Abstract
In pursuit of continuing medical education in robotic surgery, several forms of training have been implemented. This variable application of curriculum has brought acquisition of skills in a heterogeneous and unstandardized fashion from different parts of the world. Recently, efforts have been made to provide cost effective and well-structured curricula with the aim of bridging the gap between formal fellowship training and short courses. Proctorship training has been implicated on some curriculum to provide excellent progression during the learning curve while ensuring patient safety.
Robotic Surgery has taken a critical role in management of different diseases and is now gaining popularity across different specialties. Recent data showed that Da Vinci Surgical System has increased its revenue over 14% this year from 2015 [1]. From its commencement, it has gained popularity with some drawbacks because of its cost-effectiveness [234]. This increase in number and availability of robotic system has become advantageous to laparoscopy naive surgeons to immediately access minimally invasive procedures. However, transferring from open to robotic surgery has profound learning curve even among experienced laparoscopic surgeons. In effect, this has lead postgraduate urologist to seek different forms of training in robotic surgery.
Ever since its introduction, continuous efforts have been made in order to standardize training of urologists and surgeons in general, who use robotic platform. Rampant efforts have been placed in order to come up with reproducible and simple training curriculum [5]. As development of surgical techniques evolves, urologists are also obliged to have a safe and organized acquisition of skills. Thus, surgical programs should be safe, cost-effective, and transferrable to real clinical scenario. This has led to a greater demand for mentoring of inexperienced surgeons [6]. During the introduction of laparoscopic surgery, mini residency and proctorship programs have been employed. This provided postgraduate urologist to venture into laparoscopic surgery with ease. Learning new surgical concept using a mini-fellowship model has been a safe process of disseminating laparoscopic surgery among surgeons. In the same manner, effective surgical education is the goal of all programs to provide competency in robotic surgery. Nevertheless, several surgical societies and surgeons have promoted the need for a standardized approach for basic training, assessment, testing, and certification in robotic surgery [7].
We aim to present the framework of surgical curriculum, mentoring, and proctorship in robotic surgery.
Training for robotic techniques has been variable from one place to another. Therefore, credentials have also the same effect of nonuniformity among different centers. Efforts have been made to develop a robotic surgery curriculum to attain uniformity among different institutions. Several governing bodies for development have made preclinical exposure and validated tools for assessment of surgeons' proficiency [7]. Unlike laparoscopy, robotic training lacks evidence-based validated program like Fundamentals of Laparoscopic Surgery (FLS) course that has been widely used across nations. This course introduced by Society of Gastrointestinal and Endoscopic Surgeons [8] have been the reference point of different groups in trying to come up with new curriculum for robotic trainees. However, FLS does not actually include basic and specific training for robotic surgery. Validation of surgical curriculum has been one of the greatest hindrances in robotics because of the absence of gold standard assessment tool. On the other hand, Global Evaluative Assessment of Robotic Skills has been recently introduced, which is aimed to validate training tools in order to standardize every program [9]. Moreover all surgical curricula are aimed towards one goal, which is safe and cost-effective acquisition of robotic skills (Fig. 1).
In the recent years, Fundamentals of Robotic Surgery (FRS) was developed by expert surgeons [10] which was made from proficiency-based training and was based on 2 groups; Florida Hospital Nicholson Center and the Orlando group [11]. The former was made up of a series of consensus from different surgical specialties. On the other hand, the latter is a model based on five-simulated tasks; camera targeting, peg board, ring walk, energy dissection, and suture sponge, based on skill simulator for Da Vinci Si. This FRS model now serves as the template in the development of core basic skills template applicable for their own specialty. Presently, this model is undergoing stages of validation.
Another curriculum is Fundamental Skills of Robotic Surgery (FSRS), which is introduced by a team based in Roswell Cancer Institute, Buffalo, NY. It is a simulation-based course developed by group of expert robotic surgeons and has been assessed and validated using Robotic Skills Assessment Score (RSA) [12]. This course uses a scoring system to measure robotic skills of trainee using RSA that was validated between expert and nonexpert surgeons. Likewise, FSRS has gained validation and proven to show significant improvement of experimental group [13]. As a result, this group of expert surgeons has formally introduced Robotic Assisted Surgical Training program. It is based on the FSRS curriculum with hands on tasks and is designed to be completed by participants between 5 days and 3 weeks. This has gained acceptance among trainees and proved to have influenced on their surgical education and been widely applied in their respective centers.
