Abstract
High-grade T1 bladder cancer has a poor prognosis due to a higher incidence of recurrence and progression than other nonmuscle invasive bladder cancer; thus patients with high-grade T1 have to be carefully monitored and managed. If patients are diagnosed with high-grade T1 at initial transurethral resection (TUR), a second TUR is strongly recommended regardless of whether muscle layer is present in the specimen because of the possibility of understating due to incomplete resection. Since high-grade T1 disease shows diverse clinical courses, individual approaches are recommended for treatment. In cases with low risk of progression, cystectomy could represent overtreatment and deteriorate quality of life irreversibly, while, in those with high risk, bacillus Calmette-Guérin (BCG) therapy may worsen survival by delaying definitive therapy. Therefore, a strategy for predicting prognosis based on the risk of progression is needed for managing high-grade T1 disease. Molecular risk classifiers predicting the risk of progression and response to BCG may help identify the optimal management of high-grade T1 disease for each individual.
Bladder cancer is the ninth most common cancer in the world; 3,762 patients were newly diagnosed with bladder cancer and 1,280 died from it in Korea in 2013 [12]. The most common cell type of bladder cancer is urothelial cancer, and about 70%–80% of these are nonmuscle invasive bladder cancers (NMIBCs), while the other 20%–30% are muscle invasive bladder cancers (MIBCs). MIBC has a poor prognosis due to invasion or metastasis to other organs. NMIBC has a high recurrence rate (up to 50%) and progression (10%–30%), and thus is a great burden to patients [3]. Moreover, T1 disease, which invades the lamina propria, and poorly differentiated high-grade disease have a poor prognosis due to a higher incidence of recurrence and progression than other NMIBC; thus patients with high-grade T1 have to be carefully monitored or managed. Although bacillus Calmette-Guérin (BCG) followed by transurethral resection (TUR) is known as the gold standard treatment, controversies remain over whether BCG can reduce the progression rate of highgrade T1 [45]. One third of high-grade T1 patients who receive intravesical BCG therapy progress to MIBC [6] and are at risk of dying from bladder cancer because ineffective BCG therapy delays radical cystectomy [7]. Nevertheless, there is no consensus about how to predict progression and manage high-grade T1 disease. Herein, this review describes how to stratify high-grade T1 disease to predict progression and how to manage it properly by reducing over or under treatment.
Most bladder cancers are initially treated with TUR, and high-grade T1 disease is diagnosed from clinical specimens. Therefore, the role of urologists and pathologists is important for accurate diagnosis of high-grade T1. The outcome of TUR is highly variable depending on the skills of urologists [8]; thus an educational program is recommended for effective TUR. The extended TUR technique, which obtains additional specimens from the bottom of the tumor and grossly normal-appearing margin sites could improve the outcomes of TUR [9]. Bipolar equipment is an advantage of TUR because it appears to cause little tissue distortion and has the potential to facilitate the staging and grading of bladder tumors, although clinical outcomes are not different from those obtained with monopolar equipment [1011]. Photodynamic diagnosis or narrow-band imaging increases the sensitivity of cystoscopy, but whether it lowers the tumor recurrence rate is under debate [121314].
If patients are diagnosed with high-grade T1, a second TUR is strongly recommended regardless of the presence of muscle in specimens because of the possibility of understating due to incomplete resection [1516]. It provides more accurate pathological staging information, since persistent tumor in second TUR specimens can be detected in 33%-55% of patients [1718]. Even when muscle is seen in the initial TUR specimen, muscle invasion by urothelial cancer in the second TUR specimen can be detected in up to 10% of specimens [1920]. In addition, a second TUR promotes cancer control. In a randomized controlled study, a second TUR decreased the recurrence rate compared to a single TUR [21]. Further, residual tumor in the second TUR specimen is associated with poor prognosis. Of 92 patients with residual T1 cancer in second TURs, 75 (82%) progressed to muscle invasion within 5 years compared to 49 of 260 (19%) who had no or non-T1 tumor detected on restaging TUR [22]. The second TUR is recommended within 2 to 6 weeks after the initial resection. Because of the high incidence of carcinoma in situ (CIS) in the prostatic urethra or duct, biopsy from the prostatic urethra is recommended if tumor is located on the trigone or bladder neck [23].
