. 2014; 25:2878–2886. PMID: 25104803.

7. Bae SR, Seong JM, Kim LY, Paick SH, Kim HG, Lho YS, et al. The epidemiology of reno-ureteral stone disease in Koreans: a nationwide population-based study. Urolithiasis. 2014; 42:109–114. PMID: 24526235.

8. Kim HH, Jo MK, Kwak C, Park SK, Yoo KY, Kang D, et al. Prevalence and epidemiologic characteristics of urolithiasis in Seoul, Korea. Urology. 2002; 59:517–521. PMID: 11927302.

9. Huang WY, Chen YF, Carter S, Chang HC, Lan CF, Huang KH. Epidemiology of upper urinary tract stone disease in a Taiwanese population: a nationwide, population based study. J Urol. 2013; 189:2158–2163. PMID: 23313204.

10. Yasui T, Iguchi M, Suzuki S, Kohri K. Prevalence and epidemiological characteristics of urolithiasis in Japan: national trends between 1965 and 2005. Urology. 2008; 71:209–213. PMID: 18308085.

11. Soucie JM, Thun MJ, Coates RJ, McClellan W, Austin H. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 1994; 46:893–899. PMID: 7996811.

12. Soucie JM, Coates RJ, McClellan W, Austin H, Thun M. Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am J Epidemiol. 1996; 143:487–495. PMID: 8610664.

13. Fakheri RJ, Goldfarb DS. Ambient temperature as a contributor to kidney stone formation: implications of global warming. Kidney Int. 2011; 79:1178–1185. PMID: 21451456.

14. Tasian GE, Pulido JE, Gasparrini A, Saigal CS, Horton BP, Landis JR, et al. Daily mean temperature and clinical kidney stone presentation in five U.S. metropolitan areas: a time-series analysis. Environ Health Perspect. 2014; 122:1081–1087. PMID: 25009122.

15. Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med. 1993; 328:833–838. PMID: 8441427.

16. Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. 2004; 15:3225–3232. PMID: 15579526.

17. Curhan GC, Willett WC, Knight EL, Stampfer MJ. Dietary factors and the risk of incident kidney stones in younger women: Nurses' Health Study II. Arch Intern Med. 2004; 164:885–891. PMID: 15111375.
18. Sorensen MD, Kahn AJ, Reiner AP, Tseng TY, Shikany JM, Wallace RB, et al. Impact of nutritional factors on incident kidney stone formation: a report from the WHI OS. J Urol. 2012; 187:1645–1649. PMID: 22425103.

19. Friedlander JI, Antonelli JA, Pearle MS. Diet: from food to stone. World J Urol. 2015; 33:179–185. PMID: 24938177.

20. Ferraro PM, Curhan GC, Sorensen MD, Gambaro G, Taylor EN. Physical activity, energy intake and the risk of incident kidney stones. J Urol. 2015; 193:864–868. PMID: 25229560.

21. Turney BW, Appleby PN, Reynard JM, Noble JG, Key TJ, Allen NE. Diet and risk of kidney stones in the Oxford cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC). Eur J Epidemiol. 2014; 29:363–369. PMID: 24752465.

22. Lauderdale DS, Thisted RA, Wen M, Favus MJ. Bone mineral density and fracture among prevalent kidney stone cases in the Third National Health and Nutrition Examination Survey. J Bone Miner Res. 2001; 16:1893–1898. PMID: 11585355.

23. Denburg MR, Leonard MB, Haynes K, Tuchman S, Tasian G, Shults J, et al. Risk of fracture in urolithiasis: a population-based cohort study using the health improvement network. Clin J Am Soc Nephrol. 2014; 9:2133–2140. PMID: 25341724.

24. Rule AD, Bergstralh EJ, Melton LJ 3rd, Li X, Weaver AL, Lieske JC. Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol. 2009; 4:804–811. PMID: 19339425.

25. Kummer AE, Grams M, Lutsey P, Chen Y, Matsushita K, Köttgen A, et al. Nephrolithiasis as a risk factor for CKD: the Atherosclerosis Risk in Communities study. Clin J Am Soc Nephrol. 2015; 10:2023–2029. PMID: 26342045.

26. Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Morgan C, Samuel S, et al. Kidney stones and kidney function loss: a cohort study. BMJ. 2012; 345:e5287. PMID: 22936784.

27. West B, Luke A, Durazo-Arvizu RA, Cao G, Shoham D, Kramer H. Metabolic syndrome and self-reported history of kidney stones: the National Health and Nutrition Examination Survey (NHANES III) 1988-1994. Am J Kidney Dis. 2008; 51:741–747. PMID: 18436084.

28. Ando R, Nagaya T, Suzuki S, Takahashi H, Kawai M, Okada A, et al. Kidney stone formation is positively associated with conventional risk factors for coronary heart disease in Japanese men. J Urol. 2013; 189:1340–1346. PMID: 23159273.

29. Weinberg AE, Patel CJ, Chertow GM, Leppert JT. Diabetic severity and risk of kidney stone disease. Eur Urol. 2014; 65:242–247. PMID: 23523538.

30. Madore F, Stampfer MJ, Rimm EB, Curhan GC. Nephrolithiasis and risk of hypertension. Am J Hypertens. 1998; 11(1 Pt 1):46–53. PMID: 9504449.

31. Madore F, Stampfer MJ, Willett WC, Speizer FE, Curhan GC. Nephrolithiasis and risk of hypertension in women. Am J Kidney Dis. 1998; 32:802–807. PMID: 9820450.

32. Ferraro PM, Taylor EN, Eisner BH, Gambaro G, Rimm EB, Mukamal KJ, et al. History of kidney stones and the risk of coronary heart disease. JAMA. 2013; 310:408–415. PMID: 23917291.

33. Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Samuel S, Klarenbach SW, et al. Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol. 2014; 9:506–512. PMID: 24311706.

34. Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J Urol. 2005; 173:848–857. PMID: 15711292.

35. Antonelli JA, Maalouf NM, Pearle MS, Lotan Y. Use of the National Health and Nutrition Examination Survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur Urol. 2014; 66:724–729. PMID: 25015037.

Table 1
Contemporary prevalence and incidence of nephrolithiasis
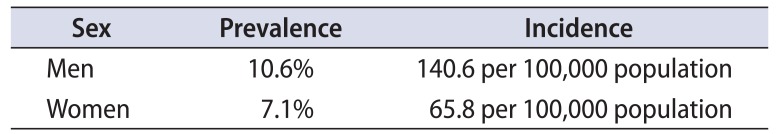
| Sex | Prevalence | Incidence |
|---|---|---|
| Men | 10.60% | 140.6 per 100,000 population |
| Women | 7.10% | 65.8 per 100,000 population |
Table 2
Risk of a recurrent stone event
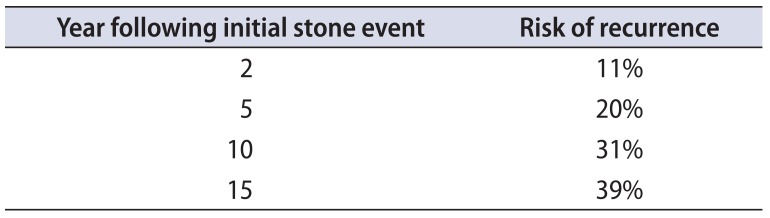
| Year following initial stone event | Risk of recurrence |
|---|---|
| 2 | 11% |
| 5 | 20% |
| 10 | 31% |
| 15 | 39% |
Adapted from Rule et al. [6].
Table 3
Environmental associations with nephrolithiasis
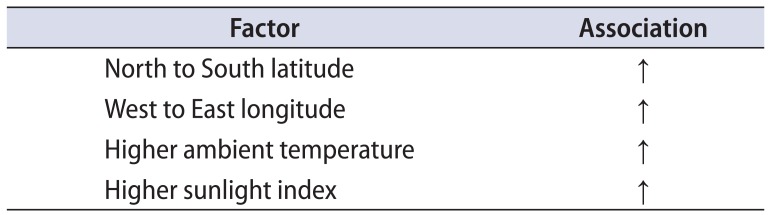
| Factor | Association |
|---|---|
| North to South latitude | ↑ |
| West to East longitude | ↑ |
| Higher ambient temperature | ↑ |
| Higher sunlight index | ↑ |
Table 4
Dietary associations with nephrolithiasis




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download