Abstract
Purpose
Robot-assisted radical cystectomy (RARC) was originally intended to replace open radical cystectomy (ORC) as a minimally invasive surgery for patients with invasive bladder cancer. The purpose of this study was to evaluate the advantages of robotic surgery, comparing perioperative and oncologic outcomes between RARC and ORC.
Materials and Methods
Between June 2012 and August 2016, 49 bladder cancer patients were given a radical cystectomy, 21 robotically and 28 by open procedure. We compared the clinical variables between the RARC and ORC groups.
Results
In the RARC group, the median estimated blood loss (EBL) during cystectomy, total EBL, operative time during cystectomy, and total operative time were 0 mL, 457.5 mL, 199 minutes, and 561 minutes, respectively. EBL during cystectomy (p<0.001), total EBL (p<0.001), and operative time during cystectomy (p=0.003) in the RARC group were significantly lower compared with the ORC group. Time to resumption of a regular diet (p<0.001) and length of stay (p=0.017) were also significantly shorter compared with the ORC group. However, total operative time in the RARC group (median, 561 minutes) was significantly longer compared with the ORC group (median, 492.5 minutes; p=0.015).
The gold standard treatment for nonmetastatic muscle-invasive and bacille Calmette-Guerin (BCG)-refractory, high-risk nonmuscle invasive bladder cancer (BC) is open radical cystectomy (ORC) with pelvic lymph node dissection (PLND) [1]. ORC with urinary diversion, however, remains a morbid operation with a substantial complication rate, mainly due to long operation time and blood loss [2]. The use of robot-assisted radical cystectomy (RARC) is on the rise [3] as a means of lessening invasiveness.
During the last decade, perioperative and short-term outcomes have demonstrated that RARC is a potential treatment alternative to ORC. The International Robotic Cystectomy Consortium (IRCC) has reported over 1,000 cases of RARC [4]. However, despite publication of a few studies reporting lower or comparable rates of complications, quicker recovery, and equivalent oncologic outcomes compared with ORC, RARC is not yet viewed as an alternative to ORC [5678]. In this study, we report our initial experience with RARC and analyze whether this method produced merits in comparison with ORC.
Between November 2012 and August 2016, 2 surgeons consecutively performed RARC on 21 patients. The indications for RC were muscle-invasive BC without distant metastasis (clinical T [cT] 2–4, NX, M0) and recurrent, nonmuscle invasive BC refractory to repeat transurethral resection with intravesical therapy of BCG. The TNM stage of the BC was determined according to the 2010 Union for International Cancer Control TNM classification of BC [9]. The relative or absolute exclusion criteria for RARC were a history of radiotherapy and a contraindication to the steep Trendelenburg position such as a decrease in pulmonary compliance, glaucoma, cerebral aneurysm, and severe hypertension. Patients with bulky disease were also excluded as RARC candidates. Patients failing to meet the RARC criteria received ORC, while those meeting the criteria were given the choice between RARC and ORC. In all, 28 patients selected ORC and were included in this study as a control group. This retrospective observational study was approved by Teikyo University Institutional Review Board (approval number: 11078) and was performed in adherence to the Declaration of Helsinki. All participants gave written informed consent.
