This article has been corrected. See "Corrigendum: Correction of the Acknowledgment.Prevalence and management status of urologic disease in geriatric hospitals in South Korea: A population-based analysis" in Volume 59 on page 220.
Abstract
Purpose
This study aimed to investigate the prevalence and management status of urologic disease in geriatric hospitals in Korea.
Materials and Methods
We conducted population-based analyzed using cohort established by the National Health Insurance Service of Korea, which contains the medical insurance data of 1 million people from 2002 to 2013. The prevalence, prescription rate, and complication incidence of urologic disease in geriatric hospitals were compared with similar-sized general hospitals. We analyzed the changes that followed the adoption of the fixed sum medical fee per day for geriatric hospitals, which began in January 2008. Subgroup analysis was conducted in an elderly group and a propensity score matching (PSM) group.
Results
During this time, the number of geriatric hospitals exponentially increased over general hospitals (675.5%/y vs. 30.9%/y). The prevalence, prescription rate, and complication incidence of urologic disease was higher in geriatric hospitals than in general hospitals (2.1, 1.8, and 1.4 times higher). In the elderly group, the prevalence of urologic disorders was higher in geriatric hospitals than in general hospitals, but the prescription rate was lower (26.5% vs. 19.9% and 6.8% vs. 10.0%). This tendency also founded in the PSM analysis. After the medical fee system changed, diagnosis and prescription rates decreased in geriatric hospitals but increased in general hospitals.
The world's population is aging. Most developed countries already have a substantially greater proportion of elderly citizens; Japan became the country with the most aged population in the world in 2015 [1]. Likewise, Korea has one of the most rapidly aging populations. Based on the ratio of the elderly (65 years and over) to the entire population, Korea joined the list of aging societies (7%–14%) in 2000 and is expected to become an aged society (14%–20%) in 2018 [2].
Elderly patients are different from general population patients. First, most of patients have at least one chronic disease at the time of admission. According to the “2014 elderly report,” 90% of elderly people have a chronic disease and 31.5% have cognitive impairments that require daily support [3]. Second, patient needs longer hospitals stay than general population. Bo et al. [4] reported that cognitive impairment and functional dependency prolonged hospital stay in general hospitals. For this reason, the demand for geriatric hospital that manages elderly patient's chronic disease and long term care is increasing.
Urologic disease is common in elderly populations and is closely associated with quality of life (QoL) [56]. However, most urologic diseases are not life-threatening, so they are easily neglected by health care providers [5]. Patients also regard these symptoms as part of the normal process of aging [7]. Moreover, limited reimbursement for medical expenses adversely affects urologic disease management. In January 2008, the medical payment system of geriatric hospitals changed from a fee-for-service model to a fixed sum medical fee per day (FSMFD) system, which provides a fixed daily medical insurance fee. The role of the urologist is important in geriatric hospitals for appropriate management of urologic problems. However, presently, there are few urologists working at geriatric hospitals [8].
This research aims to reveal the prevalence and management status of urologic disorders in geriatric hospitals through the National Health Insurance Service-National Sample Cohort (NHIS-NSC). We also looked at how the FSMFD system has influenced the management of urologic disorders in geriatric hospitals.
The NHIS-NSC is a population-based cohort, which represents 2.2% of the Korean population in 2002 [9] which collected by Korea government. During the follow-up period, the cohort was refreshed annually by adding a representative sample of newborns, using the 2.2% sampling rate. Subjects in this cohort were selected by random sampling and followed until 2013. Sampling was carried out based on the stratification and proportional allocation method for national medical insurance data. The cohort includes 1,025,340 participants and the follow-up period was a total of 12 years, from January 2002 to December 2013.