Several studies proposed that, in the context of T1 disease, substaging based on depth or width of tumor infiltration affects clinical outcome (Fig. 1) [242526]. These studies suggested that T1 substaging is associated with progression and survival, and thus could have prognostic value. However, substaging has inherent pitfalls: pathological reports from TUR specimens are inconsistent because tissues are easily affected by electrical cautery. In fact, a recent validation study comparing two substaging systems could not reach statistical significance, although a trend toward a difference in progression and survival was observed during a follow-up period of 10 years [27]. For this reason, these systems are not widely used in clinical practice.
CIS is an important prognostic factor in high-grade T1 disease. The European Organization for Research and Treatment of Cancer investigated 194 high-grade T1 patients with a median follow-up of 3.9 years and suggested that the most important prognostic factor in patients with high-grade T1 tumors is the presence of concomitant CIS [3]. High-grade T1 patients without CIS had a probability of progression of 10% after 1 year and 29% after 5 years. By contrast, these rates for high-grade T1 patients with CIS were 29% and 74%, respectively. Denzinger et al. [28] also reported that CIS was associated with recurrence, progression, and cancer-specific survival in 132 high-grade T1 patients who received BCG induction therapy. Palou et al. [29] conducted a retrospective analysis of 146 patients with high-grade T1 detected in initial TUR over a median follow-up period of 8.7 years. None of the patients underwent a second TUR, and 44.5% of the patients had recurrence, 17.1% had progression, and 12.3% died of cancer. The authors suggested that female gender and the presence of CIS in the prostatic urethra were independent prognostic factors for progression and survival. Recently, Gontero et al. [30] carried out a retrospective study with 2,451 high-grade T1 patients from 23 centers, and suggested that age ≥70 years, tumor ≥3 cm, and concomitant CIS were the most important factors for progression.
Pathological outcomes from second TURs in patients with high-grade T1 are associated with prognosis. Herr et al. [22] conducted a study in a cohort of 352 patients with T1 on initial TUR, and compared progression according to pathological outcome on second TUR. Of the 92 patients with residual T1 cancer, 82% progressed to muscle invasion within 5 years compared to 19% of those who had no or non-T1 tumor detected on restaging TUR. Dalbagni et al. [31] performed a retrospective review of pathological outcomes from second TURs in 523 patients with T1 on initial TUR, and suggested that patients with T1 disease on restaging had a higher risk of progression; thus early cystectomy should be considered.
It is questionable whether the gene expression patterns of T1 with progression to MIBC on follow-up and those without progression are different from those of T2 cancer, since the gene expression patterns of T1 with progression at initial diagnosis should already show a T2 pattern. Therefore, we conducted unsupervised hierarchical clustering using 70 patients with T1 who did not experience progression, 10 T1 who experienced progression, and 26 with T2 disease (GSE 13507) [32]. The result was interesting. T1 patients without progression and T2 patients were relatively well categorized separately. However, 4 of 10 patients with T1 who experienced progression belonged to the T1 without progression cluster, whereas the other 6 of 10 belonged to the T2 cluster (Fig. 2) (data are not published). Interestingly, three of four patients with high-grade T1 who experienced progression were categorized as T2. This means that the gene expression patterns of high-grade T1 might already have MIBC characteristics at initial diagnosis. Similarly, Hurst et al. [33] performed an integrated genomic analysis of 49 high-grade T1 tumors. The authors investigated the copy number alteration and mutations in tumor tissues and suggested that the high-grade T1 tumors separated into three major subgroups and one minor subgroup, although they did not clearly describe whether these clusters were associated with progression or survival.