Data were collected retrospectively on patient details, operative outcomes and follow-up. We reviewed the patient demographics, including age and peri- and postoperative outcomes and made parameter comparisons between the RARC and ORC groups. Total operative time is the time from start to finish of the operation including cystectomy, lymphadenectomy, and urinary diversion in both intracorporeal robotic surgery and laparotomy. The operative time during cystectomy is from start to finish of the cystectomy procedure itself. Total EBL is the total hemorrhage volume during total operative time, while EBL during cystectomy is the hemorrhage volume from the start of operation to the end of cystectomy in both RARC and ORC. In this study, we defined the time to flatus as the number of postoperative days to flatus. The adverse events related to surgery were graded according to the Clavien-Dindo classification [10].
The surgeries were performed with da Vinci S, Si, Xi (Intuitive Surgical Inc., Sunnyvale, CA, USA) robotic assistance. All RARCs were performed by 2 surgeons (SM, SH). Although both surgeons had significant previous experience in ORCs, having participated in over 200 such procedures, their experience with laparoscopic radical cystectomy was limited. Additionally, although both surgeons had experienced over 40 cases involving Robot-assisted radical prostatectomy (RARP), this study was their initial experience with RARC. PLND ranged from the outer side to the genitofemoral nerve, the proximal side to the bifurcation of the common iliac artery, and the caudal side to the node of Cloquet. In the initial 8 cases, PLND was performed extracorporeally after robotic extirpation of the bladder. We subsequently performed intracorporeal PLND for all cases. Urinary diversions were performed extracorporeally after PLND through a midline incision extending 6–8 cm from the camera port in 17 cases. Orthotopic neobladders were created using the Studer method. Ureteroileal anastomoses of the ileal conduit or neobladder were constructed with Wallace ureteroileal anastomoses [11]. In 4 cases, we performed intracorporeal ileal conduit urinary diversion. We universally inserted a ureteral stent into the renal pelvis, regardless of urinary diversion type. In this study, we did not incorporate either the Fast-track program or Enhanced Recovery After Surgery (ERAS) protocol due to lack of experience.
The effects of factors were quantified by odds ratios and statistical analysis using Pearson chi-square test. Oncologic outcomes including progression-free survival (PFS) and overall survival (OS) of RARC and ORC were compared using a Kaplan-Meier analysis. Statistical analysis was performed using R ver. 2.14.1 (R Foundation for Statistical Computing, Vienna, Austria) [12]. Two-tailed p-values of less than 0.05 were considered to indicate a statistically significant difference.
Patient clinical preoperative characteristics are summarized in Table 1. The average age of the RARC group was 66.8 years. In the RARC group, 14 patients (66.7%) received ileal conduit diversion surgery, and 6 (28.6%) received ileal neobladder reconstruction. The frequency of neobladder-type urinary diversion was significantly higher in the RARC group than in the ORC group (3.6%, p=0.047).
Nine patients (42.9%) in the RARC group and 9 patients (32.1%) in the ORC group received neoadjuvant chemotherapy consisting of gemcitabine or cisplatin. No patients in either group had undergone preoperative radiotherapy. One patient in the RARC group received 2 courses of cisplatin and gemcitabine adjuvant chemotherapy for pT4a disease with pN2. Two of the patients in the ORC group received 2 courses of gemcitabine and carboplatin for pT3 or pT4a disease with pN2. There were no significant differences between the RARC and ORC groups in age (p=0.174), body mass index (p=0.523), past history of abdominal surgery (p=0.609), frequency of neoadjuvant chemotherapy (p=0.638), clinical T (p=0.645) and N stage (p=0.919), and follow-up periods (p=0.174) (Table 1). There were 2 patients over 80 years of age in the RARC group (9.5%) and 5 in the ORC group (17.9%) (p=0.409).
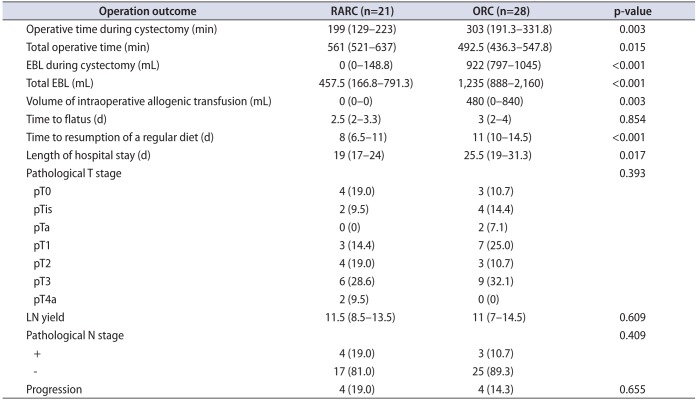