We use medical treatment database and medical care institution database set of NHIS-NSC for this investigation. The ‘medical treatment database’ consists of 57 variables containing information about participants' medical bills claimed by medical service providers. It comprises four databases: participant's electronic medical treatment bills, bill details, details of diseases and details of prescriptions. All four databases are further classified according to type of medicine: ‘medical’ and ‘dental & Korean traditional medicine’ tables. A pharmacy table is also included in the first 2 databases. In the ‘medical care institution database’, information regarding the type of institution, establishment, location, number of beds, facilities and physicians are recorded under 10 variables. These databases were episode based of each years of follow-up period.
This study was approved by the Institutional Review Board of Seoul National University Hospital (approval number: E-1410-080-618).
The prevalence of urologic disorders (N00-N99) and major voiding disorders was assessed by searching for patients with primary or secondary diagnoses of benign prostatic hyperplasia (BPH), overactive bladder (OAB), or neurogenic bladder according to their Korean standard classification of diseases 6 (KCD6) codes. To include diagnoses received after transfer to another hospital, diagnoses received in other hospitals were also checked. The prescription frequency of voiding dysfunction medication was analyzed by the prescription codes within geriatric hospitals—including alpha blockers (tamsulosin, terazosin, doxazosin, alfuzosin, naftopidil, and silodosin), antimuscarinics (oxybutynin, propiverine, tolterodine, solifenacin, fesoterodine, imidafenacin, and trospium), 5-alpha reductase inhibitors (finasteride and dutasteride), antidiuretics (desmopressin), and parasympathomimetics (bethanechol). A detailed list of KCD codes for specific urologic diseases, medication, and complications is included in Supplementary Materials.
A repeat history of chronic complications at any time counted as a single event, and an acute complication counted as a single event if it recurred within a 3-month period. Complications diagnosed following hospital transfer were also considered relevant and were included in our study. Acute and chronic urinary retention, prostatitis, urethritis, cystitis, pyelonephritis, other urinary tract infections, urolithiasis, urethral stricture, and hematuria were defined as urologic complications and dermatitis, bedsores, and renal failure were defined as nonurologic complications. The overall complication incidence was calculated as the sum of each complication incidence and included duplicates.
The payment system of geriatric hospitals in Korea changed after the adoption of the FSMFD, which started in January 2008. Before the FSMFD, medical fees covered by national insurance were reimbursed on a fee-for-service basis, which covered the sum of the costs incurred at each medical practice. The FSMFD provided a fixed daily medical insurance fee, graded by patient disease status (7 steps), an activity of daily living score, and the medical resources required. Since payment system changes can affect medical practices in the field, we evaluated changes before and after the adoption of the FSMFD.
We analyzed the data in 4 sequential steps. First, we compared annual changes of bed counts and hospital numbers from ‘ medical care institution database’. The second step, we selected hospitalized patients in geriatric hospitals and similar-sized general hospitals for compare cumulative incidence of variables in each group; the prescription rate, diagnostic frequency, and the complication rate. Additional analysis was performed before and after the adoption of the FSMFD in geriatric hospitals. In the third step, considering that hospitalized geriatric patients are mostly elderly, we selected patients aged 65 years and older. We compared the diagnostic frequency, complication rate, and changes after the adoption of the FSMFD. In our last step, after filtering out confounding variables through one-toone propensity score matching (PSM) based on age, gender, and presence of stroke and dementia (the top reasons for hospital admittance), we conducted a final comparison of diagnostic frequency, complication rate, and changes after the adoption of the FSMFD. All the statistical analysis was conducted by SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA) and PSM was using computerized matching process, OneToManyMTCH macro for SAS which using greedy matching algorithm.