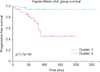
There are several reports indicating that molecular markers successfully predict the progression of NMIBC. Kim et al. [32] developed a clinically applicable quantitative real-time PCR gene signature to predict the progression of NMIBC. They undertook a microarray analysis of specimens derived from 103 primary NMIBC patients and identified an eight-gene progression-related classifier. The progressionrelated gene classifier in patients with NMIBC was closely correlated with progression in both the original cohort (165 patients) and an independent cohort (107 patients). Interestingly, no patient with NMIBC in the good-prognosis signature group experienced cancer progression. A further long-term validation study is in progress over a 10-year follow-up. An interim analysis showed that the molecular risk score could accurately predict the progression of NMIBC (Fig. 3) (data are not published). A similar study was carried out by Dyrskjot et al. [34]. The authors conducted a validation study of a gene expression signature designed to predict outcome in NMIBC, and suggested that the 88-gene progression classifier was highly significantly correlated with progression-free survival and cancer-specific survival. An interesting study was recently reported. Bartsch et al. [35] investigated whether a machine learning algorithm could predict the recurrence risk within 5 years after initial TUR using a molecular signature. They enrolled 112 patients with NMIBC in a study cohort and 83 in a validation cohort, and reported that a 3-gene rule was constructed that predicted recurrence with 80% sensitivity and 90% specificity in the study set, and 71% and 67%, respectively, in the validation set. Such a method could be applied to the decision-making for high-grade T1 management.
If patients with high-grade T1 disease have a low risk of progression, bladder sparing management should be considered. BCG instillation into bladder is the gold standard for conservative treatment for high-grade T1 disease. The therapeutic effect of BCG in high-grade T1 has already been established by several meta-analysis studies [43637]. However, we have to keep in mind that patients die upon progression to MIBC, not upon recurrence, and that the effectiveness of BCG at preventing progression was not as great as its effectiveness at preventing recurrence. In addition, BCG therapy may be associated with severe side effects with local or systemic symptoms. For that reason, the ability to predict the response to treatment before BCG instillation would be an invaluable tool in the selection of appropriate therapeutic modalities.
There are only a limited number of studies assessing prognostic and predictive factors in patients treated with BCG. A study by Kang et al. [38] examined the predictive value of glutathione S transferase mu (GSTM1) and theta polymorphisms in the early response to BCG induction therapy in patients with primary NMIBC. Patients carrying a GSTT1-positive genotype demonstrated a higher likelihood of early BCG failure, especially in the high-risk group (high-grade T1), where a GSTT1-positive genotype showed a 14-fold higher risk of early BCG failure compared to a GSTT1-null genotype. Predictive gene signatures may be a promising technique for assessing the response to intravesical BCG therapy, which may allow for the formulation of individualized therapeutic modalities. Until now, only one paper reported a gene signature that was able to predict BCG response and progression in primary T1 bladder cancer. Kim et al. [39] undertook a microarray analysis of specimens derived from 48 primary pT1 bladder cancer patients treated with BCG induction immunotherapy. Differentially expressed genes (12 for recurrence and 12 for progression) were the only independent predictors of recurrence (hazard ratio, 3.38; p=0.048) or progression (hazard ratio, 10.49; p=0.048).
Several studies focused on urinary changes in cytokines before or before/after vesical instillation for predicting BCG response. Zuiverloon et al. [40] conducted a systematic review of attempts to predict BCG response in high-risk bladder cancer and concluded that measurement of urinary interleukin (IL)-2 after BCG therapy seems to be the most potent predictor of BCG response. A similar study suggested that the ratio of urinary IL-6/IL-10 before BCG therapy could predict recurrence following BCG therapy in high-risk NMIBC [41]. A recent study suggested that a nomogram using the urinary levels of nine inducible cytokines (IL-2, IL-8, IL-6, IL-1ra, IL-10, IL-12, IL-12, TRAIL (tumor necrosis factor-related apoptosis-inducing ligand), and tumor necrosis factor-α) from before and after BCG instillation could predict the likelihood of recurrence with 85.5% accuracy in intermediate- and high-risk NMIBC patients [42]. However, it is not clear how urinary cytokines can predict BCG response, and using post-instillation urine is useless if we have to decide whether BCG therapy works or not for treating high-grade T1 disease.
Considering the high risk of progression and cancer death of high-grade T1 disease, cystectomy would be the best answer for treatment. However, there are disadvantages. First, cystectomy may be overtreatment for high-grade T1 disease. Since at least 50% of high-grade T1 patients are not upstaged upon cystectomy [434445], almost half undergo the surgery unnecessarily. Second, cystectomy deteriorates the quality of life. Although the incidence of continent orthotopic diversion has been increasing, many patients undergo incontinent diversion such as ileal conduit. Finally, cystectomy is a highly complicated surgery in the urological field, and almost 30%-50% of patients experience perioperative or long-term complications [4647].