In the RARC group, median console time was 218 minutes (interquartile range [IQR], 200–285 minutes) and median total operative time was 561 minutes (IQR, 521–637 minutes), the latter significantly longer than in the ORC group (median, 492.5 minutes; IQR, 436.3–547.8 minutes; p=0.015). However, operative time during cystectomy in the RARC group (median, 199 minutes; IQR, 129–223 minutes) was significantly shorter compared with the ORC group (median, 303 minutes; IQR, 191.3–331.8 minutes, p=0.003). EBL during cystectomy (median, 0 mL; IQR, 0–148.8 mL) and total EBL in the RARC group (median, 457.5 mL; IQR, 166.8–791.3 mL) were significantly lower compared with the ORC group (p<0.001). As a consequence, the volume of intraoperative allogenic transfusion in the RARC group (median, 0 mL; IQR, 0–0 mL) was significantly decreased compared with the ORC group (median, 480 mL; IQR, 0–840 mL; p=0.003). RARC resulted in significantly faster postoperative resumption of regular diet (p<0.001), as well as shorter length of stay (LOS) (p=0.017).
Both groups experienced postoperative adverse events. The RARC group confirmed 1 case (4.8%) each of grade IIIa anastomotic stenosis of the neobladder, grade IIIa paralytic ileus, and grade II metabolic acidosis, and 2 cases (9.6%) of grade II pyelonephritis. On the other hand, the ORC group confirmed 1 case (3.6%) each of grade IIIa postoperative blood loss, grade IIIa anastomotic stenosis of the neobladder, grade II cutaneous-neobladder fistula, grade II iliac venous thrombosis, and grade II ileus, 2 cases (7.1%) each of grade IIIb rectal injury and grade II leg edema, and 3 cases (10.7%) of grade II pyelonephritis. There were no significant differences in the frequency of complications between both groups (p=0.166).
Pathological results for the RARC group were as follows: pT0 (n=4), pTis (n=2), pT1 (n=3), pT2 (n=4), pT3 (n=6), and pT4a (n=2). These results were not significantly different from those of the ORC group (p=0.393) (Table 2). All patients underwent extended PLND, except one case in the ORC group. The median number of lymph nodes removed in the RARC group was 11.5 (IQR, 8.5–13.5), with 4 cases of lymph node metastasis to obturator lymph nodes; the median number of removed lymph nodes was also 16 (IQR, 11–18) in the ORC group, with 3 cases of obturator lymph node metastasis. There was no significant difference in number of removed lymph nodes (p=0.807) or degree of node metastasis (p=0.409) between the 2 groups.
There was no significant difference (Table 1) (p=0.174) in the median follow-up period between the RARC (26 months; IQR, 8–32 months) and ORC (17.5 months; IQR, 7–23.5 months) groups, or in postoperative progression for the 2 groups (Table 2) (p=0.655). The RARC group had 2 cases of lymph node and lung metastasis, 1 case of pelvic local recurrence, and 1 case of sacral metastasis. On the other hand, the ORC group had 2 cases of lymph node metastasis, 1 case of pelvic local recurrence, and 1 case of peritoneal dissemination. There were no significant differences in PFS (p=0.732; Fig. 1A) and OS (p=0.401; Fig. 1B) between the RARC (mean: PFS, 37.4 months; OS, 40.2 months) and ORC groups (mean: PFS, 30.9 months; OS, 34.8 months).
In IRCC outcomes, mean EBL in RARC was 401 mL and 16% of the patients required a blood transfusion [4]. In their systematic review and meta-analysis, Li et al. [13] reported that evaluated EBL was significantly lower in the RARC group than in the ORC group (p<0.001). It has been reported that if EBL is low, perioperative mortality and morbidity rates are also low [14], which may be one of the main advantages of RARC. In this study, median EBL during cystectomy was 0 mL (IQR, 0–148.8 mL) and median total EBL was 457.5 mL (IQR, 166.8–791.3 mL). Both EBL during cystectomy and total EBL were significantly lower in the RARC group than the ORC group (p<0.001). Our study clarifies that, although RARC is still in its early stages of usage, it already contributes to lower blood loss than does ORC.