The number of geriatric hospitals increased from 15 in 2002 to 1,330 in 2013—with an annual growth rate of 675.5%—while the number of general hospitals increased from 393 to 1,826 in the same period, with an annual growth rate of 30.9%. Total bed count in geriatric hospitals grew explosively from 3,058 in 2002 to 230,194 in 2013—an annual average growth rate of 797.0%—while the bed count in general hospitals increased from 58,353 to 256,608 in the same period, or a growth rate of 33.2%. The growth in the number and capacity of geriatric hospitals slowed temporarily between 2008 and 2009 when the FSMFD was adopted but demonstrated continuous growth afterwards (Fig. 1).
The prevalence for all urologic disease was 24.5% (6,821 of 27,841 patients) in geriatric hospitals, 2.1 times higher than the 11.5% (34,230 of 297,660 patients) found in general hospitals. The diagnosis of all major voiding disorders was more frequent in geriatric hospitals and the relative risk (RR) was 1.9 (p<0.001; 95% confidence interval [CI], 1.858–2.022), 1.3 (p<0.001; 95% CI, 1.206–1.404), and 1.8 (p<0.001; 95% CI, 1.673–1.877) for BPH, OAB, and neurogenic bladder, respectively.
The institutional prescription rate of voiding dysfunction medication in geriatric hospitals was 6.2% on average (1,726 of 27,841 patients), which was 1.8 times higher than the 3.5% (10,340 of 297,660 patients) prescription rate of general hospitals. Alpha-blockers, 5-alpha reductase inhibitors, and parasympathomimetics were prescribed more frequently in geriatric hospitals, while the prescription rate for antidiuretics was similar for geriatric hospitals and general hospitals.
The total cumulative incidence of complication was 70.9% in geriatric hospitals and 51.5% in general hospitals, including duplicates. Urinary retention, urinary tract infection, urethral stricture, hematuria, bedsores, and renal failure occurred more frequently in geriatric hospitals. Urolithiasis and skin infections were more prevalent in general hospitals than geriatric hospitals.
The prevalence of urologic diseases and the associated prescription rate in geriatric hospitals dropped after the adoption of the FSMFD. In contrast, the prevalence in general hospitals did not change significantly; the prescription rate actually increased. (Fig. 2A, B) In terms of specific diseases, the prevalence of BPH and neurogenic bladder decreased in geriatric hospitals, while OAB increased. The complication incidence increased in general hospitals, while it decreased in geriatric hospitals.
The prevalence of urologic disorders in elderly patients in geriatric hospitals was 26.5%, which is 1.3 times that of the 19.9% found in general hospitals. Among the major urologic disorders, only OAB was higher in geriatric hospitals, with an RR of 1.23 (p<0.001; 95% CI, 1.128–1.356). The prevalence of BPH and neurogenic bladder was lower in geriatric hospitals, with an RR of 0.65 (p<0.001; 95% CI, 0.622–0.684) and 0.86 (p<0.001; 95% CI, 0.811–0.927), respectively. The prescription rate in geriatric hospitals was lower than that of general hospitals as well. The prescription rates of alphablockers, 5-alpha reductase inhibitors, antimuscarinics, antidiuretics, and parasympathomimetics were all lower in geriatric hospitals. The complication incidence was similar in each group: 76.35% in general hospitals and 73.37% in geriatric hospitals.
In geriatric hospitals, only the diagnostic rate of OAB increased, while the diagnosis of all major urologic diseases increased in general hospitals after adoption of the FSMFD. The prescription rates of all urologic medications decreased in geriatric hospitals, but increased in general hospitals. The complication incidence increased in general hospitals from 64.32% to 81.54%. In geriatric hospitals, the complication incidence decreased from 96.78% to 69.58%.
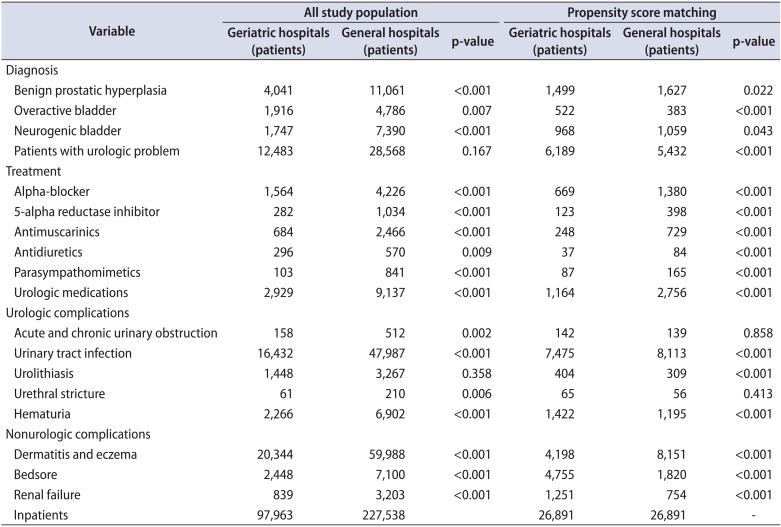
