Abstract
Purpose
To evaluate the effect of ‘Bernoulli maneuver’ (bringing the access sheath to horizontal plane) on operative time and stone free rates in patients undergoing mini-percutaneous nephrolithotomy (PCNL).
Materials and Methods
All consecutive patients with a solitary kidney stone undergoing a mini-PCNL between 2015 and 2016 were included into this study. Patients were randomized either to standard prone or control (C) group patients or to tilted prone with ‘Bernoulli maneuver’ group (B) patients. Pre-, intra-, and postoperative characteristics of these 2 groups were recorded and analyzed.
Results
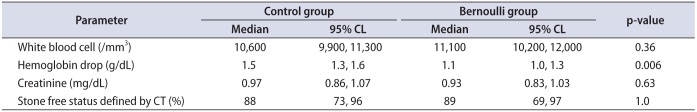
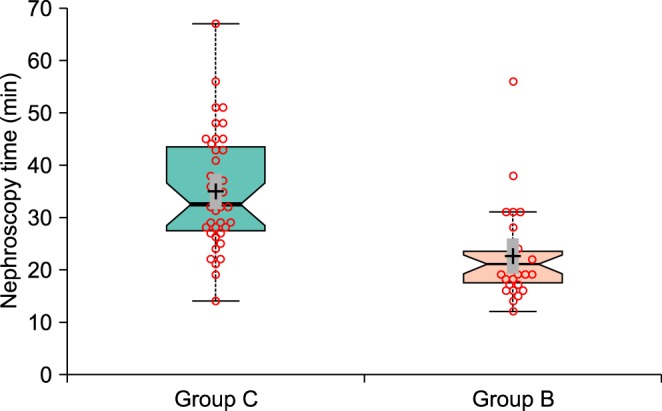
A total of 67 patients were included in the study. Of these, 40 patients were randomized to group C and 27 to group B. The mean (95% confidence limits) stone size (mm) in group C and B was 14 (13, 15) and 13 (11, 14), respectively (p=0.26). Nephroscopy time was shorter in Bernoulli group (35 minutes vs. 23 minutes, p=1.5·10-5, and Bayes factor BF10=2,340, and Cohen standardized effect size dst=1.2). The difference made it up 12 minutes (with 95% confidence interval from 8 to 18 minutes). There were no statistically significant differences between groups regarding white blood cell, creatinine level and stone-free status defined by computed tomography on the first postoperative day.
Since the first introduction of percutaneous nephrolithotomy (PCNL) in 1976 [1] it has become the gold standard surgical treatment for large kidney stones. In order to reduce the morbidity associated with PCNL, several attempts have been made to modify the standard technique and reduce the size of instrumentation used for PCNL. The first significant size reduction has been proposed by Helal et al. [2] in 1997, who described the ‘mini-PCNL’ technique in a 2-year-old child using 15 Fr. Hickman peel away introduction set. Further advances led to the development of metallic Amplatz sheath with nephroscope, where one of the prominent advantages was vacuum cleaner effect, consistent with hydrodynamic Bernoulli's principle [3]. According to this principle, during mini-PCNL, the front of a low pressure called ‘pseudocavity’ is produced at the tip of nephroscope, which can extract the stone fragments through an access sheath without any additional grasping devices [4]. At a closer look, we have noticed that the horizontal plane, being one of the necessary conditions for Bernoulli equation, possibly for negation of gravitational influence on the flow velocity [5], was for some reason neglected.
In this study, we evaluated whether bringing the access sheath during mini-PCNL to the horizontal plane, which we called ‘Bernoulli maneuver,’ by table manipulation and/or gentle hand assistance, can be beneficial regarding nephroscopy time. We compared the 2 groups of patients operated either in a standard prone or tilted prone position.
We obtained Institutional Review Board approval to perform a single center prospective, randomized and controlled study (approval number: ГНК - 72345). All patients undergoing mini-PCNL procedure between February 2015 and April 2016 for solitary medium-sized kidney stones (1–2 cm) of high density (more than 1,000 HU) were consented to be included in the study. Choice of treatment modality was dictated by existing guidelines [6] and local insurance coverage protocols. Randomization was performed via a web-based generator of true random numbers, in which the randomness comes from atmospheric noise (www.random.org) and results were assigned to the control (C) and Bernoulli (B) groups in numbered envelopes. Patients with multiple or complex renal stones, stones in anomalous kidneys as well as patients with active infection or coagulation disorders were excluded from the study. Patient demographics and stone characteristics are shown in Table 1.
All PCNL procedures were performed by 2 competent surgeons [7] under general anesthesia. With the patient in the lithotomy position, a ureteral catheter 6 Fr was placed into the stone-bearing kidney under cystoscopic guidance. Then the patient was turned to the prone position and strapped down at the upper body and buttocks to the operating table (Alphamax, Maquet, Germany) to prevent sliding during ‘Bernoulli maneuver’ (Fig. 1).
Our surgical technique has been described elsewhere [8]. Briefly, we routinely obtain percutaneous renal access under combined fluoroscopic and/or ultrasonic guidance. After calyceal puncture, a 0.035 hydrophilic guidewire (Roadrunner, Cook Medical, Bloomington, IN, USA) is inserted into the pelvicalyceal system (PCS). A ‘single-step’ tract dilation, with a 16.5/19.5 Fr metal access sheath, is performed (Karl Storz, Tuttlingen, Germany). A rigid nephroscopy is conducted with a rigid 12-Fr nephroscope (Karl Storz). After identification of the stone, according to the group assignment, the patient was operated in either standard prone (Fig. 2A) or tilted prone position (Fig. 2B), with the maximum intention to bring access sheath to horizontal. Gentle hand assistance was applied to maximize tilting if needed (Fig. 2C). Fragmentation of the stone mass instead of “laser painting” with the formation of fitting the access sheath particles, which were immediately evacuated via Bernoulli effect, was accomplished with laser lithotripter (VersaPulse 100 W, Lumenis, Israel) and 365 micron laser fiber, under the following initial parameters: 0.5 J and 20 Hz. Nor basket neither grasping device was needed during all operations. Nephrostomy/stent or totally tubeless ending was at the surgeons' discretion. Blood cell count and creatinine level were analyzed on the first postoperative day. Evaluated parameters in the study were nephroscopy time i.e., time from stone identification till the end of the evacuation of the last fragment, stone free and complication rates.