On the other hand, cystectomy has definite advantages for high-grade T1 disease. In the largest study so far, the clinical outcomes of 167 patients with high-grade T1 were reviewed after cystectomy [44]. Surprisingly, almost 30% experienced disease recurrence, and 18.5% died from bladder cancer. 50% of the cases had disease upstaging, and 27.5% had extravesical disease. A greater than 3-month delay between cystectomy and last TUR showed a trend toward upstaging, which means that delaying cystectomy for BCG therapy may worsen prognosis. Several lines of evidence bolster the rationale for cystectomy in high-grade T1. Wiesner et al. [48] performed a retrospective review of 219 patients with NMIBC who underwent cystectomy, and suggested that the number of TURs and instances of tumor upstaging in cystectomy specimens correlated with an increased prevalence of lymph node metastasis. A similar study reported that early cystectomy seems to prolong cancer-specific survival compared to deferred cystectomy in high-risk high-grade T1 patients [45]. Given the vice and versa evidences of cystectomy, risk stratification is required for optimal treatment of high-grade T1 disease.
Kitamura and Kakehi [49] suggested that optimal management strategies should be based on pathological findings from second TUR specimens in patients with T1 disease. They recommended that patients with T0 upon second TUR be considered for BCG therapy or watchful waiting. A randomized controlled study is ongoing comparing watchful waiting to BCG therapy in high-grade T1 disease with T0 on second TUR [50]. In cases of Ta or T2 on second TUR, unarguably patients should undergo BCG therapy or cystectomy, respectively. In the case of T1 on second TUR, however, questions remain as to which treatment is the optimal treatment for high-grade T1 disease [51525354]. Such approaches are reasonable to select optimal treatment. However, if molecular risk classifiers for predicting progression or BCG response are included, it may help select treatment modalities for high-grade T1 patients, although they require validation in multiple large scale cohorts. Fig. 4 illustrates a proposed algorithm for treatment decision-making in high-grade T1 bladder cancer.
Patients with high-grade T1 bladder cancer show diverse clinical courses, with some highly associated with poor prognosis. In cases with low risk of progression, cystectomy may represent overtreatment and deteriorate quality of life irreversibly, while, in those with high risk, BCG therapy may worsen survival by delaying definitive therapy. There is currently no validated strategy to decide which treatment modality is optimal for each patient with high-grade T1. Current evidence suggests that clinico-pathological and molecular risk classifiers together may help select the optimal management course for each high-grade T1 patient.
Figures and Tables
Fig. 1
T1 disease substaging systems based on depth or width of tumor infiltration. T1a, invasion above muscularis mucosae; T1b, invasion within muscularis mucosae; T1c, invasion below muscularis mucosae; T1m, a single focus of lamina propria invasion ≤0.5 mm; T1e, specimens showing >0.5 mm lamina propria invasion or multiple invasions.

Fig. 2
Unsupervised hierarchical clustering using 70 patients with T1 who did not experience progression, 10 patients with T1 who experienced progression, and 26 patients with T2 disease (GSE 13507). Interestingly, three of four patients with high-grade T1 who experienced progression were categorized as T2. This means that high-grade T1 gene expression patterns might already have muscle invasive bladder cancer characteristics at initial diagnosis. (A) Heatmap from microarray data. (B) Clustering with clinico-pathological variables. HG, high-grade.

ACKNOWLEDGMENTS
This work was supported by a research grant from Chungbuk National University in 2014.
References
1. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–450.
2. Song W, Jeon HG. Incidence of kidney, bladder, and prostate cancers in Korea: An update. Korean J Urol. 2015; 56:422–428.
3. Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006; 49:466–477.
4. Sylvester RJ, van der Meijden AP, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol. 2002; 168:1964–1970.
5. Malmström PU, Sylvester RJ, Crawford DE, Friedrich M, Krege S, Rintala E, et al. An individual patient data meta-analysis of the long-term outcome of randomised studies comparing intravesical mitomycin C versus bacillus Calmette-Guérin for non-muscle-invasive bladder cancer. Eur Urol. 2009; 56:247–256.
6. Kulkarni GS, Hakenberg OW, Gschwend JE, Thalmann G, Kassouf W, Kamat A, et al. An updated critical analysis of the treatment strategy for newly diagnosed high-grade T1 (previously T1G3) bladder cancer. Eur Urol. 2010; 57:60–70.