About 26,891 patients within 97,963 in geriatric hospital was selected for propensity matching analysis with same amount of matched population in general hospital (Table 1). The diagnostic rates of BPH (RR, 0.92; p=0.018; 95% CI, 0.861–0.986) and neurogenic bladder (RR, 0.91; p=0.039; 95% CI, 0.839–0.996) were lower in geriatric hospitals, but that of OAB (RR, 1.36; p<0.001; 95% CI, 1.196–1.553) was higher. The average prescription rate in geriatric hospitals was 0.4 times lower than in general hospitals. Urethral stricture, urolithiasis, hematuria, bed sore and renal failure were more prevalent in geriatric hospitals than in general hospitals (Fig. 3) however, overall complications were similar in geriatric hospitals and general hospitals (73.27% and 76.37%).
After the adoption of the FSMFD, the diagnostic rate and prescription rate increased in general hospitals but dropped in geriatric hospitals (Fig. 4). Especially prevalence of urologic disease in geriatric hospitals suddenly dropped after adoption of FSMFD on 2007 (Fig. 5). Before the adoption of the FSMFD, the diagnostic rate was 1.8 times higher in geriatric hospitals than general hospitals, but after the adoption of the FSMFD, they became similar. The prescription rate was 1.5 times higher in geriatric hospitals than general hospitals before 2007, but dropped to 0.3 times higher after the adoption of the FSMFD Complications decreased in geriatric hospitals (from 91.26% to 70.14%), while general hospital complications increased (from 66.62% to 78.09%).
In this population-based study we wish to know prevalence and management status in geriatric hospitals in South Korea. In all age groups, the prevalence of urologic disease and the complication rate were higher in geriatric hospitals than in general hospitals. After the adoption of the FSMFD, the prevalence of urologic disease and the complication rate dropped significantly in geriatric hospitals, but not in general hospitals. In the elderly group, the prevalence of urologic disease was higher (1.3 times) in geriatric hospitals than general hospitals, but the complication rate was not. After PSM analysis, the prevalence of urologic disease and complication rate were similar in both hospitals.
Urologic diseases are a well-known problem for the elderly, and the number of patients with neurogenic problems increases with age; therefore, the prevalence of urologic disease in geriatric hospitals should be higher than in the community population. According to a 1981 report from the United States [10], 69.3% of elderly patients admitted to geriatric long-term care hospitals presented with urinary dysfunction. In Korea, in an adult (18 years and older) population study [11], 61.4% of adults were found to suffer from urinary dysfunction, with the incidence increasing with age. The prevalence of BPH in the elderly population has been reported to be 40%–70% [1213] in western countries and 20%–40% in Korea [141516]. Incontinence is also common in the elderly and increases with age. The prevalence of incontinence was reported to be 43%–77% in United States nursing home patients [17] and 41.8% in Korean patients [18]. In our study, however, the prevalence of urologic disease was only 24.5%, which is significantly lower than in previous studies. Following subgroup analysis for the elderly and PSM, the prevalence of urologic disease was 26.5% and 23.0%, respectively. Moreover, the prevalence of OAB was only 2.9%, and even with neurogenic bladder included as an overlapping diagnosis, it only increased to 7.7%. Our study findings were more general than another study, which showed a prevalence of OAB ranging from 10.0% to 14.3% at age 40 and an increased incidence in the elderly [11]. These results also conflict with other studies that found a higher prevalence of neurogenic bladder and voiding disorders and higher rates of dementia and neuro-degenerative disorders among the inpatients of geriatric hospitals [1920]. This discrepancy in prevalence suggests that urologic diseases in geriatric hospitals are not properly diagnosed.
