Abstract
Purpose
To evaluate the diagnostic value of magnetic resonance imaging (MRI) in patients with suspected penile fracture.
Materials and Methods
A total of 122 patients admitted to our inpatient clinic with a suspicion of penile fracture following a recent history of penile trauma and who underwent surgical exploration were included this study. A thorough physical examination, a detailed medical history, description of the trauma, and preoperative International Index of Erectile Function (IIEF) scores were obtained for each patient prior to surgery. Thirty-eight of these patients were evaluated with MRI before the surgical exploration. Intraoperative findings were also recorded. Physical findings and IIEF scores were also recorded at postoperative 6 months.
Results
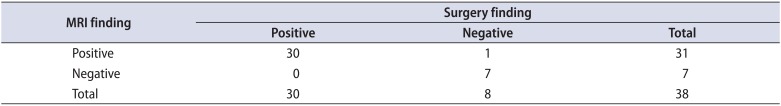
The mean age of our patient group was 36.5±12.3 years. Penile fracture was detected in 105 of 122 patients in whom surgical exploration was performed owing to a suspected diagnosis. The mean time interval from penile trauma to hospital admittance was 9.9±15.1 hours. No cavernosal defect was detected in 9 of 84 patients (10.7%) who were not evaluated with MRI prior to surgery. Compared with surgical exploration, MRI findings showed 100% (30 of 30) sensitivity and 87.5% (7 of 8) specificity in the diagnosis of penile fracture. MRI had a high negative predictive value of 100% (7 of 7) and a positive predictive value of 96.7% (30 of 31) with just 1 misdiagnosed patient.
Penile fracture is defined as a disruption of the tunica albuginea with a corporeal tear occurring after a blunt trauma directed to an erect penis. Fracture typically occurs when the penis comes out from the vagina and hits the pubic bone or perineum during sexual intercourse [1]. Well-known physical findings and patient history reveal the diagnosis in most cases, and additional imaging methods are usually not necessary. However, false penile fracture is also reported in patients who present with penile swelling, ecchymosis, and rapid detumescence after blunt penile trauma and report hearing a snap sound, which is typical of a penile fracture. In these circumstances, surgical exploration or additional imaging modalities can be considered [1]. As a differential diagnosis, rupture of the penile superficial dorsal vein can be treated conservatively [2]. Cavernosography or penile ultrasonography can help in diagnosis, but these methods are mainly operator-dependent and have high false-negative rates [1]. Magnetic resonance imaging (MRI) has much better soft tissue imaging quality and can show tunical tears noninvasively [2].
The aim of this study was to evaluate the diagnostic value of MRI in patients with suspected penile fracture.
Between January 2005 and July 2015, 122 male patients were admitted to our Emergency Department with a suspected penile fracture. All patients underwent a surgical exploration. Preoperatively, MRI had been done in 38 patients (study group) to locate the tunical tear. The remaining 84 patients were explored without preoperative MRI (control group). The study was approved by the Institutional Ethics Committee of our facility (date: 19/12/2013; number: 89513307/1009/232). All authors had full access to the data and take responsibility for the integrity of the data. All authors read and approved the manuscript as written.
Preoperative MRI was done in our radiology clinic with our clinical consultation service after admission to the emergency department. Magnetic resonance (MR) images were obtained at 1.5 MR Tesla units with the patient's penis laid and fixed on his abdomen dorsally. Coronal, axial, and sagittal images were obtained. Fracture was defined as hematoma with discontinuity of the low signal intensity in the tunica albuginea. Analyses of these images were done by the radiology clinic in our hospital.
Time from fracture to hospital admission, ecchymosis of the penis, palpation of the fracture line, presence of penile hematoma, urethrorrhagia, penile deviation, hearing of a snap sound, intraoperative findings such as incision type, presence of a cavernosal tear, and if present the location and length of the tear and additional urethral damage were recorded. Patients in whom preoperative MR images were obtained (n=38) were asked to complete the International Index of Erectile Function (IIEF) questionnaire preoperatively and at 6 months postoperatively. Postoperative physical examinations were also recorded at 6 months.
IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) was used for the statistical analysis. Statistical data were presented as means±standard deviations. Normal distributions of variables were analyzed with the one-sample Kolmogorov Smirnov Test. Comparisons between groups were carried out by using chi-square, Mann-Whitney U-test, and Student t-test with a p-value <0.05 considered statistically significant.