Low-dose computed tomography (CT) imaging was obtained on all patients on postoperative day 1 to evaluate residual stones. Data acquisition was performed using a 64-row CT unit Somatom Definition AS (Siemens, Berlin, Germany). Stone free rate was defined as residual stones less than <2 mm [9].
Our approach to the statistical data analysis could be named “harmonizing statistical evidences and predictions.” It is rather fruitful because it combines not only confidence interval estimates for parameters, for the standardized effect size dC, for the achieved power (1–β), and planned sample sizes, but prediction intervals for them and for p-values, as well as estimates of posterior probabilities for the null hypothesis P(H0│D) and Bayes factors BF10. For parameter estimation and hypothesis testing the complementary combination of frequentist (orthodox) and Bayesian approaches was used. Nonparametric bootstrapping and permutation (Monte Carlo) procedures were realized with the number of replicates and/or random permutations as large as possible (but no less than 1 million). For measurable variables (stone size and density) medians and their 95% confidence limits were calculated. Software PAST [10], BoxPlotR (http://boxplot.tyerslab.com/), JASP (https://jasp-stats.org/), G*Power [11] and LePrep (http://lmrs.univ-rouen.fr/Persopage/Lecoutre/PAC.htm) have been involved.
Total of 67 patients were included in the study; of these, 40 patients were randomized to group C and 27 patients to group B. Their ratio 1.5 with 95% confidence limits from 0.9 to 2.4 did not differ statistically from the expected 1:1 (p=0.14). Data in group C appeared not agree with a normal distribution (Table 1). So all statistical estimations and tests used were nonparametric. In group B the nephroscopy time was significantly shorter than in group C (Fig. 3).
The time difference between studying groups was 12.6 minutes (with 95% confidence interval from 8 to 18 minutes). Bayes factor BF10=2,340 means that the probability to receive the observed effect under the alternative hypothesis is 2,340 times larger than under the null hypothesis. At the same time, it means that the posterior odds in favor of the alternative hypothesis against the null hypothesis are 2,340 times larger then prior odds. This result agrees well with the high value of achieved power (Pow=0.998) and with a high probability of replication psrep=0.97. Prediction analysis shows that in replication the Cohen effect size dst will be not less than 0.49 and p-value will not exceed 0.027 with the probability 95% (Table 2).
Moderate positive correlation was observed between stone size and nephroscopy time, where linear Pearson correlation coefficient appeared to be r=0.53 (4.5·10-6) and Spearman correlation coefficient was rs=0.55 (1.4·10-6) (Fig. 4A) as well as between nephroscopy time and haemoglobin drop (Fig. 4B), r=0.66 (1.5·10-9) and rs=0.55 (5·10-11).
No intraoperative complications such as profuse bleeding, PCS rupture etc. have occurred in the study. There were no statistically significant differences between groups in terms white blood cell count, creatinine level and stone-free status defined by CT on the first postoperative day. Though we did find statistically significant difference in hemoglobin (Hb) drop between groups (less in group B), it was not clinically significant (Table 3).
PCNL is a challenging procedure with a steep learning curve. There are many factors that have been shown to impact the surgical outcomes of PCNL procedures. These variables include surgeon's experience, patient and stone characteristics. Due to the challenging nature of the procedure, there have been many modifications suggested to improve patient related outcomes and stone free rates.
In this study we evaluated a simple yet reproducible maneuver to improve stone free rates and nephroscopy time. The ‘Bernoulli maneuver,’ to our best knowledge, has never been evaluated before during PCNL procedures and this is the first study to quantitatively demonstrate the benefits of this simple technique. Our results demonstrated a shorter nephroscopy time in the ‘Bernoulli’ group. On average, we saved 12 minutes just on nephroscopy time when the ‘Bernoulli maneuver’ was used. Although this difference seems small and not very clinically significant, cumulatively makes a huge difference at tertiary centers such as our institution where we daily perform a high volume of surgical procedures for urolithiasis. Since this maneuver requires tilting the table, one should pay close attention for patient positioning and securing with tapes on the table to prevent slipping during the procedure. If the table tilting is not enough to bring access sheath to the horizontal plane then gentle hand assistance may be used, but not zealously – not to tear the kidney.