Compared with general hospitals, although there was a higher prevalence of urologic disease, urologic medication was prescribed less in geriatric hospitals. The diagnostic rate of OAB was 1.26 times higher in geriatric hospitals than general hospitals in the elderly group, yet the prescription rate of antimuscarinics was 0.61 times lower. From these results, we can suppose that factors other than clinical decision-making affect incontinence treatment. According to a 2009 field study of the Busan area [18], most patients with incontinence are not managed promptly and treatment is determined by cost and healthcare provider convenience. Moreover, the prescription rate of antimuscarinics was significantly lower after the adoption of the FSMFD; dropping from 4.86% to 0.89%. If there were not any sudden changes in inpatients characteristics within follow-up period, this result can assist that care for voiding dysfunction in inpatients actually worsened by economic issue. On the other hand, we cannot rule out there was over diagnosis and treatment before adoption of the FSMFD and decline was result of optimize management in geriatric hospital. For clear out this competing hypothesis, well designed study for effect of FSMFD in geriatric hospitals with changes in another disease treatment should be needed.
Urologic diseases are important in elderly patients QoL and lack of certified urologists in geriatric hospitals can be worsen management of urologic disease in geriatric hospitals. In previous study of our group [21], we found knowledge level is important in urinary incontinence management and over a half of healthcare providers agreed with needs in management by urologist. Currently, the number of urologist working in geriatric hospitals as of December 2013 was 38 (1.14%), which is only 1.6% (38 of 2,350) of the total number of urologist. This number is even lower than that of other specialists in fields not included in the 8 main specialist groups (internal medicine, general surgery, neurology, neuropsychiatry, rehabilitation medicine, family medicine, neurosurgery, and orthopedics); such as obstetrics and gynecology (4.5%, 245 of 5,425) and oriental medicine (6.8%, 1,244 of 18,199). Political support such as designated urologist in geriatric hospitals or regular consultation of urologist should be helpful for improve management of urologic disease in geriatric hospitals.
This study was a population-based analysis using established cohort of NHIS which based on medical insurance claims data. Thus, it has limitations in reflecting the actual situation in the field. We can only suggest a trend of diagnosis and management of urologic disease in geriatric hospitals, based on this study. Also, complications were assessed according to the sum of each complication incidence, so we cannot remove duplicate events for individual patients and this is another limitation of this study. Another study using non-medical insurance data needs to be completed for results that are based on more accurate data for prevalence and management status of urologic diseases in geriatric hospitals. And this study has some conflicting issues, such as management changes after the adoption of FSMFD. There are obvious changes after adoption of FSMFD in management patterns in urologic disease of geriatric hospitals from our study, however we cannot assure how it affect to patients. It is important to medical politics decision making, so another well designed study and follow-up studies are needed for clarifying this situation.
Urologic disease is common in the elderly and is associated with patient QoL. We founded some problems in diagnosis and management of urologic diseases from this investigation. Political support such as assigning more urologist in geriatric hospitals can be help to overcome these problems.
ACKNOWLEDGMENTS
This study was supported by the Foundation for Korean Urological Association in 2014 (FKUA-2014-001).
References
1. United Nations. World population aging 2015 [Internet]. New York: United Nations, Department of Economic and Social Affairs Population Division;2015. cited 2016 May 5. Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf.
2. Statistics Korea. Population projections for Korea: 2010-2016 (Based on the 2010 Census) [Internet]. Daejeon: Statistics Korea;c2017. cited 2015 Oct 12. Available from: http://kosis.kr/ups3/service/ch_file_down.jsp?PUBCODE=PJ&FILE_NAME=/ups3/upload/101/PJ/PJ2011.pdf&SEQ=15.
3. Korea Institute for Health and Social Affairs. 2014 Elderly reports [Internet]. Sejong: Korea Institute for Health and Social Affairs;c2017. cited 2017 May 1. Available from: http://repository.kihasa.re.kr:8080/handle/201002/13710.
4. Bo M, Fonte G, Pivaro F, Bonetto M, Comi C, Giorgis V, et al. Prevalence of and factors associated with prolonged length of stay in older hospitalized medical patients. Geriatr Gerontol Int. 2016; 16:314–321. PMID: 25752922.