RARC tends to require slightly longer operative time. Bak et al. [15] reported that the median operative time was 75 minutes longer in the RARC group than in the ORC group. Li et al. [13] reported in their systematic review and meta-analysis that data of 668 patients showed significantly longer operative times in the RARC than in the ORC group (p<0.001). Due to limited experience with the technique, we used robot-assisted surgery only through the radical cystectomy and then performed open surgery for the remaining procedures, including lymphadenectomy in the initial 8 cases, and urinary diversion extracorporeally in 17 cases in this study. Furthermore, in terms of urinary diversion type, the number of ileal neobladders in the RARC group was significantly higher than in the ORC group (p=0.174) (Table 1). As a result, although the operative time during cystectomy in the RARC group was significant shorter than in the ORC group (p=0.003) (Table 2), the total operative time was significantly longer in the RARC group compared with the ORC group (p=0.015) (Table 2). In multivariable analysis, age, American Society of Anesthesiologists physical status classification, preoperative hematocrit, and operative time were independent predictors of complications of any grade after RARC [16]. Therefore, shortening operative time will be critical in reducing postoperative complications. A potentially steep learning curve was reported regarding laparoscopic and robotic surgery [17]. Collins et al. [18] reported that operative time decreased significantly with experience. In the IRCC report [4], the median total operative times were 441, 368, and 307 minutes for those surgeons who had experienced fewer than 30 cases, 30–50 cases, and more than 50 cases, respectively (p<0.0001). These results show a correlation between surgical volume and total operative time. Accordingly, we may expect shorter operative times as more RARC experience is gained. In the present study, although the median console time for radical cystectomy alone was 199 minutes (IQR, 129–223 minutes), as cases proceeded, time shortened.
A robotic approach has been shown to reduce the complication rates compared to ORC. Bak et al. [15] reported that the RARC group showed a lower major complication rate compared with the ORC group and zero perioperative mortality. Li et al. [13] reported that, in terms of overall perioperative complications in 474 patients, those in the RARC group showed a significantly lower rate of such complications as compared to the ORC group. We did not find significant differences between the RARC and ORC groups in this study. Our experience showed, however, that RARC can be as safe as ORC, despite the fact that overall robotic surgical experience remains low. Age is one of the independent risk factors for mortality after radical cystectomy [19]. Therefore, robotic surgery offers a promising way for elderly patients to receive minimally invasive cystectomy. Izquierdo et al. [20] reported that perioperative mortality rates and complications rates of ORC in previous reports have varied widely from 0% to 14% and from 17% to 67%, respectively. In this study, we only performed RARC on 2 patients over 80 years of age. So, although we could not assess the influences of RARC on mortality and complications for elderly patients, we have a need to verify the effects of RARC on elderly patients. Some studies [2122] have reported that performing RARC on elderly patients does not result in worse perioperative complications or pathologic outcomes compared with younger patients. In particular, deep venous thrombosis (DVT) is recognized as one of the most serious complications of pelvic surgery [23]. There are no known reports of DVT complications among RARC patients. It was reported, however, that the incidence of DVT in patients undergoing radical cystectomy was higher than in those receiving radical prostatectomy [23]. With regard to radical prostatectomy, it is not established whether a robotic or an open procedure is preferable in terms of preventing DVT. Therefore, we must shed light on the effectiveness of RARC in DVT management.