7. van den Bosch S, Alfred Witjes J. Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: a systematic review. Eur Urol. 2011; 60:493–500.
8. Mariappan P, Finney SM, Head E, Somani BK, Zachou A, Smith G, et al. Good quality white-light transurethral resection of bladder tumours (GQ-WLTURBT) with experienced surgeons performing complete resections and obtaining detrusor muscle reduces early recurrence in new non-muscle-invasive bladder cancer: validation across time and place and recommendation for benchmarking. BJU Int. 2012; 109:1666–1673.
9. Richterstetter M, Wullich B, Amann K, Haeberle L, Engehausen DG, Goebell PJ, et al. The value of extended transurethral resection of bladder tumour (TURBT) in the treatment of bladder cancer. BJU Int. 2012; 110(2 Pt 2):E76–E79.
10. Mashni J, Godoy G, Haarer C, Dalbagni G, Reuter VE, Al-Ahmadie H, et al. Prospective evaluation of plasma kinetic bipolar resection of bladder cancer: comparison to monopolar resection and pathologic findings. Int Urol Nephrol. 2014; 46:1699–1705.
11. Venkatramani V, Panda A, Manojkumar R, Kekre NS. Monopolar versus bipolar transurethral resection of bladder tumors: a single center, parallel arm, randomized, controlled trial. J Urol. 2014; 191:1703–1707.
12. Schumacher MC, Holmang S, Davidsson T, Friedrich B, Pedersen J, Wiklund NP. Transurethral resection of non-muscle-invasive bladder transitional cell cancers with or without 5-aminolevulinic Acid under visible and fluorescent light: results of a prospective, randomised, multicentre study. Eur Urol. 2010; 57:293–299.
13. Stenzl A, Penkoff H, Dajc-Sommerer E, Zumbraegel A, Hoeltl L, Scholz M, et al. Detection and clinical outcome of urinary bladder cancer with 5-aminolevulinic acid-induced fluorescence cystoscopy : A multicenter randomized, double-blind, placebo-controlled trial. Cancer. 2011; 117:938–947.
14. Herr HW. Randomized trial of narrow-band versus white-light cystoscopy for restaging (second-look) transurethral resection of bladder tumors. Eur Urol. 2015; 67:605–608.
15. Ramírez-Backhaus M, Dominguez-Escrig J, Collado A, Rubio-Briones J, Solsona E. Restaging transurethral resection of bladder tumor for high-risk stage Ta and T1 bladder cancer. Curr Urol Rep. 2012; 13:109–114.
16. Shim JS, Choi H, Noh TI, Tae JH, Yoon SG, Kang SH, et al. The clinical significance of a second transurethral resection for T1 high-grade bladder cancer: Results of a prospective study. Korean J Urol. 2015; 56:429–434.
17. Jahnson S, Wiklund F, Duchek M, Mestad O, Rintala E, Hellsten S, et al. Results of second-look resection after primary resection of T1 tumour of the urinary bladder. Scand J Urol Nephrol. 2005; 39:206–210.
18. Vasdev N, Dominguez-Escrig J, Paez E, Johnson MI, Durkan GC, Thorpe AC. The impact of early re-resection in patients with pT1 high-grade non-muscle invasive bladder cancer. Ecancermedicalscience. 2012; 6:269.
19. Miladi M, Peyromaure M, Zerbib M, Saighi D, Debre B. The value of a second transurethral resection in evaluating patients with bladder tumours. Eur Urol. 2003; 43:241–245.
20. Schwaibold HE, Sivalingam S, May F, Hartung R. The value of a second transurethral resection for T1 bladder cancer. BJU Int. 2006; 97:1199–1201.
21. Kim W, Song C, Park S, Kim J, Park J, Kim SC, et al. Value of immediate second resection of the tumor bed to improve the effectiveness of transurethral resection of bladder tumor. J Endourol. 2012; 26:1059–1064.
22. Herr HW, Donat SM, Dalbagni G. Can restaging transurethral resection of T1 bladder cancer select patients for immediate cystectomy? J Urol. 2007; 177:75–79.
23. Mungan MU, Canda AE, Tuzel E, Yorukoglu K, Kirkali Z. Risk factors for mucosal prostatic urethral involvement in superficial transitional cell carcinoma of the bladder. Eur Urol. 2005; 48:760–763.
