Abstract
Purpose
According to the aging of society and the spread of antibiotic-resistant strains, it is worth considering the different aspects of epididymitis (EP) in older and younger patients, even though the etiology and therapeutic strategies of this disease are considered to be established. Thus, we investigated how age affects EP-related symptoms.
Materials and Methods
Data were gathered from 7 hospitals in Hyogo, Japan, and the correlations of age (older or younger) with urine findings such as pyuria or bacteriuria and EP-related symptoms such as fever were investigated.
Results
In all 308 cases with full data for evaluation, there were 66 febrile (38℃ or higher) cases (21.4%) and bacteriuria was seen in 158 cases (51.3%). In the multivariate analysis, older age (65 years or older) was significantly correlated with the presence of pyuria (p=0.0156). Regarding the relationship between urine findings and EP-related symptoms, pyuria was significantly related to fever (37℃ or higher; p=0.0159).
The recent aging of society and, importantly, the spread of antibiotic-resistant strains, makes it worthwhile to consider the different aspects of epididymitis (EP) in older and younger patients, even though the etiology and therapeutic strategies of this disease are considered to be established. Thus, we investigated how age (older or younger) affects EP-related symptoms. EP may have different characteristics in older and younger patients, especially in terms of causative microorganisms and severity; however, research has focused mostly on younger men in the United States [1]. It has been debated whether EP is related to urinary tract infections (UTIs) [2345], and the theory suggests that the cause of EP in younger men tends to be sexually transmitted infections (STIs) and that the cause in older men tends to be UTIs. This may be partly because the causative routes of infection are varied, and some routes involve the urinary tract and others involve urogenital organs such as the prostate or seminal vesicle [6].
EP presents with a variety of clinical features or symptoms; for instance, the infection occurrence pattern can be acute or chronic, and the patients may or may not have fever [5]. Differences in the extent of inflammation may help to explain differences in presenting symptoms [7]. Considering that older patients have lower urinary tract symptoms (LUTS) from benign prostatic hyperplasia (BPH) [8], urinary tract factors may affect this infectious disease; for instance, pyuria, bacteriuria, or large volumes of residual urine might be risk factors for EP from UTI.
In this study, we retrospectively examined 308 cases from seven hospitals in Hyogo, Japan, to explore the clinical risk factors for EP-related symptoms, with a particular focus on the patients' age or urine findings of pyuria or bacteriuria. These findings could provide the basis for prospective or randomized studies to establish the clinical risk factors for EP-related symptoms or algorithms for treatments in the future.
The EP data were gathered from seven hospitals (Kobe University Hospital, Yodogawa Catholic Hospital, Steel Memorial Hirohata Hospital, Shinko Hospital, Kobe City Medical Center West Hospital, Kobe Red Cross Hospital, and Hara Genitourinary Hospital) in Hyogo, Japan. Data were analyzed retrospectively. This study was admitted by the Kobe University Institutional Review Board and followed the basis of the Declaration of Helsinki (approval number: 160148). EP was diagnosed by the physicians taking care of the patients as induration and tenderness of the epididymis. All patients were diagnosed and treated between April 2007 and July 2012.
All data included the following factors: age, febrile or afebrile, duration to improvement of fever, site, tenderness, pyuria, bacteriuria, and antibiotic treatments. The symptoms investigated were those at the time of diagnosis. In addition, pyuria and bacteriuria were also investigated if they might have caused EP-related symptoms. Pyuria was defined as 5 or more white blood cells per high power field in urine and bacteriuria as a bacterial isolation of 105 or more colony forming units/mL in urine. Bacteriuria was diagnosed by simple urine analysis.
Statistical analysis was conducted by using chi-square tests with JSTAT (Java Virtual Machine Statistics Monitoring Tool). To examine whether older age (≥65 years) correlated with urine findings or EP-related symptoms in EP patients, we divided the patients into 2 groups by age, 65 years or older and 64 years or younger, and performed statistical analyses on the categories mentioned above. This is because 65 years is regarded as older age in this country. In addition, statistical analyses were conducted to examine whether pyuria or bacteriuria correlated to EP-related symptoms with p<0.05 considered to indicate statistical significance. These analyses were performed by use of univariate and multivariate analyses, and multiple regression analysis was performed by use of the PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
In all cases in which data were available for analysis, age ranged from 5 to 98 years. The site of EP included 150 right cases, 152 left cases, and 4 bilateral cases (2 unknown cases). Sixty-six cases (21.4%) had high fever (≥38℃) and the mean duration to fever suppression was 3.35±1.83 days. Pyuria was seen in 147 of 308 cases (47.7%) and bacteriuria was seen in 152 of 308 cases (49.4%). Causative microorganisms were Escherichia coli and Chlamydia in 8 cases each (2.6%), respectively. As to other antibiotic-resistant strains, there were 2 cases each of extended spectrum beta-lactamase-producing E. coli and methicillin-resistant Staphylococcus aureus (0.65%), respectively (Tables 1, 2).
All cases improved after treatment but 2 cases underwent orchiectomy for abscess formation. As therapeutic antibiotics, levofloxacin (133 patients [43.2%]), cefozopran (73 patients [23.7%]), and ceftriaxone (43 patients [14.0%]) were used frequently. One hundred fifty-one patients (49.0%) were treated with 1 kind of antibiotic and 139 (45.1%) were treated with 2 kinds, but mostly they were used as a switching therapy.