In this study, the RARC group could postoperatively return to a regular diet significantly earlier than the ORC group (Table 2). We performed extracorporeal urinary diversion in many cases, with both RARC and ORC groups following the same protocol for intestinal tract preparation. Furthermore, the neobladder reconstruction rate was significantly higher in the RARC group compared with the ORC group in this study (p=0.047) (Table 1). It is well known that an EBL greater than 600 mL is significantly associated with an increased risk of postoperative ileus [24]. Therefore, the RARC group showed a faster return to a regular diet, indicating that the significantly lower blood loss in RARC has some impact. Fast-track programs and the ERAS protocol have attracted attention over the years, as has radical cystectomy. Enormous problems are associated with the ERAS protocol, such as its effect on medical costs or QoL, its uncertain specificity for cystectomy, and the fact that it remains unestablished. At the same time, the Robotic Urology Section's Scientific Working Group in the European Association of Urology recognized the role of enhanced recovery programs and endorses them as standardized perioperative care for patients undergoing RARC [25]. Therefore, although we could not examine the ERAS protocol in this study, evaluating RARC with the ERAS protocol [26] remains a future priority.
In spite of little experience with RARC, our total operative time was not much longer than that with ORC. As LOS in the RARC group was significantly shorter than in the ORC group, performing RARC would have merit even during the introductory period of robotic surgery. Although many medical facilities are introducing robotic surgery for RARP in Japan, which is covered by national health insurance, our results in this study suggest potential for RARC even during the initial experience. There is evidence that surgeons experienced in ORC have a short learning curve in RARC for oncologic outcomes [4]. This study demonstrates that ORC-experienced surgeons can perform RARC safely and meaningfully. Previous studies [1527] reported that there were no significant differences in PFS and OS between RARC and ORC. Based on our study, we concur with those findings. This oncologic outcome was the strongest point in selecting RARC.
The present study has some limitations that must be considered. One is that the sample size of this study was too small. EBL during cystectomy, time to resumption of a regular diet, and LOS can be considered statistically significant even if the number of cases is low, while larger series with long-term follow-up are needed before RARC can be considered a viable alternative to ORC. Cost-effectiveness analysis was lacking in this investigation. Several studies have reported comparisons of RARC and ORC costs. Although many papers reported that RARC was pricier due to increased material cost, when complications, LOS, and operating time are taken into consideration, RARC appears to be more cost-effective [28]. In addition, the present series was a single-group retrospective study. Treatment selection bias between RARC and ORC cannot be ignored; a multicenter, collaborative prospective study is necessary for more accurate evaluations. In this study, our staffs were aware of which technique was being employed: RARC or ORC. Therefore, their knowledge had potential to affect LOS and time to flatus. Finally, as the follow-up period was generally short, long-term outcomes of RARC (as compared with ORC) have yet to be proven, particularly in terms of cancer control, urinary continence, and sexual potency.
References
1. Jensen JB, Ulhøi BP, Jensen KM. Extended versus limited lymph node dissection in radical cystectomy: impact on recurrence pattern and survival. Int J Urol. 2012; 19:39–47. PMID: 22050425.