5. Batista-Miranda JE, Molinuevo B, Pardo Y. Impact of lower urinary tract symptoms on quality of life using Functional Assessment Cancer Therapy scale. Urology. 2007; 69:285–288. PMID: 17320665.

6. Lawhorne LW, Ouslander JG, Parmelee PA, Resnick B, Calabrese B. Urinary incontinence: a neglected geriatric syndrome in nursing facilities. J Am Med Dir Assoc. 2008; 9:29–35. PMID: 18187110.

7. Robertson C, Link CL, Onel E, Mazzetta C, Keech M, Hobbs R, et al. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int. 2007; 99:347–354. PMID: 17313423.

8. Korea Statistical Information Service. Number of specialists [Internet]. Daejeon: Statistics Korea;c2017. cited 2016 May 5. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_HIRA4K&vw_cd=&list_id=&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K1&path=#.
9. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15. PMID: 26822938.

10. Jewett MA, Fernie GR, Holliday PJ, Pim ME. Urinary dysfunction in a geriatric long-term care population: prevalence and patterns. J Am Geriatr Soc. 1981; 29:211–214. PMID: 6785337.

11. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011; 29:185–190. PMID: 19898824.

12. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PMID: 6206240.

13. Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet. 1991; 338:469–471. PMID: 1714529.

14. Chung JS, Byun SS, Han BK, Jeong SJ, Hong SK, Lee SE. Changes in prostate-specific antigen levels and prostate volume in octogenarian men: community-based study. Urology. 2009; 73:1270–1273. PMID: 19371943.

15. Lee YJ, Jeong SJ, Byun SS, Lee JJ, Han JW, Kim KW. Prevalence and correlates of nocturia in community-dwelling older men: results from the korean longitudinal study on health and aging. Korean J Urol. 2012; 53:263–267. PMID: 22536470.

16. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998; 33:17–21. PMID: 9471036.

17. Offermans MP, Du Moulin MF, Hamers JP, Dassen T, Halfens RJ. Prevalence of urinary incontinence and associated risk factors in nursing home residents: a systematic review. Neurourol Urodyn. 2009; 28:288–294. PMID: 19191259.

18. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009; 50:450–456.

19. Lee SH, Kang JS, Kim JW, Lee SJ. Incontinence pad usage in medical welfare facilities in Korea. Int Neurourol J. 2013; 17:186–190. PMID: 24466466.

20. Lee SH, Cho ST, Na HR, Ko SB, Park MH. Urinary incontinence in patients with Alzheimer's disease: relationship between symptom status and urodynamic diagnoses. Int J Urol. 2014; 21:683–687. PMID: 24593278.

21. Jang Y, Kwon BE, Kim HS, Lee YJ, Lee S, Kim SJ, et al. Knowledge and practice behaviors regarding urinary incontinence among Korean healthcare providers in long-term care hospitals. Int Neurourol J. 2015; 19:259–264. PMID: 26739180.

SUPPLEMENTARY MATERIALS
Scan this QR code to see the supplementary Tables, or visithttp://icurology.org/src/sm/icu-58-281-s001.pdf.

