Abstract
Purpose
To analyze postoperative outcomes of prostate surgery, resected specimen weight is commonly used. The difference between the preoperative calculated transitional zone volume and actual enucleated specimen weight following holmium laser enucleation of the prostate (HoLEP) is reported at over 20%. The reason for this difference is unclear. We assessed the association of volume of the prostatic adenoma with enucleated weight, the volume and calculated volume of the adenoma by pre- and postoperative ultrasonographic measurement.
Materials and Methods
All patients were prospectively enrolled who underwent HoLEP by two surgeons (SJO and JKO) between 2010 and 2015. Preoperative and postoperative prostate ultrasonography examinations were performed by a single examiner (JKO) during surgery, and weight and volume of the enucleated adenoma were measured. We compared preoperative adenoma size with postoperative weight and volume of the enucleated adenoma, calculated enucleated volume using ultrasonography, and calculated the correlation coefficients between preoperative adenoma volume and postoperative parameters.
Results
One hundred forty-two patients with a mean age (±standard deviation) of 69.8 (±8.8) years were analyzed. The mean preoperative ultrasound-measured adenoma volume was 31.7 (±21.4) mL, while postoperatively the mean retrieved weight of the adenoma was 22.3 (±17.0) g and the mean volume was 22.3 (±16.8) mL. Postoperatively calculated enucleated volume using ultrasonography was most strongly correlated with preoperative adenoma size (Pearson correlation coefficient 0.965, p<0.01).
Lower urinary tract symptoms (LUTS) are common in older men [1]. Though the guidelines of the American Urological Association suggest transurethral resection of the prostate (TURP) as the standard surgical treatment for benign prostate hyperplasia (BPH) [2], recent studies introduce holmium laser enucleation of the prostate (HoLEP) as the “new gold standard” surgical management [345]. Some studies report that HoLEP is preferable due to less blood loss and shorter hospital stay than TURP [6].
HoLEP consists of 2 steps—enucleation and morcellation [7]. Theoretically, adenoma tissue will be lost during laser enucleation and morcellation, as much as 20% loss of the enucleated adenoma during HoLEP. However, there is no evidence quantifying the postoperative specimen loss of enucleated adenoma in spite of frequent quotation in various studies.
Most studies report surgical outcomes using specimen weight, and none have assessed volume of the enucleated specimen. However, it seems important to measure the volume of enucleated adenoma, not only because the density of prostate tissue is different for each prostate, but because preoperative ultrasonographic data means volume of adenoma.
Accordingly, our study was designed to assess the difference between preoperatively estimated adenoma size and postoperatively remnant specimen, and assess the strength of association of preoperative volume of the prostatic adenoma with enucleated weight, the volume and calculated volume of the adenoma by pre- and postoperative transrectal ultrasonography (TRUS).
Our study was a prospective, multicenter study and was approved by the Institutional Review Board of Seoul National University Hospital (Seoul, South Korea) (approval number: H-1008-136-330) and Gachon University Gil Medical Center (Incheon, South Korea) (approval number: GAIRB2013-82). We prospectively collected data from consecutive patients who underwent HoLEP for management of symptomatic LUTS/BPH between 2010 and 2015. All operations were performed using a holmium: yttrium-aluminum-garnet laser by two surgeons (SJO and JKO). The holmium laser apparatus used in our study were OmniPulse (Trimedyne Inc., Irvine, CA, USA) and VersaPulse PowerSuite (Lumenis, Yokneam, Israel) [8].
The enucleated adenoma tissue was immediately weighed and tissue volume measured after retrieval in the operation room. To estimate volume of the enucleated adenoma, Archimedes' principle was used. An initial 100 mL of normal saline was poured into a 200-mL measuring cylinder. A specimen of enucleated adenoma was put into the cylinder. The increased volume in the measuring cylinder was measured by single examiner (JKO) and recorded as the volume of the enucleated specimen.
The method of estimation of prostate volume was the ellipsoid method previously introduced [9]. The calculated enucleated adenoma volume was estimated by the formula: calculated enucleated adenoma volume = preoperative prostate volume – (postoperative prostate volume – defect volume). The defect volume was determined using the same prostate volume calculation with ellipsoid method (Fig. 1) [10].
To compare the difference between preoperative transitional zone volume and postoperative enucleated adenoma, difference ratio was calculated as follows. Difference ratio with transitional zone volume (%) = (transitional zone volume – weight or volume of enucleated prostate)/transitional zone volume.
To compare the difference between calculated enucleated volume and postoperative enucleated adenoma, difference ratio was calculated as follows. Difference ratio with calculated enucleated volume (%) = (calculated enucleated volume – weight or volume of enucleated prostate)/calculated enucleated volume.
A descriptive analysis of age, weight and volume of postoperative specimen, ultrasonographic parameters including prostate volume, transitional zone volume, postoperative residual prostate volume, calculated enucleated adenoma volume was performed. To assess the association with preoperative adenoma volume, a multiple linear regression model was used with transitional zone volume as the outcome variable and other postoperative parameters introduced as independent variables. Null hypotheses of no difference were rejected if p-values were less than 0.05. All statistical analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC, USA).