Moreover, European Association of Urology Robotic Section has come up with a new curriculum from congress meetings of EAU Robotic Urology Section (ERUS) [14]. This model provides a training module, simulation and observation in a mixed setting of dry lab, wet lab, and virtual reality for trainees. It also entails table assistance and eventually procedural steps with a mentor in a dual console. Interestingly, this course has shown significant improvement in robotic skills in its infancy validation stage [15]. Incorporation of mentorship has made this unique over other curricula. Meanwhile, a multidisciplinary basic skills training which also consist of lectures and modules is being offered in the University of Toronto. However, unlike ERUS it is not tailored to any specific specialty but rather provides generic surgical robotic skills [16]. It is also a simulation based curricula which has not incorporated operating room training and proctorship.
Proficiency based curriculum was introduced by a group from the University of Texas Southwestern Medical Center. It is comprised of inanimate tasks, online didactics and a half-day tutorial [11]. The course takes 2 months to complete and the 9 tasks are expected to be performed by trainees until they reach suitable levels of proficiency. It has also been validated among different groups who found this course to be highly relevant for surgical training [17]. One of its advantages is the assurance of proficiency for all surgeon learners.
Robotics and computer sciences have innovated ways to enhance surgeon's skills and achieve an early competency. Virtual reality exercises have been employed such as da Vinci Skills Simulator (Intuitive Surgical Inc., Sunnyvale, CA, USA), as well as corresponding dry lab versions of each exercise (Mimic Technologies, Seattle, WA, USA) to hasten the old apprenticeship training. These tools have shown to be feasible and compliant with global assessment tools even in the setting of dry lab exercises [18]. It has allowed trainees to fine tune their technical skills without compromising patients' safety. Furthermore, due to the widespread use of robotic technology, it has become essential to combine clinical training with simulation to facilitate rapid skill acquisition among trainees. These simulators have provided surgeons an acceptable progression along the initial learning curve.
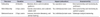
Every curriculum has its own advantages (Table 1). FSRS has the potential to be used in different applications and future simulators with a commendable psychomotor development. Strengths of each curriculum should rather be considered in creating specific training for specialties or procedures. Moreover, reality in cost effectiveness [3] should also be considered in every training curriculum. Some centers may not be able to provide an extra robot for training new surgeons, which would limit the access for training. Based on the abovementioned curricula, not all programs have incorporated proctorship among their training. To the very least, ERUS is the only course which had incorporated a fellowship-style mentorship from a dual console. ERUS versatility and provision of structured proctorship in the form of mini-fellowship has been one of its advantages over other existing curriculum [15]. This varied training is ideal for trainees as it gives them a broad experience in robotics before actual clinical use. By way of incorporating proctorship, it allows urologists to embark on robotic surgery with more safety, efficiency and confidence during the initial learning curve.
A formal fellowship is considered as one of the most structured form of proctorship, mentoring and training program. Most of the programs are modular based [19] and has been proven to have a beneficial educational impact. Its objective is to develop a systematic teaching method, which is reproducible. Guided learning has always been part of fellowship wherein trainees perform progressive steps of the operation under careful guidance of an instructor with constant and immediate feedback. It has long been believed that guided learning lead to improved proficiency in operative techniques. It reinforces the flow of operation by direct and immediate guidance from the attending surgeon to the trainee. In turn, this translates into a safer and effective way of surgical education. With the aim of further standardization, very recently Hung et al. [20] reported improvements in training from a structured learning program in robotic surgery using proficiency scores. This has boosted the confidence of trainees' robotic skills. As a result, they have now adopted the use of this quantitative feedback based on proficiency scores.