Fig. 1
Comparison of the annual numbers of institutions (A) and bed count (B) between geriatric hospital and general hospital. Geriatric hospitals institution numbers exponentially increased (A) and bed counts were almost catch up by 2013 (B). Increasing velocity of geriatric hospital institutions and bed counts slowed down in 2008 to 2009 period, it was owing to changes in medical fee system of geriatric hospitals.
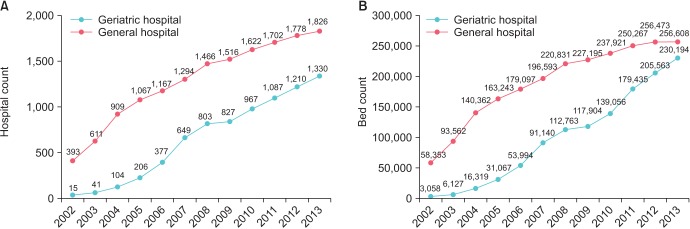
Fig. 2
Changes of management pattern in geriatric (A) and general hospitals (B) after adoption of the fixed sum medical fee per day (FSMFD) in all aged group. Prevalence, prescription rate and complication incidence were notably decreased in geriatric hospitals however prescription rate and complication incidence in general hospitals were increased.
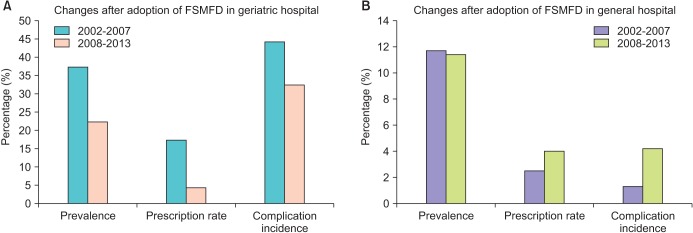
Fig. 3
Comparison of complication incidence in the propensity score matching group. Urolithiasis, hematuria, bed sore, and renal failure were common in geriatric hospitals but urinary tract infection and dermatitis were more prevalent in general hospitals.
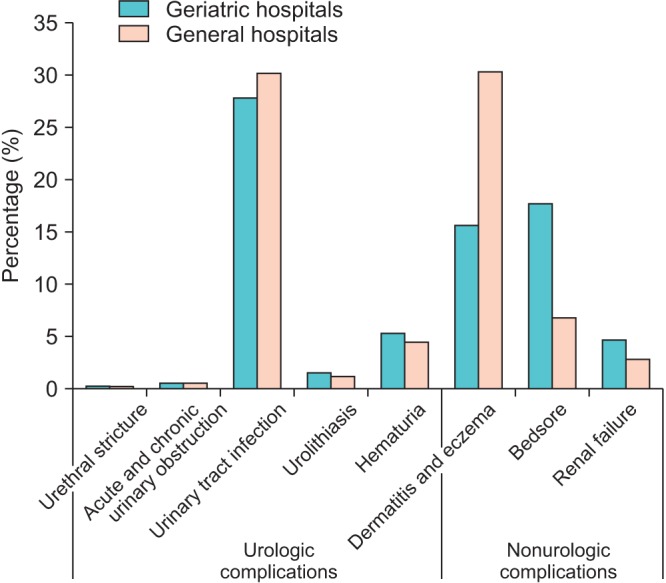
Fig. 4
Comparison of changes before and after adoption of fixed sum medical fee per day (FSMFD) in geriatric hospital (A) and general hospital (B) in propensity matching analysis. Changes in average prescription rate of geriatric hospitals after adoption of the FSMFD was dropped from 10.8% to 3.2 %.
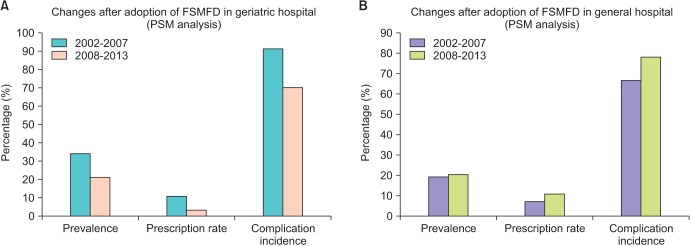
Fig. 5
Annual changes in urologic disease prevalence in propensity matching analysis. Urologic disease prevalence was significantly dropped in 2008–2009 year, when fixed sum medical fee per day was started.
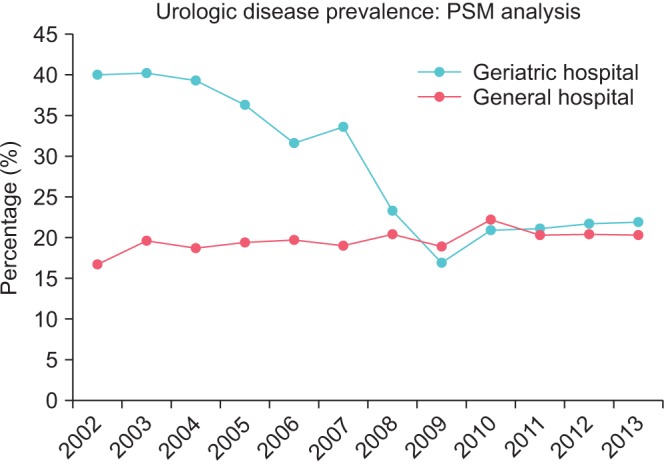
Table 1
Comparison of geriatric hospitals and general hospitals: before and after propensity score matching analysis




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download