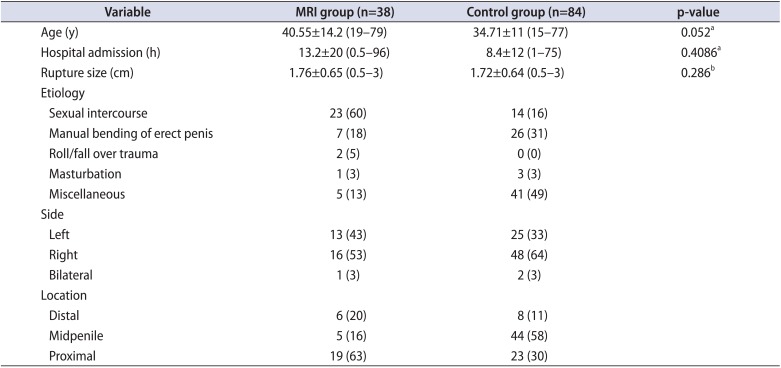
The etiologies of penile fracture cover a wide spectrum because of differences in patient-dependent history. Detailed history taking showed that 38% of 122 patients reported miscellaneous causes of fracture and 30% reported a fracture incident during sexual intercourse. A common cause of fracture in the Middle East, “manual bending of erect penis,” was the third most frequent cause in 27% of patients (Table 1).
Patient age, time to hospital admission after incidence, and penile rupture size were not statistically different between the MRI and the control groups (p=0.052, p=0.4086, and p=0.286, respectively).
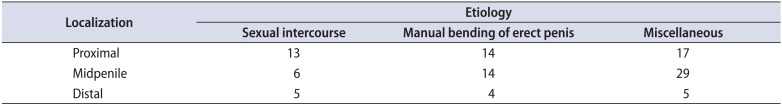
The most common causes of fracture were analyzed by chi-square test according to the location of the tunical tear. Evaluation of 122 patients showed that there was no statistically significant difference between fracture localization and cause (p=0.1365) (Table 2).
The postoperative physical findings of the 38 patients in the MRI group revealed normal postoperative changes. Mean preoperative and postoperative IIEF scores were 23.2±2.5 and 22.5±3.6, respectively (p=0.09). Five patients (13.2%) reported mild penile deviation of less than 30 degrees and not leading to difficulty with sexual intercourse. One patient (2.6%) also reported a hard nodule underneath the penile skin that was caused by the suture material.
Evaluation of the IIEF scores revealed that 7 of 38 patients (18.4%) had lower scores in the postoperative assessment. All of these 7 patients also had a score less than 25 in the preoperative setting. Time to hospital admission and rupture size did not significantly affect postoperative IIEF score (p=0.9655 and p=0.3831, respectively).
MRI findings revealed penile fracture in 31 of 38 patients. Only 1 of the 31 patients had no tunical tear in surgical exploration. In all 7 patients who were diagnosed as having no tunical rupture by MRI, the diagnosis was confirmed by surgical exploration. However, 11% (9 of 84) of the patients in the control group were not found to have a penile rupture in surgical exploration (Table 3, Fig. 1).
Compared with surgical exploration, the MRI findings showed 100% sensitivity and 87.5% specificity in the diagnosis of penile fracture. MRI had a high negative predictive value of 100% and a positive predictive value of 96.7% with just 1 misdiagnosed patient.
In surgical exploration with the help of MRI findings, fracture localization was determined and a lateral incision was made above the fracture line in 5 patients, a penoscrotal incision was made in 8 patients, and a circumferential degloving incision was made in 25 patients to access the fracture site.
Penile fracture occurs with expansion of the corpus cavernosum and thinning of the tunica albuginea. As a result, it leads to an albuginea that is more vulnerable to external trauma [3]. Penile fracture is an emergency that needs surgical intervention. Clinical history and physical findings may not be adequate to diagnose this situation; there are several reports of other pathologies that mimic penile fracture. It can be difficult for many urologists to make an appropriate diagnosis because the physical and history findings may differ in each patient. Surgical exploration remains a safe and reliable option in all cases, but preoperative imaging techniques can help to make a diagnosis and avoid unnecessary surgical explorations.
The etiology of penile fracture can differ geographically. In Western countries, sexual intercourse has been reported as the most common cause [4]. Zargooshi [5] reported a 352 patient series from Iran in which manual bending of the erect penis was found to be the most common cause in 76% of patients. In our study, we found results comparable with those in the literature, with sexual intercourse (30%) and manual bending of the erect penis (27%) as common causes. However, we had to define a majority (37%) of etiologies as “miscellaneous” because the patients' reports about the cause varied widely.
Asgari et al. [6] reported penile curvature and painful sexual intercourse in patients who were surgically treated 48 hours after the incident. Another study with 3 patients reported that erection was normal and straight after surgical correction that was delayed by 24 to 40 hours [7]. El-Assmy et al. [8] reported no difference in late complications with 113 months of follow-up between 31 patients who underwent surgical treatment after admission more than 24 hours (mean, 44 hours) after the incident and patients who were admitted early. A recent study revealed mild erectile dysfunction or penile curvature in 29 patients with a mean admission time after incidence of 5.5 hours [9]. In our study, we also found no significant effect on postoperative erectile function of late admission to the hospital. IIEF scores remained the same in 9 patients who were admitted 12 to 96 hours after incidence; 1 patient developed lower urinary tract symptoms.