Although we did not assess surgeons' subjective opinion, we believe that the maneuver makes the stone fragmentation and removal significantly easy. Possible explanation for the observed pattern may be reduced gravitational influence with the implementation of the ‘Bernoulli maneuver.’ Moreover, one can observe a comparative easiness of fragments washout during standard PCNL in the supine position [12], though this effect does not occur so prominently in standard PCNL as compared to mini-PCNL [13].
Our study demonstrated positive correlations between the stone size and operative time, nephroscopy time and decrease in Hb level. These findings are consistent with the previous studies [1415].
Today definition of mini-PCNL comprises utilization of access sheaths of size 14–20 Fr [1516]. According to this definition the first mention of ‘mini PCNL’ was made by Helal et al. [17] in 1997 using 15 Fr. Hickman peel away catheter, followed by Jackman et al. [18] in 1998 utilizing an 11 Fr. peel-away access sheath, with comparable to standard PCNL results. The first description of standard “minimally invasive PCNL” with specialized 12-Fr rigid nephroscope and 15-Fr access sheath came out in 2001. However, according to the authors' note, despite the fact that no hemorrhage has occurred in a group of 19 patients, miniaturized instruments were associated with significant operative time increase with larger stone masses [19], due to the fact that utilization of a smaller sheaths are associated with more difficult stone fragment retrieval and need of additional tools such as disposable retrieval baskets [4]. It was not until Nagele et al. [3] in 2008 reported on a “Newly Designed Amplatz Sheath” (Karl Storz) with the vacuum cleaner effect, which was nicely depicted in a study by Nicklas et al. [4]. The basis of this effect lies in Bernoulli's principle, according to which an increase in the speed of a fluid in the constriction zone occurs simultaneously with a decrease in pressure [20], also known as ‘pseudocavity’ which is being located at the tip of the nephroscope during mini-PCNL able to extract stone fragments through access sheath without any additional stone extracting devices [4]. Besides ‘Bernoulli effect’ or ‘Vacuum cleaner effect’ passive or active wash out as well as purging effect can also be utilized to gain maximum stonefree rate during mini-PCNL, though were not used in our study [21].
Several attempts have been made to compare mini-PCNL to standard PCNL. The former has been shown to be associated with reduced morbidity, pain and blood loss compared to standard PCNL [2223]. In a series of more than 1,000 patients using a 16-Fr access sheath bleeding complications occurred in less than 1.5% [24]. For medium sized stones (1–2 cm) no significant differences between mini- and standard PCNL regarding stone free and complication rates were observed. However hospital stay and Hb drop were less in the mini-PCNL group. The only parameter was in favor to standard PCNL - the operative time, which was 12–14 minutes shorter in average [14]. Suggested in our study ‘Bernoulli maneuver’ with its additional 12 minutes possibly could offset this time difference making mini-PCNL an attractive option for medium sized stones (1–2 cm). One can raise a fair question, if SWL is not an option due to unfavorable stone factors [25], why not to use an endoscopic removal in medium-sized stones instead of mini-PCNL as existing guidelines dictate? [6]. The answer lies in residual fragments. As was nicely depicted even miniscule residuals <1 mm could affect an early recurrence, possibly to a delayed nidus effect [26]. Not speaking about time and expenditures needed to leave a patient absolutely stone-free with the endoscopic route.
Our study has limitations that should be mentioned. First, the study is a single-surgical-center study thus generalizability of this data is limited. Moreover during mini-PCNL in control group to render patient stone-free the sheath is often moved in all types of directions, which is also should be considered. Second, the study sample size is relatively low and larger studies are required. Finally, surgeon's subjective feeling was not measured and future studies with validated questionnaires would help to elucidate if the maneuver makes clinically significant difference to the surgeon during the procedure.
ACKNOWLEDGMENTS
We would like to thank Dr. Nikita Khromov-Borisov for his assistance with statistical analysis.
References
1. Fernström I, Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol. 1976; 10:257–259. PMID: 1006190.
2. Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997; 11:171–172. PMID: 9181444.