To determine if age correlated with urine findings such as pyuria or bacteriuria or EP-related symptoms such as scrotum swelling or fever, we set 65 years as the cutoff as mentioned above and then compared symptoms between the older age group (≥65 years) and the younger age group (≤64 years). We found that pyuria (p=0.0027) and bacteriuria (p=0.033) were observed at a significantly higher ratio in the older age group than in the younger age group. However, there was no significant correlation between age and duration of fever (p=0.057). In the multivariate analysis, older age groups correlated with pyuria (p=0.0156) (Table 3).
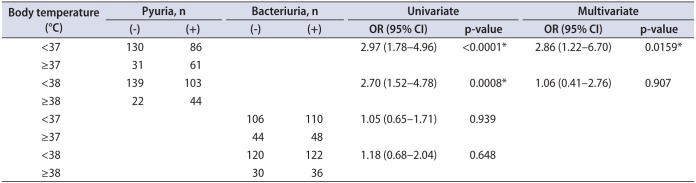
Pyuria was significantly related to fever (p<0.0001 for 37℃ or higher and p=0.0008 for 38℃ or higher), and this was observed as significant in the multivariate analyses as well (p=0.0159 for 37℃ or higher) (Table 4).
The notable features of EP are as follows: (1) Identification of the route of infection is sometimes unclear. (2) The causative microorganisms are often undetectable. (3) EP is comparatively easy to diagnose. (4) As mentioned below in the study limitations, it may be hard to test urine or pus cultures because patients with EP, like patients with male urethritis, tend to be cured in clinics and not in research institutions such as a university hospital. Therefore, there are fewer cases with treatment difficulties compared with other urological infections and thus research is lacking. Accordingly, we focused on the correlation between the patient's age and urine findings related to inflammation or infection, and EP-related symptoms such as fever in order to further knowledge of EP and its etiology.
Several reports have described the guidelines for the management of EP. Street et al. [9] stated that in their management of epididymo-orchitis they consider mumps and, especially in the immune-compromised host, tuberculosis as possible causative microorganisms and that consideration of gonorrhea is essential for decisions about antibiotics. As to the antibiotic treatments, our cases included a high frequency of fluoroquinolone use according to the literature [10], followed by the third- or fourth-generation cephalosporins. These differences in antibiotic use suggest that (1) our cases included older patients at higher ratios than in other studies and that Enterobacteriaceae, which is not an STI-causing microorganism in general, should have been a target for treatment, and (2) regional guidelines may be necessary because not all regions will have the same trends in patients' age and causative microorganisms [11].
In terms of causative microorganisms, Bébéar et al. [12] stated in their review that asymptomatic chlamydia infection can cause symptomatic EP and that single-dose antibiotic treatments should be effective in uncomplicated cases. On the other hand, E. coli was most often isolated as the causative microorganism in our limited data (because only 41 cases had positive urine or pus culture tests as mentioned below in the study limitations), which differs from other reports in which Neisseria gonorrhoeae or Chlamydia spp. were the most prevalent [1314]. EP may be caused by symptomatic or asymptomatic UTIs, at least based on our data and especially in the older generation.
A report from Korea showed that epididymo-orchitis was more common in patients not only with a history of urethral stricture but on clean intermittent catheterization (CIC) rather than indwelling urethral catheterization. Those authors also added that CIC, not urethral stricture, is a significant independent risk factor for epididymo-orchitis [15]. Our data showed that pyuria correlated with fever (p=0.0159). In contrast to younger men, in whom sexually transmitted pathogens are predominant, in older patients with a history of subvesical obstruction, E. coli is the most frequent pathogen responsible [16]. These data support our data mentioned above and overcome the limited evidence for not only etiology but also treatments, especially in older patients.
We would like to emphasize the limitations of this study. First, the data were retrospectively gathered from seven hospitals over 5 years and lack some elements necessary for definitive statistical analyses. However, we designed the study to include and reflect real clinical EP and its treatments. In particular, bacterial studies were not always available, suggesting that physicians need to be educated on the need for culture tests when treating with antibiotics [17]. Garthwaite et al. [18] discussed the lower implementation rate of the European Urological Association guideline in the management of acute epididymo-architis. However, the references cited in that paper are older and considering the dramatic changes in society, especially in aging and antibiotic-resistant microorganisms, information on this disease needs to be updated by this kind of research. Finally, our data on LUTS were available in only a limited population. These limitations should be overcome by the establishment of therapeutic strategies not only for antibiotic therapies but also for treatment goals and the management of risk factors such as uncontrolled LUTS from BPH including pyuria or bacteriuria.
Our retrospective data showed that older patients (≥65 years) had a higher ratio of pyuria, and in the multivariate analysis, pyuria may have been significantly correlated with EP-related symptoms (fever) in this study of over 300 cases of EP. These data suggest that age-specific guidelines may be necessary, and for this, additional clinical trials should be considered.
ACKNOWLEDGMENTS
We thank Drs. Minoru Hazama, Akira Fujii, Hiroshi Maeda, Masuo Yamashita, Ichiro Nakamura, Takashi Matsui, and Shoji Hara for data gathering and taking care of patients.
References
1. Mittemeyer BT, Lennox KW, Borski AA. Epididymitis: a review of 610 cases. J Urol. 1966; 95:390–392. PMID: 5906006.