In the largest study ever with 352 patients, Zargooshi [5] reported that the most common location of ruptures caused by manual bending of the erect penis (taghaandan practice) in Iran is proximal. We found no statistically significant difference between fracture etiology and tear location in 122 patients.
Surgical degloving of the penis with a circumferential incision is the most used technique for exploring the corpora cavernosum and penile urethra. However, this technique can cause additional morbidity by diffuse swelling of the Dartos fascia [3]. Penoscrotal incision can be an adequate approach, whereas nearly two-thirds of fractures are located proximally [10,11]. We chose the incision technique in 41% of our patients (13 of 31) according to the tear location seen on MRI, and adequate exploration was accomplished.
Diagnosis of penile fracture mainly depends on clinical history and physical examination findings, but there are also helpful diagnostic tools such as cavernosography, urethrography, ultrasonography, and MRI. Cavernosography and urethrography are easy to perform but are invasive, and complications such as priapism, allergic reaction, infection, and contrast medium allergy have been reported [4,9]. A little thrombus can occlude a small tunical tear and this can cause false-negative results in cavernosography [12]. Urethrography has also limitations and may not detect an urethral tear in every case [4].
Ultrasound is a very useful technique in the diagnosis of penile fracture. Several studies have reported this modality to be a safe, fast, and low-cost technique [13,14]. Lee et al. [15] reported a series of 32 patients who underwent ultrasound before surgery confirmed tunical rupture. For tunical rupture with small tears, however, evaluation may be difficult with sonography. The thrombus may close the defect and ultrasound may not differentiate the normal tunica albuginea from the defect area [16].
MRI can be used in the diagnosis of penile fracture because it can show tissue intensity perfectly and can provide multiplanar images [17]. It also has some limitations, however, such as cost and availability in every center. MRI is especially useful for showing unity of the tunical albuginea, the length of a tunical tear, and the location and presence of a tear in cases in which ultrasound may not provide adequate information [18]. Additionally, MRI can show adjacent tissue damage such as to the urethra and corpus spongiosum and can help in differential diagnosis of penile fracture [2]. Guler et al. [19] reported the high diagnostic value of MRI in penile fracture in a recent study with 15 patients. However, that study did not include a control group and could not actually define the diagnostic accuracy of MRI. In our study, there were no statistically significant differences in age, hospital admission time, or rupture size between the groups. Thus, we assumed homogeneity between these groups of patients. The 100% sensitivity of MRI was calculated in 38 patients who underwent MRI before surgical exploration. Just 1 patient was misdiagnosed. An unnecessary exploration rate of 11% in our control group confirmed that MRI can be an appropriate method to define the exact diagnosis of penile fracture in centers where MRI is available.
The limitations of this study were that we did not have IIEF scores for all 122 patients. Also, before surgical exploration we could not perform penile ultrasonography in all patients to make a more definite statement about the diagnostic power of MRI in these cases.
MRI can be used to diagnose penile fracture and to determine a surgical approach. We suggest that with the help of this modality, urologists can decrease the number of unnecessary surgical explorations and decrease both early and late postoperative complications by choosing an adequate surgical approach. In emergency situations, MRI may not be available in every center, but it can be helpful for diagnosis in centers where it is easily accessible.
References
1. Morey AF, Dugi DD. Genital and lower urinary tract trauma. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 2379–2392.
2. Koifman L, Barros R, Júnior RA, Cavalcanti AG, Favorito LA. Penile fracture: diagnosis, treatment and outcomes of 150 patients. Urology. 2010; 76:1488–1492. PMID: 20708223.