3. Nagele U, Horstmann M, Sievert KD, Kuczyk MA, Walcher U, Hennenlotter J, et al. A newly designed amplatz sheath decreases intrapelvic irrigation pressure during mini-percutaneous nephrolitholapaxy: an in-vitro pressure-measurement and microscopic study. J Endourol. 2007; 21:1113–1116. PMID: 17941796.

4. Nicklas AP, Schilling D, Bader MJ, Herrmann TR, Nagele U. Training and Research in Urological Surgery and Technology (T.R.U.S.T.)-Group. The vacuum cleaner effect in minimally invasive percutaneous nephrolitholapaxy. World J Urol. 2015; 33:1847–1853. PMID: 25833660.

5. Eastwell PH. Bernoulli? Perhaps, but what about viscosity? Sci Educ Rev. 2007; 6:1–13.
6. Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016; 69:475–482. PMID: 26344917.

7. Mishra S, Jagtap J, Sabnis RB, Desai MR. Training in percutaneous nephrolithotomy. Curr Opin Urol. 2013; 23:147–151. PMID: 23357932.

8. Gadzhiev N, Brovkin S, Grigoryev V, Tagirov N, Korol V, Petrov S. Sculpturing in urology, or how to make percutaneous nephrolithotomy easier. J Endourol. 2015; 29:512–517. PMID: 25321395.

9. Raman JD, Bagrodia A, Gupta A, Bensalah K, Cadeddu JA, Lotan Y, et al. Natural history of residual fragments following percutaneous nephrostolithotomy. J Urol. 2009; 181:1163–1168. PMID: 19152935.

10. Hammer Ø, Harper DA, Ryan PD. PAST: paleontological statistics software package for education and data analysis. Palaeontol Electron. 2001; 4:9–18.
11. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191. PMID: 17695343.
12. Kumar P, Bach C, Kachrilas S, Papatsoris AG, Buchholz N, Masood J. Supine percutaneous nephrolithotomy (PCNL): ‘in vogue’ but in which position? BJU Int. 2012; 110(11 Pt C):E1018–E1021. PMID: 22564784.