2. Roghmann F, Trinh QD, Braun K, von Bodman C, Brock M, Noldus J, et al. Standardized assessment of complications in a contemporary series of European patients undergoing radical cystectomy. Int J Urol. 2014; 21:143–149. PMID: 23906282.

3. Challacombe BJ, Bochner BH, Dasgupta P, Gill I, Guru K, Herr H, et al. The role of laparoscopic and robotic cystectomy in the management of muscle-invasive bladder cancer with special emphasis on cancer control and complications. Eur Urol. 2011; 60:767–775. PMID: 21620562.

4. Hayn MH, Hussain A, Mansour AM, Andrews PE, Carpentier P, Castle E, et al. The learning curve of robot-assisted radical cystectomy: results from the International Robotic Cystectomy Consortium. Eur Urol. 2010; 58:197–202. PMID: 20434830.

5. Atmaca AF, Canda AE, Gok B, Akbulut Z, Altinova S, Balbay MD. Open versus robotic radical cystectomy with intracorporeal Studer diversion. JSLS. 2015; 19:e2014.

6. Kader AK, Richards KA, Krane LS, Pettus JA, Smith JJ, Hemal AK. Robot-assisted laparoscopic vs open radical cystectomy: comparison of complications and perioperative oncological outcomes in 200 patients. BJU Int. 2013; 112:E290–E294. PMID: 23815802.

7. Styn NR, Montgomery JS, Wood DP, Hafez KS, Lee CT, Tallman C, et al. Matched comparison of robotic-assisted and open radical cystectomy. Urology. 2012; 79:1303–1308. PMID: 22516354.

8. Sung HH, Ahn JS, Seo SI, Jeon SS, Choi HY, Lee HM, et al. A comparison of early complications between open and robot-assisted radical cystectomy. J Endourol. 2012; 26:670–675. PMID: 22011001.

9. Sobin LH, Gospodarowicz M, Wittekind C, editors. International Union Against Cancer (UICC). TNM Classification of Malignant Tumours. 7th ed. Hoboken (NJ): Wiley-Blackwell;2010.
10. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
11. Shigemura K, Yamanaka N, Imanishi O, Yamashita M. Wallace direct versus anti-reflux Le Duc ureteroileal anastomosis: comparative analysis in modified Studer orthotopic neobladder reconstruction. Int J Urol. 2012; 19:49–53. PMID: 22004164.

12. R Development Core Team. R. a language and environment for statistical computing. Vienna (Austria): R Foundation for Statistical Computing;2011.
13. Li K, Lin T, Fan X, Xu K, Bi L, Duan Y, et al. Systematic review and meta-analysis of comparative studies reporting early outcomes after robot-assisted radical cystectomy versus open radical cystectomy. Cancer Treat Rev. 2013; 39:551–560. PMID: 23273846.

14. Wu WC, Smith TS, Henderson WG, Eaton CB, Poses RM, Uttley G, et al. Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann Surg. 2010; 252:11–17. PMID: 20505504.

15. Bak DJ, Lee YJ, Woo MJ, Chung JW, Ha YS, Kim HT, et al. Complications and oncologic outcomes following robot-assisted radical cystectomy: what is the real benefit? Investig Clin Urol. 2016; 57:260–267.

16. Yuh BE, Nazmy M, Ruel NH, Jankowski JT, Menchaca AR, Torrey RR, et al. Standardized analysis of frequency and severity of complications after robot-assisted radical cystectomy. Eur Urol. 2012; 62:806–813. PMID: 22705382.

17. Goh AC, Gill IS, Lee DJ, de Castro Abreu AL, Fairey AS, Leslie S, et al. Robotic intracorporeal orthotopic ileal neobladder: replicating open surgical principles. Eur Urol. 2012; 62:891–901. PMID: 22920581.

18. Collins JW, Tyritzis S, Nyberg T, Schumacher MC, Laurin O, Adding C, et al. Robot-assisted radical cystectomy (RARC) with intracorporeal neobladder - what is the effect of the learning curve on outcomes? BJU Int. 2014; 113:100–107. PMID: 24053710.

19. Novotny V, Froehner M, Koch R, Zastrow S, Heberling U, Leike S, et al. Age, American Society of Anesthesiologists physical status classification and Charlson score are independent predictors of 90-day mortality after radical cystectomy. World J Urol. 2016; 34:1123–1129. PMID: 26658887.

20. Izquierdo L, Peri L, Leon P, Ramírez-Backhaus M, Manning T, Alcaraz A, et al. The role of cystectomy in elderly patients - a multicentre analysis. BJU Int. 2015; 116(Suppl 3):73–79. PMID: 26333289.

21. Guillotreau J, Miocinovic R, Gamé X, Forest S, Malavaud B, Kaouk J, et al. Outcomes of laparoscopic and robotic radical cystectomy in the elderly patients. Urology. 2012; 79:585–590. PMID: 22386404.