Another form of mentorship is a mini-fellowship. It has previously proven to have a high take rate [21] and has allowed postgraduate urologist to operate safely and independently with excellent progress across their initial learning curve. Notably, mini-fellowship programs have been more profoundly helpful among partner surgeons who took the course together rather than those who did not [22]. This effect explains its high take rate among attendees. Perhaps, it may have a subjective sense of trust between console surgeon and his bedside assistant as both were trained in the same way. Most urologists prefer this option, since it requires only a short amount of time, while training is intensive. This would allow them to immediately adapt it into their own clinical practice. However, progression of skills after training may still be questionable particularly among low caseload surgeons.
In 2011, Patel et al. [23] reported that a mentored course which entails lectures, standardized laboratory training with videotape analysis, and a mentored porcine training benefited their attendees in transition to robotic surgery. Their result showed that the mentored animal laboratory course was the most beneficial among the trainees. Even in the era of laparoscopic training, mutual mentoring has been proven to be an effective way of learning [24]. It is on this form of short course, a postgraduate urologist naïve of robotic skill can easily acquire new skills without compromising patients' safety. In the same manner as mini-fellowship, it offers short duration training at a lower cost.
On the other hand, Kwon et al. [25] reported that proctorship program has provided efficiency and rapid progression of learning curve among surgeons. They described it as a rotational form of participation in the operation when one takes the role of console surgeon while the other acts like a proctor. In their program, they reported acceptable 8% complication rates comparable to what is reported in the literature and an average prostatectomy time of 2 hours in their first 100 patients, which were better than expected for an initial series. There have been continuing demands for improvement of acquisition of robotic skills. Moreover, an extended proctorship has been implemented by a group of urologists. They have found this to be beneficial with increased take rate and reduced learning curve with a score of 4.2 in 5-point Likert scale among participants [26]. Provision of proctorship has made trainees achieve earlier performance of independent robotic cases. This has allowed a conduction of safe surgery with the proctor guiding the trainee throughout the procedure during his early learning curve cases. As previously mentioned, formal fellowship training is considered the most structured form of proctorship and mentoring. Amidst longer duration, it provides more number of cases, postoperative management of complex cases and even progression to advanced skills which one may not attain from other forms like mini-fellowship and mentored courses. Common lines are always present between proctorship and mentorship and are often used interchangeably. However, in any form it is always aimed to provide the acquisition of robotic skills that are safe and reproducible. With the aim of achieving better interaction between robotic trainee and proctor, technological advancements such as 3-dimensional (3D) hands and instruments for telestration have been added to proctorship armamentarium [27]. All of which has its own advantages and disadvantages from the perspective of cost, duration and actual acquisition and application of robotic skills (Table 2). Successful training programs have allowed progressive interaction and involvement of surgeon teacher and learners. During early years of robotic training, proctoring environment has been difficult due to 1 surgeon and 1 console. Since the release of the dual-console of da Vinci Si Surgical System, more suitable proctoring environment has been made available for proctors as well as trainees (Fig. 2). This modality of proctorship has provided a safe method of proctoring without prolonging the operative time and compromising patient safety [28]. Likewise, the future looks promising for mentoring and proctorship as technology has emerged to facilitate telementoring thereby facilitating proctorship and mentoring from a remote place [29].
Proctoring has been used to hasten the steep learning curve one may encounter in acquiring robotic skill. Proctors and mentors play an important role in certifying one's competency in robotic skills. Unfortunately, there is no standardized rule in certifying a surgeon to become a proctor. To the very least, a urologist can be proctor to other surgeon if he has successfully performed 20 independent robotic surgery cases [7].
Legal dilemmas have always been a challenge among proctor and mentor surgeons.