24. Platz CE, Cohen MB, Jones MP, Olson DB, Lynch CF. Is microstaging of early invasive cancer of the urinary bladder possible or useful? Mod Pathol. 1996; 9:1035–1039.
25. Smits G, Schaafsma E, Kiemeney L, Caris C, Debruyne F, Witjes JA. Microstaging of pT1 transitional cell carcinoma of the bladder: identification of subgroups with distinct risks of progression. Urology. 1998; 52:1009–1013.
26. van Rhijn BW, van der Kwast TH, Alkhateeb SS, Fleshner NE, van Leenders GJ, Bostrom PJ, et al. A new and highly prognostic system to discern T1 bladder cancer substage. Eur Urol. 2012; 61:378–384.
27. DE Marco V, Cerruto MA, D'Elia C, Brunelli M, Otte O, Minja A, et al. Prognostic role of substaging in T1G3 transitional cell carcinoma of the urinary bladder. Mol Clin Oncol. 2014; 2:575–580.
28. Denzinger S, Otto W, Fritsche HM, Roessler W, Wieland WF, Hartmann A, et al. Bladder sparing approach for initial T1G3 bladder cancer: Do multifocality, size of tumor or concomitant carcinoma in situ matter? A long-term analysis of 132 patients. Int J Urol. 2007; 14:995–999.
29. Palou J, Sylvester RJ, Faba OR, Parada R, Peña JA, Algaba F, et al. Female gender and carcinoma in situ in the prostatic urethra are prognostic factors for recurrence, progression, and disease-specific mortality in T1G3 bladder cancer patients treated with bacillus Calmette-Guérin. Eur Urol. 2012; 62:118–125.
30. Gontero P, Sylvester R, Pisano F, Joniau S, Vander Eeckt K, Serretta V, et al. Prognostic factors and risk groups in T1G3 non-muscle-invasive bladder cancer patients initially treated with Bacillus Calmette-Guérin: results of a retrospective multicenter study of 2451 patients. Eur Urol. 2015; 67:74–82.
31. Dalbagni G, Vora K, Kaag M, Cronin A, Bochner B, Donat SM, et al. Clinical outcome in a contemporary series of restaged patients with clinical T1 bladder cancer. Eur Urol. 2009; 56:903–910.
32. Kim WJ, Kim EJ, Kim SK, Kim YJ, Ha YS, Jeong P, et al. Predictive value of progression-related gene classifier in primary non-muscle invasive bladder cancer. Mol Cancer. 2010; 9:3.
33. Hurst CD, Platt FM, Taylor CF, Knowles MA. Novel tumor subgroups of urothelial carcinoma of the bladder defined by integrated genomic analysis. Clin Cancer Res. 2012; 18:5865–5877.
34. Dyrskjot L, Zieger K, Real FX, Malats N, Carrato A, Hurst C, et al. Gene expression signatures predict outcome in non-muscleinvasive bladder carcinoma: a multicenter validation study. Clin Cancer Res. 2007; 13:3545–3551.
35. Bartsch G Jr, Mitra AP, Mitra SA, Almal AA, Steven KE, Skinner DG, et al. Use of artificial intelligence and machine learning algorithms with gene expression profiling to predict recurrent nonmuscle invasive urothelial carcinoma of the bladder. J Urol. 2016; 195:493–498.
36. Shelley MD, Wilt TJ, Court J, Coles B, Kynaston H, Mason MD. Intravesical bacillus Calmette-Guérin is superior to mitomycin C in reducing tumour recurrence in high-risk superficial bladder cancer: a meta-analysis of randomized trials. BJU Int. 2004; 93:485–490.
37. Böhle A, Bock PR. Intravesical bacille Calmette-Guérin versus mitomycin C in superficial bladder cancer: formal meta-analysis of comparative studies on tumor progression. Urology. 2004; 63:682–686.
38. Kang HW, Tchey DU, Yan C, Kim WT, Kim YJ, Yun SJ, et al. The predictive value of GSTT1 polymorphisms in predicting the early response to induction BCG therapy in patients with non-muscle invasive bladder cancer. Urol Oncol. 2014; 32:458–465.