22. Coward RM, Smith A, Raynor M, Nielsen M, Wallen EM, Pruthi RS. Feasibility and outcomes of robotic-assisted laparoscopic radical cystectomy for bladder cancer in older patients. Urology. 2011; 77:1111–1114. PMID: 21333341.

23. Chen EC, Papa N, Lawrentschuk N, Bolton D, Sengupta S. Incidence and risk factors of venous thromboembolism after pelvic uro-oncologic surgery: a single center experience. BJU Int. 2016; 117(Suppl 4):50–53. PMID: 26486818.
24. Chang SS, Cookson MS, Baumgartner RG, Wells N, Smith JA Jr. Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol. 2002; 167:2012–2016. PMID: 11956429.

25. Collins JW, Patel H, Adding C, Annerstedt M, Dasgupta P, Khan SM, et al. Enhanced recovery after robot-assisted radical cystectomy: EAU Robotic Urology Section Scientific Working Group Consensus View. Eur Urol. 2016; 70:649–660. PMID: 27234997.

26. Mir MC, Zargar H, Bolton DM, Murphy DG, Lawrentschuk N. Enhanced recovery after surgery protocols for radical cystectomy surgery: review of current evidence and local protocols. ANZ J Surg. 2015; 85:514–520. PMID: 25781409.

27. Nepple KG, Strope SA, Grubb RL 3rd, Kibel AS. Early oncologic outcomes of robotic vs. open radical cystectomy for urothelial cancer. Urol Oncol. 2013; 31:894–898. PMID: 21803615.

28. Lee R, Chughtai B, Herman M, Shariat SF, Scherr DS. Cost-analysis comparison of robot-assisted laparoscopic radical cystectomy (RC) vs open RC. BJU Int. 2011; 108(6 Pt 2):976–983. PMID: 21917100.

Fig. 1
Kaplan-Meier estimated survival between RARC and ORC. There are no significant differences in PFS (p=0.732; A) and OS (p=0.401; B) between the RARC (mean: PFS, 37.4 months; OS, 40.2 months) and ORC groups (mean: PFS, 30.9 months; OS, 34.8 months). RARC, robot-assisted radical cystectomy; ORC, open radical cystectomy; PFS, progression-free survival; OS, overall survival.
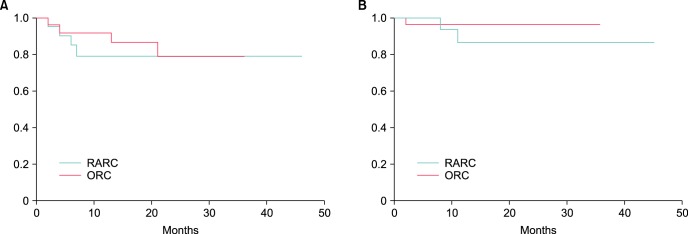
Table 1
Patient characteristics
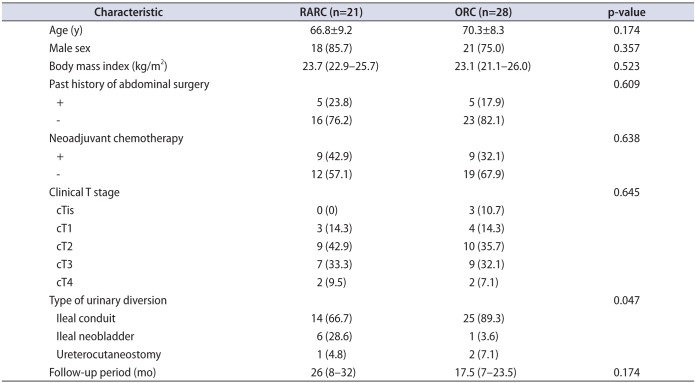
Table 2
Operation outcomes




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download