There is no clear implication whether a proctor is liable over an impending eventuality of serious complications. Courts have put trainee surgeon the sole responsible party on this case. Nevertheless, proper explanation of surgeon trainee and proctor role should be clearly discussed with the patient prior to surgical consent to avoid any possibility of legal precedents [30]. However, it is not routinely practiced especially in robotic cases. Most guidelines recommend a proctor to intervene if the patient's well-being is in danger. However, doctor-patient relationship only exists between the patient and surgeon trainee. As a result, proctors are not held liable on this scenario. For rare instances that a proctor has intervened over a trainee in an emergency situation, legal implications still remain unclear. In emergency cases, converting robotic surgery to open is the safest and most effective way to alleviate legal burden on the proctor but rather the trainee takes hold of the full responsibility. Aside from the legal implications, time and financial constrains maybe another form of limiting factor for success of program which entails proctorship [31]. Another factor is lack of availability of simple cases in centers where the surgeon trainee would commence his robotic clinical application. These shortcomings need to be better addressed to avoid any medicolegal implications in the future and, ultimately, to provide optimal patient safety and care.
Robotic training still lacks uniformity and proper standardization but is on its way to build strong foundation programs. Undeniably, competence and skill acquisition is still variable across the world. Several organization and group of expert robotic surgeons are paving the way towards a cost-effective, valid, and safe curriculum for robotic training. This would ensure future urologist a proper grasp of education and skills to safely apply robotic technology on their patients. Fellowship training remains the strongest form of acquisition of robotic surgical skills due to its direct proctorship and more caseloads. At present stage, proctorship remains a viable option for postgraduate urologist to safely venture their learning curve in robotic surgery short of a formal fellowship. Though fundamental curriculum is at its infancy and adaptation has a promising early result, proctorship incorporation on its course may still be of value. Moreover, future developments in technology have made proctorship more promising using 3D hands and a possibility of telementoring. All of these structural developments and aids are essential and necessary in providing new skills to surgeons to integrate robotic surgery to provide optimal care for their patients.
Figures and Tables
Table 1
Advantages and disadvantages of each curriculum

Table 2
Comparison of robotic surgical acquisition by proctorship and mentoring
References
1. Da Vinci Surgical System [Internet]. Sunnyvale (CA): Intuitive Surgical Inc.;c2016. cited 2016 Jul 30. Available from: http://www.intuitivesurgical.com.
2. Seo IY. Urologic robotic surgery in Korea: past and present. Korean J Urol. 2015; 56:546–552.
3. Kim DK, Rha KH. Supporting evidence for robotic urological surgery. Korean J Urol. 2015; 56:733–734.
4. Nishimura K. Current status of robotic surgery in Japan. Korean J Urol. 2015; 56:170–178.
5. Fisher RA, Dasgupta P, Mottrie A, Volpe A, Khan MS, Challacombe B, et al. An over-view of robot assisted surgery curricula and the status of their validation. Int J Surg. 2015; 13:115–123.
6. Marguet CG, Young MD, L'Esperance JO, Tan YH, Ekeruo WO, Preminger GM, et al. Hand assisted laparoscopic training for postgraduate urologists: the role of mentoring. J Urol. 2004; 172:286–289.
7. Zorn KC, Gautam G, Shalhav AL, Clayman RV, Ahlering TE, Albala DM, et al. Training, credentialing, proctoring and medicolegal risks of robotic urological surgery: recommendations of the society of urologic robotic surgeons. J Urol. 2009; 182:1126–1132.
8. Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, et al. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery. 2004; 135:21–27.
9. Hung AJ, Jayaratna IS, Teruya K, Desai MM, Gill IS, Goh AC. Comparative assessment of three standardized robotic surgery training methods. BJU Int. 2013; 112:864–871.
10. Smith R, Patel V, Satava R. Fundamentals of robotic surgery: a course of basic robotic surgery skills based upon a 14-society consensus template of outcomes measures and curriculum development. Int J Med Robot. 2014; 10:379–384.
11. Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, et al. Developing a comprehensive, proficiency-based training program for robotic surgery. Surgery. 2012; 152:477–488.
12. Chowriappa AJ, Shi Y, Raza SJ, Ahmed K, Stegemann A, Wilding G, et al. Development and validation of a composite scoring system for robot-assisted surgical training--the Robotic Skills Assessment Score. J Surg Res. 2013; 185:561–569.
13. Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, et al. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013; 81:767–774.
14. Ahmed K, Khan R, Mottrie A, Lovegrove C, Abaza R, Ahlawat R, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015; 116:93–101.