3. Antonini G, Vicini P, Sansalone S, Garaffa G, Vitarelli A, De Berardinis E, et al. Penile fracture: penoscrotal approach with degloving of penis after Magnetic Resonance Imaging (MRI). Arch Ital Urol Androl. 2014; 86:39–40. PMID: 24704930.

5. Zargooshi J. Sexual function and tunica albuginea wound healing following penile fracture: an 18-year follow-up study of 352 patients from Kermanshah, Iran. J Sex Med. 2009; 6:1141–1150. PMID: 19138357.

6. Asgari MA, Hosseini SY, Safarinejad MR, Samadzadeh B, Bardideh AR. Penile fractures: evaluation, therapeutic approaches and long-term results. J Urol. 1996; 155:148–149. PMID: 7490817.

7. Cummings JM, Parra RO, Boullier JA. Delayed repair of penile fracture. J Trauma. 1998; 45:153–154. PMID: 9680030.

8. el-Assmy A, el-Tholoth HS, Mohsen T, Ibrahiem el-HI. Does timing of presentation of penile fracture affect outcome of surgical intervention? Urology. 2011; 77:1388–1391. PMID: 21440289.

9. Swanson DE, Polackwich AS, Helfand BT, Masson P, Hwong J, Dugi DD 3rd, et al. Penile fracture: outcomes of early surgical intervention. Urology. 2014; 84:1117–1121. PMID: 25443914.

10. Ozcan S, Akpinar E. Diagnosis of penile fracture in primary care: a case report. Cases J. 2009; 2:8065. PMID: 19830047.

11. Srinivas BV, Vasan SS, Mohammed S. A case of penile fracture at the crura of the penis without urethral involvement: rare entity. Indian J Urol. 2012; 28:335–337. PMID: 23204666.

12. Dever DP, Saraf PG, Catanese RP, Feinstein MJ, Davis RS. Penile fracture: operative management and cavernosography. Urology. 1983; 22:394–396. PMID: 6636395.

13. Kachewar S, Kulkarni D. Ultrasound evaluation of penile fractures. Biomed Imaging Interv J. 2011; 7:e27. PMID: 22279504.
14. Mazaris EM, Livadas K, Chalikopoulos D, Bisas A, Deliveliotis C, Skolarikos A. Penile fractures: immediate surgical approach with a midline ventral incision. BJU Int. 2009; 104:520–523. PMID: 19239439.

15. Lee SH, Bak CW, Choi MH, Lee HS, Lee MS, Yoon SJ. Trauma to male genital organs: a 10-year review of 156 patients, including 118 treated by surgery. BJU Int. 2008; 101:211–215. PMID: 17922859.

16. Koga S, Saito Y, Arakaki Y, Nakamura N, Matsuoka M, Saita H, et al. Sonography in fracture of the penis. Br J Urol. 1993; 72:228–229. PMID: 8402028.

17. Yokogi H, Mizutami M, Ishibe T. Magnetic resonance imaging of a penile fracture. Acta Urol Belg. 1992; 60:93–95. PMID: 1414726.
19. Guler I, Ödev K, Kalkan H, Simsek C, Keskin S, Kilinç M. The value of magnetic resonance imaging in the diagnosis of penile fracture. Int Braz J Urol. 2015; 41:325–328. PMID: 26005975.

Fig. 1
Magnetic resonance images showing penile rupture. (A) Coronal plane image of a proximal corporal rupture (arrow). (B) Axial plane image of a midpenile corporal rupture (arrow).
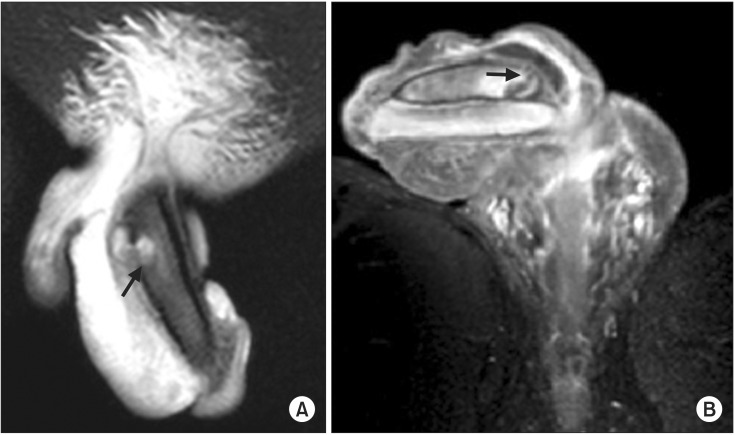
Table 1
Demographics and findings in the magnetic resonance imaging (MRI) and control groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download