13. Ganpule AP, Bhattu AS, Desai M. PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol. 2015; 33:235–240. PMID: 25316173.

14. Mishra S, Sharma R, Garg C, Kurien A, Sabnis R, Desai M. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int. 2011; 108:896–899. PMID: 21477212.
15. Wright A, Rukin N, Smith D, De la Rosette J, Somani BK. ‘Mini, ultra, micro’ - nomenclature and cost of these new minimally invasive percutaneous nephrolithotomy (PCNL) techniques. Ther Adv Urol. 2016; 8:142–146. PMID: 27034726.

16. Sabnis RB, Ganesamoni R, Sarpal R. Miniperc: what is its current status? Curr Opin Urol. 2012; 22:129–133. PMID: 22273758.
17. Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997; 11:171–172. PMID: 9181444.

18. Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: experience with a new technique. Urology. 1998; 52:697–701. PMID: 9763096.

19. Lahme S, Bichler KH, Strohmaier WL, Götz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol. 2001; 40:619–624. PMID: 11805407.

20. Rassweiler J, Rassweiler MC, Klein J. New technology in ureteroscopy and percutaneous nephrolithotomy. Curr Opin Urol. 2016; 26:95–106. PMID: 26626887.

21. Nagele U, Nicklas A. Vacuum cleaner effect, purging effect, active and passive wash out: a new terminology in hydrodynamic stone retrival is arising--Does it affect our endourologic routine? World J Urol. 2016; 34:143–144. PMID: 26002252.

22. Yamaguchi A, Skolarikos A, Buchholz NP, Chomón GB, Grasso M, Saba P, et al. Operating times and bleeding complications in percutaneous nephrolithotomy: a comparison of tract dilation methods in 5,537 patients in the Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study. J Endourol. 2011; 25:933–939. PMID: 21568697.

23. Knoll T, Wezel F, Michel MS, Honeck P, Wendt-Nordahl G. Do patients benefit from miniaturized tubeless percutaneous nephrolithotomy? A comparative prospective study. J Endourol. 2010; 24:1075–1079. PMID: 20575685.

24. Hu G, Guo Z, Liu H, Luo M, Liu M, Lai P, et al. A novel minimally invasive percutaneous nephrolithotomy technique: safety and efficacy report. Scand J Urol. 2015; 49:174–180. PMID: 25247463.

25. El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: the value of high-resolution noncontrast computed tomography. Eur Urol. 2007; 51:1688–1693. PMID: 17161522.

26. Hein S, Miernik A, Wilhelm K, Schlager D, Schoeb DS, Adams F, et al. Endoscopically determined stone clearance predicts disease recurrence within 5 years after retrograde intrarenal surgery. J Endourol. 2016; 30:644–649. PMID: 27021947.

Fig. 4
Correlations between stone size and nephroscopy time (A) and between nephroscopy time and haemoglobin drop (B). 95% confidence ellipses are shown. r, linear Pearson correlation coefficient; rS, Spearman correlation coefficient.

Table 1
Relevant patient characteristics
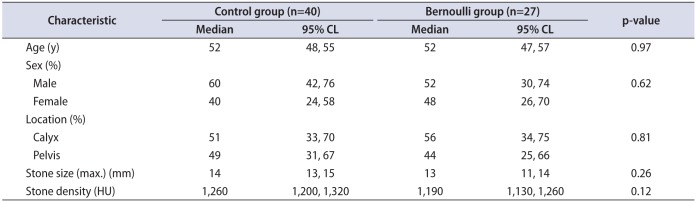
Table 2
Comprehensive data analysis (statistical descriptions, tests, effect size measures, power, and predictions) of nephroscopy time in both groups
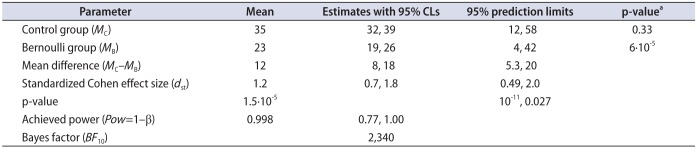
Table 3
Postoperative parameters




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download