15. Volpe A, Ahmed K, Dasgupta P, Ficarra V, Novara G, van der Poel H, et al. Pilot Validation study of the European Association of Urology Robotic Training Curriculum. Eur Urol. 2015; 68:292–299.
16. Foell K, Finelli A, Yasufuku K, Bernardini MQ, Waddell TK, Pace KT, et al. Robotic surgery basic skills training: Evaluation of a pilot multidisciplinary simulation-based curriculum. Can Urol Assoc J. 2013; 7:430–434.
17. Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KK, Tesfay ST, Scott DJ. Content and face validity of a comprehensive robotic skills training program for general surgery, urology, and gynecology. Am J Surg. 2012; 203:535–539.
18. Ramos P, Montez J, Tripp A, Ng CK, Gill IS, Hung AJ. Face, content, construct and concurrent validity of dry laboratory exercises for robotic training using a global assessment tool. BJU Int. 2014; 113:836–842.
19. Rashid HH, Leung YY, Rashid MJ, Oleyourryk G, Valvo JR, Eichel L. Robotic surgical education: a systematic approach to training urology residents to perform robotic-assisted laparoscopic radical prostatectomy. Urology. 2006; 68:75–79.
20. Hung AJ, Bottyan T, Clifford TG, Serang S, Nakhoda ZK, Shah SH, et al. Structured learning for robotic surgery utilizing a proficiency score: a pilot study. World J Urol. 2016; 04. 22. [Epub]. DOI: 10.1007/s00345-016-1833-3.
21. McDougall EM, Corica FA, Chou DS, Abdelshehid CS, Uribe CA, Stoliar G, et al. Short-term impact of a robot-assisted laparoscopic prostatectomy 'mini-residency' experience on postgraduate urologists' practice patterns. Int J Med Robot. 2006; 2:70–74.
22. Gamboa AJ, Santos RT, Sargent ER, Louie MK, Box GN, Sohn KH, et al. Long-term impact of a robot assisted laparoscopic prostatectomy mini fellowship training program on postgraduate urological practice patterns. J Urol. 2009; 181:778–782.
23. Patel SR, Hedican SP, Bishoff JT, Shichman SJ, Link RE, Wolf JS Jr, et al. Skill based mentored laparoscopy course participation leads to laparoscopic practice expansion and assists in transition to robotic surgery. J Urol. 2011; 186:1997–2000.
24. Jones A, Eden C, Sullivan ME. Mutual mentoring in laparoscopic urology - a natural progression from laparoscopic fellowship. Ann R Coll Surg Engl. 2007; 89:422–425.
25. Kwon EO, Bautista TC, Blumberg JM, Jung H, Tamaddon K, Aboseif SR, et al. Rapid implementation of a robot-assisted prostatectomy program in a large health maintenance organization setting. J Endourol. 2010; 24:461–465.
26. Mirheydar H, Jones M, Koeneman KS, Sweet RM. Robotic surgical education: a collaborative approach to training postgraduate urologists and endourology fellows. JSLS. 2009; 13:287–292.
27. Jarc AM, Shah SH, Adebar T, Hwang E, Aron M, Gill IS, et al. Beyond 2D telestration: an evaluation of novel proctoring tools for robot-assisted minimally invasive surgery. J Robot Surg. 2016; 10:103–109.
28. Smith AL, Scott EM, Krivak TC, Olawaiye AB, Chu T, Richard SD. Dual-console robotic surgery: a new teaching paradigm. J Robot Surg. 2013; 7:113–118.
29. Santomauro M, Reina GA, Stroup SP, L'Esperance JO. Telementoring in robotic surgery. Curr Opin Urol. 2013; 23:141–145.
30. Livingston EH, Harwell JD. The medicolegal aspects of proctoring. Am J Surg. 2002; 184:26–30.
31. Birch DW, Asiri AH, de Gara CJ. The impact of a formal mentoring program for minimally invasive surgery on surgeon practice and patient outcomes. Am J Surg. 2007; 193:589–591.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download