One hundred forty-two patients with a mean age (±standard deviation) of 69.8 (±8.8) years were analyzed. The preoperative mean total prostate volume was 60.8 (±27.0) mL and transitional zone volume were 31.7 (±21.4) mL. The mean postoperative residual volume was 31.6 (±10.7) mL, and the calculated enucleated adenoma volume was 29.2 (±20.1) mL. The postoperative parameters of the adenoma specimen are weight, 22.3 (±17.0) g, and volume, 22.3 (±16.8) mL. The difference ratio between preoperative transitional zone volume and the postoperative adenoma was 31.7% for weight and 31.3% for volume. And the difference ratio between postoperatively calculated volume of enucleated adenoma and both of weight and volume of postoperative adenoma were 26.1%. The ratio between weight and volume of enucleated adenoma was 1.0 (±0.2) g/mL (Table 1).
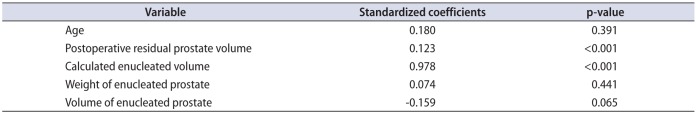
The postoperative calculated enucleated volume is strongly associated with preoperative transitional zone volume by multivariate analysis (p<0.001) (Table 2).
HoLEP is one of the best surgical treatment options to manage symptomatic BPH. Current research describes the advantages of HoLEP comparing other surgical manipulations in the aspects of preservation of erectile function, operability of concomitant anticoagulation, and acontractile detrusor function [6111213].
The exclamation, ‘Eureka!’ is from a famous anecdote regarding the ancient Greek physicist, Archimedes. To our knowledge, no study has reported the density of prostate tissue. The first aim of our study was to compare prostatic volume with weight. To investigate these parameters, Archimedes' principle was applied to assess the volume of enucleated tissue using a 200-mL measuring cylinder. We observed a ratio between weight and volume of specimen of 1.0±0.2 (g/mL). These findings are highly suggestive, not only that the mean prostatic density was about 1.0 g/mL in our study, but also that there is no difference in presenting either weight or volume of specimen to report surgical outcomes.
In our results, there was a 26% difference between the calculated enucleated volume and postoperative weight of specimen. Inversely, the calculated enucleated volume using TRUS was 30% more than postoperative weight of enucleated adenoma. There was a significant relationship between preoperative transitional zone volume and postoperative calculated enucleated volume in a multiple linear regression model.
To the best of our knowledge, this is the first study to prove the presence of difference between preoperative adenoma volume planned to remove and postoperative enucleated adenoma volume in HoLEP. Some possible reasons are suggested below. First, small morcellated adenoma tissue cannot be collected easily. In general, enucleated tissue is strained through a sieve using gauze in operation room. Different from a TURP specimen, the size of enucleated adenoma varies according to the morcellator. Furthermore, some tiny morcellated adenoma can freely penetrate holes of a sieve. Therefore, loss of some morcellated adenoma is unavoidable during tissue collection.
Second, some tissue will be vaporized during HoLEP. Though the main procedure of HoLEP is enucleation of prostatic adenoma along the adenoma plane, vaporization of some tissue is inevitable using the holmium laser. As a result, loss of tissue related to vaporization also occurs during surgery. Third, theoretically tissue volume may decrease due to loss of blood supply after enucleation. According to our above results, it is reasonable to assume that true volume of enucleated adenoma is above 30% more than the weight of the postoperative specimen in HoLEP.
In the analysis of the relationship between preoperative transitional zone volume and postoperative variables, calculated enucleated volume showed statistically strong association with preoperative transitional zone volume (p<0.001). This result may have clinical significance for the need to assess the true amount of enucleated adenoma. This kind of ultrasonographic assessment with defect volume may be useful to examine further follow-up TRUS of the patients who underwent HoLEP.
However, immediately postoperative ultrasonography is not always feasible in clinical practice not only because of bleeding control, but because of the necessity of additional preparation of ultrasonographic device in operation room. Therefore, an additional 30% more weight of postoperative specimen should be considered when the surgical outcome is compared between HoLEP and other surgery of BPH. Otherwise, immediately postoperative TRUS is recommended more than weight of postoperative specimen for obtaining the true volume of enucleated adenoma in case of considering comparative study about BPH surgeries. Our next study will focus on the change of prostate size after surgery and long-term observation results of HoLEP.
In our study, there was a significant difference between preoperative transitional zone volume and postoperative weight of enucleated adenoma during HoLEP. To assess more accurate volume of enucleated adenoma in HoLEP in case of comparing specimen weight with those of other BPH surgery, it is highly recommended to consider 1.3 times of postoperative weight or volume of enucleated prostate tissue as the volume of actually enucleated adenoma.
References
1. Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013; 64:118–140. PMID: 23541338.

2. McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803. PMID: 21420124.

3. Michalak J, Tzou D, Funk J. HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am J Clin Exp Urol. 2015; 3:36–42. PMID: 26069886.
5. Elzayat EA, Habib EI, Elhilali MM. Holmium laser enucleation of the prostate: a size-independent new “gold standard”. Urology. 2005; 66(5 Suppl):108–113.

6. Li S, Zeng XT, Ruan XL, Weng H, Liu TZ, Wang X, et al. Holmium laser enucleation versus transurethral resection in patients with benign prostate hyperplasia: an updated systematic review with meta-analysis and trial sequential analysis. PLoS One. 2014; 9:e101615. PMID: 25003963.

7. Oh JK, Bae J, Jeong CW, Paick JS, Oh SJ. Salvage Holmium laser enucleation of prostate to treat residual benign prostatic hyperplasia. Can Urol Assoc J. 2014; 8:E235–E240. PMID: 24839489.
8. Piao S, Choo MS, Kim M, Jeon HJ, Oh SJ. Holmium laser enucleation of the prostate is safe for patients above 80 years: a prospective study. Int Neurourol J. 2016; 20:143–150. PMID: 27377947.

9. Kim SB, Cho IC, Min SK. Prostate volume measurement by transrectal ultrasonography: comparison of height obtained by use of transaxial and midsagittal scanning. Korean J Urol. 2014; 55:470–474. PMID: 25045446.

10. Ku JH, Cho JY, Cho SY, Kim SW, Paick JS. The one year outcome after KTP laser vaporization of the prostate according to the calculated vaporized volume. J Korean Med Sci. 2009; 24:1187–1191. PMID: 19949680.

11. Lomas DJ, Krambeck AE. Long-term efficacy of holmium laser enucleation of the prostate in patients with detrusor underactivity or acontractility. Urology. 2016; 97:208–211. PMID: 27450935.

12. El Tayeb MM, Jacob JM, Bhojani N, Bammerlin E, Lingeman JE. Holmium laser enucleation of the prostate in patients requiring anticoagulation. J Endourol. 2016; 30:805–809. PMID: 27065437.

13. Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015; 67:1066–1096. PMID: 24972732.

Fig. 1
An example of postoperatively ultrasonographic assessment using ellipsoid method. (A) Postoperative prostate volume. (B) Defect volume.
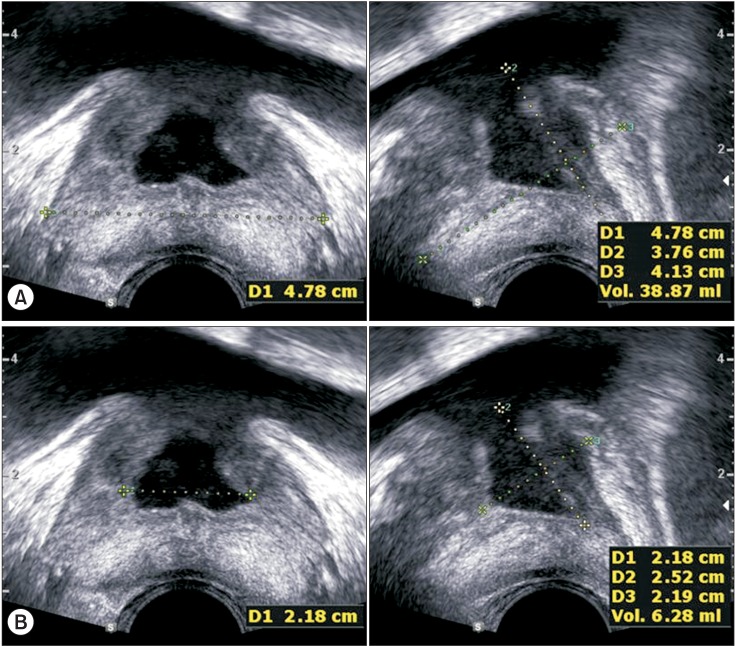
Table 1
Characteristics of clinical variables (n=142)
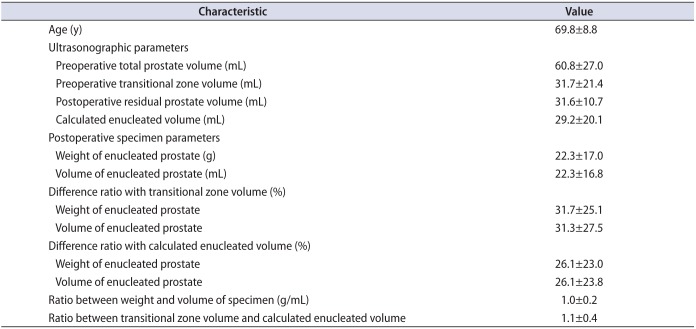
Table 2
Analysis of multiple linear regression model of comparison between transitional zone volume and clinical variables




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download