39. Kim YJ, Ha YS, Kim SK, Yoon HY, Lym MS, Kim MJ, et al. Gene signatures for the prediction of response to Bacillus Calmette-Guerin immunotherapy in primary pT1 bladder cancers. Clin Cancer Res. 2010; 16:2131–2137.
40. Zuiverloon TC, Nieuweboer AJ, Vekony H, Kirkels WJ, Bangma CH, Zwarthoff EC. Markers predicting response to bacillus Calmette-Guérin immunotherapy in high-risk bladder cancer patients: a systematic review. Eur Urol. 2012; 61:128–145.
41. Cai T, Nesi G, Mazzoli S, Meacci F, Tinacci G, Luciani LG, et al. Prediction of response to bacillus Calmette-Guérin treatment in non-muscle invasive bladder cancer patients through interleukin-6 and interleukin-10 ratio. Exp Ther Med. 2012; 4:459–464.
42. Kamat AM, Briggman J, Urbauer DL, Svatek R, Nogueras Gonzalez GM, Anderson R, et al. Cytokine Panel for Response to Intravesical Therapy (CyPRIT): nomogram of changes in urinary cytokine levels predicts patient response to bacillus Calmette-Guérin. Eur Urol. 2016; 69:197–200.
43. Lambert EH, Pierorazio PM, Olsson CA, Benson MC, McKiernan JM, Poon S. The increasing use of intravesical therapies for stage T1 bladder cancer coincides with decreasing survival after cystectomy. BJU Int. 2007; 100:33–36.
44. Gupta A, Lotan Y, Bastian PJ, Palapattu GS, Karakiewicz PI, Raj GV, et al. Outcomes of patients with clinical T1 grade 3 urothelial cell bladder carcinoma treated with radical cystectomy. Urology. 2008; 71:302–307.
45. Denzinger S, Fritsche HM, Otto W, Blana A, Wieland WF, Burger M. Early versus deferred cystectomy for initial high-risk pT1G3 urothelial carcinoma of the bladder: do risk factors define feasibility of bladder-sparing approach? Eur Urol. 2008; 53:146–152.
46. Hautmann RE, de Petriconi RC, Volkmer BG. Lessons learned from 1,000 neobladders: the 90-day complication rate. J Urol. 2010; 184:990–994.
47. Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH, Holm HV, et al. ICUD-EAU International Consultation on Bladder Cancer 2012: Urinary diversion. Eur Urol. 2013; 63:67–80.
48. Wiesner C, Pfitzenmaier J, Faldum A, Gillitzer R, Melchior SW, Thüroff JW. Lymph node metastases in non-muscle invasive bladder cancer are correlated with the number of transurethral resections and tumour upstaging at radical cystectomy. BJU Int. 2005; 95:301–305.
49. Kitamura H, Kakehi Y. Treatment and management of high-grade T1 bladder cancer: what should we do after second TUR? Jpn J Clin Oncol. 2015; 45:315–322.
50. Kunieda F, Kitamura H, Niwakawa M, Kuroiwa K, Shinohara N, Tobisu K, et al. Watchful waiting versus intravesical BCG therapy for high-grade pT1 bladder cancer with pT0 histology after second transurethral resection: Japan Clinical Oncology Group Study JCOG1019. Jpn J Clin Oncol. 2012; 42:1094–1098.
51. Hautmann RE, Volkmer BG, Gust K. Quantification of the survival benefit of early versus deferred cystectomy in high-risk non-muscle invasive bladder cancer (T1 G3). World J Urol. 2009; 27:347–351.
52. Jager W, Thomas C, Haag S, Hampel C, Salzer A, Thuroff JW, et al. Early vs delayed radical cystectomy for high-risk carcinoma not invading bladder muscle: delay of cystectomy reduces cancer-specific survival. BJU Int. 2011; 108(8 Pt 2):E284–E288.
53. Badalato GM, Gaya JM, Hruby G, Patel T, Kates M, Sadeghi N, et al. Immediate radical cystectomy vs conservative management for high grade cT1 bladder cancer: is there a survival difference? BJU Int. 2012; 110:1471–1477.
54. Sternberg IA, Keren Paz GE, Chen LY, Herr HW, Dalbagni G. Role of immediate radical cystectomy in the treatment of patients with residual T1 bladder cancer on restaging transurethral resection. BJU Int. 2013; 112:54–59.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download