2. Ludwig M, Kümmel C, Schroeder-Printzen I, Ringert RH, Weidner W. Evaluation of seminal plasma parameters in patients with chronic prostatitis or leukocytospermia. Andrologia. 1998; 30(Suppl 1):41–47. PMID: 9629442.

3. Horner PJ. European Branch of the International Union against Sexually Transmitted Infection and the European Office of the World Health Organization. European guideline for the management of epididymo-orchitis and syndromic management of acute scrotal swelling. Int J STD AIDS. 2001; 12(Suppl 3):88–93. PMID: 11589805.

4. Grabe M, Bjerklund-Johansen TE, Botto H, Çek M, Naber KG, Tenke P, et al. Guidelines on urological infections. Anheim (Netherlands): European Association of Urology;c2010. p. 79–81. Epididymitis and Orchitis.
5. Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009; 79:583–587. PMID: 19378875.
6. La Vignera S, Calogero AE, Arancio A, Castiglione R, De Grande G, Vicari E. Transrectal ultrasonography in infertile patients with persistently elevated bacteriospermia. Asian J Androl. 2008; 10:731–740. PMID: 18645676.

7. Marconi M, Pilatz A, Wagenlehner F, Diemer T, Weidner W. Are antisperm antibodies really associated with proven chronic inflammatory and infectious diseases of the male reproductive tract? Eur Urol. 2009; 56:708–715. PMID: 18715698.

8. Kirby R. Improving lower urinary tract symptoms in BPH. Practitioner. 2011; 255:15–19, 2.
9. Street E, Joyce A, Wilson J. Clinical Effectiveness Group, British Association for Sexual Health and HIV. BASHH UK guideline for the management of epididymo-orchitis, 2010. Int J STD AIDS. 2011; 22:361–365. PMID: 21729951.

10. Ludwig M. Diagnosis and therapy of acute prostatitis, epididymitis and orchitis. Andrologia. 2008; 40:76–80. PMID: 18336454.

11. Shigemura K, Okada H, Shirakawa T, Tanaka K, Arakawa S, Kinoshita S, et al. Susceptibilities of Neisseria gonorrhoeae to fluoroquinolones and other antimicrobial agents in Hyogo and Osaka, Japan. Sex Transm Infect. 2004; 80:105–107. PMID: 15054169.

12. Bébéar C, de Barbeyrac B. Genital Chlamydia trachomatis infections. Clin Microbiol Infect. 2009; 15:4–10.

13. De Jong Z, Pontonnier F, Plante P, Gautier JR, Ioualalen A, Archambaud M, et al. The frequency of Chlamydia trachomatis in acute epididymitis. Br J Urol. 1988; 62:76–78. PMID: 3408874.
14. Eley A, Oxley KM, Spencer RC, Kinghorn GR, Ben-Ahmeida ET, Potter CW. Detection of Chlamydia trachomatis by the polymerase chain reaction in young patients with acute epididymitis. Eur J Clin Microbiol Infect Dis. 1992; 11:620–623. PMID: 1396770.
15. Ku JH, Jung TY, Lee JK, Park WH, Shim HB. Influence of bladder management on epididymo-orchitis in patients with spinal cord injury: clean intermittent catheterization is a risk factor for epididymo-orchitis. Spinal Cord. 2006; 44:165–169. PMID: 16151451.

16. Melekos MD, Asbach HW. Epididymitis: aspects concerning etiology and treatment. J Urol. 1987; 138:83–86. PMID: 3474421.

17. Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011; 52:e56–e93. PMID: 21258094.

18. Garthwaite MA, Johnson G, Lloyd S, Eardley I. The implementation of European Association of Urology guidelines in the management of acute epididymo-orchitis. Ann R Coll Surg Engl. 2007; 89:799–803. PMID: 17999824.

Table 1
Patients' characteristics
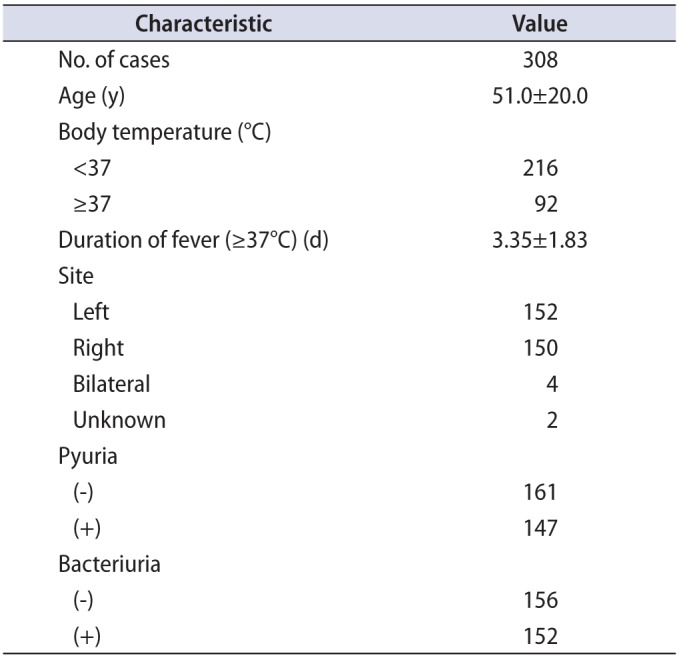
Table 2
Causative microorganism and antibiotic treatments
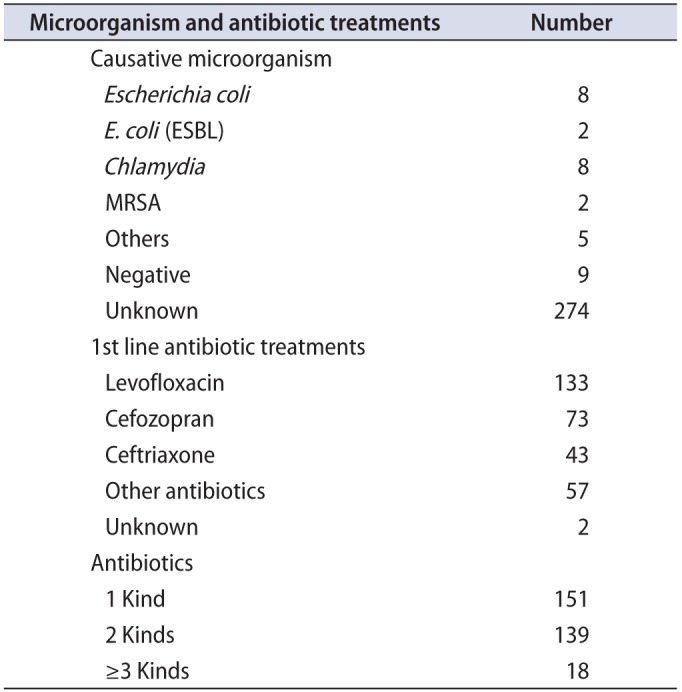
Table 3
Comparison between age and epididymitis-related symptoms
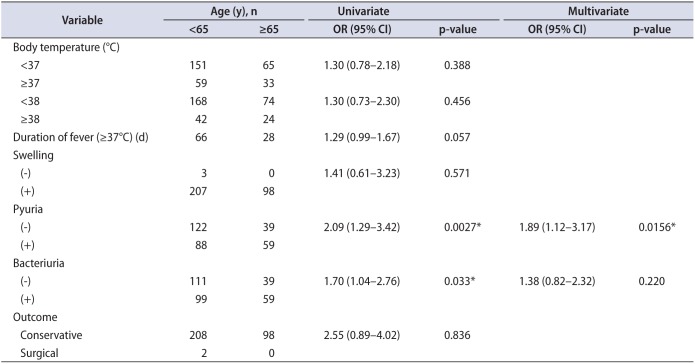
Table 4
Comparison between body temperature and urine findings




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download