Abstract
Purpose
High serum inorganic phosphorus level is related with atherosclerosis and an elevated risk of cardiovascular disease. At the same time, the association of phosphorus with erectile dysfunction (ED) is not well reported. We studied the effect of serum phosphorus on ED and the relationship with other clinical variables.
Materials and Methods
From March to September 2013, 1,899 police men aged 40 to 59 years who entered in a prostate health screening were targeted. All subjects underwent a clinical checking using the International Index of Erectile Function-5 (IIEF-5) questionnaire translated into Korean. Serum prostate-specific antigen (PSA), testosterone, inorganic phosphorus, body mass index, metabolic syndrome (MetS), and prostate ultrasound were also examined.
Results
Serum inorganic phosphorus (r=–0.108, p<0.001) had the highest correlation coefficient with IIEF-5 score other than age, followed by prostate volume (PV) (r=–0.065, P<0.001). Using logistic regression analysis, age, phosphorus, and MetS were predictive factors for moderate to severe ED in univariate analysis. PSA, testosterone, body mass index, and PV could not predict ED. Age, MetS, and phosphorus were independent predictive factors of moderate to severe ED (p<0.001; odds ratio [OR], 1.119; 95% confidence interval [CI] 1.086–1.153; p=0.048; OR, 1.283; 95% CI, 1.003–1.641; and p=0.048; OR, 1.101; 95% CI, 1.076–1.131) in the multivariate analysis.
Phosphorus is necessary for several, various biological roles in the signal transduction of cells and energy exchange of human body. About 80%–90% of phosphorus is founded in teeth and bones. Mineral balance is regulated by a complex interaction between gastrointestinal absorption, renal excretion and translocation between parts of the human body. The latter process is important during the fast changes of metabolism [12]. Impaired intestinal phosphate absorption, renal phosphate reabsorption, and phosphate metabolism can elevate serum phosphorus level [3]. Elevated serum phosphorus is suspected to elevate the risk of cardiovascular disease (CVD) through vascular calcification, myocardial fibrosis, and development of left ventricular hypertrophy [456].
Erectile dysfunction (ED) is a frequent problem that affects about 15% of men 40 to 50 years of age, 45% of men in their 60s, and 70% of men older than 70 [7]. In addition to being a distressing condition itself, ED is thought to be a harbinger of CVD and mortality. Organic ED and coronary artery disease (CAD) are closely related, as endothelial dysfunction leads to a restriction of blood flow [89]. ED and CVD share many common risk factors, such as age, hypertension, insulin resistance, increased body mass index (BMI), cholesterol, lower levels of high-density lipoprotein, and smoking [1011121314]. Overall atherosclerotic processes affect arterial blood flow and lead to major pathophysiologic changes that contribute to both cardiovascular and peripheral vascular diseases, including ED [15]. There is a growing body of evidence that ED is a sentinel marker of subclinical CVD and likely precedes symptomatic CAD.
In light of these observations, we assessed whether serum phosphorus is associated with erectile function in middle-aged Korean men.
The proposal of our research was approved by the Institutional Review Board of National Police Hospital (No. 11100176-201608-HR-005). It is a cross-sectional study including 1,899 male police officers ranging from 40 to 59 years who entered in a prostate health screening between March and September 2013 at National Police Hospital. People who were taking drugs affecting prostate physiology, such as antiandrogens and 5-α-reductase inhibitors, who used phosphodiesterase-5 inhibitors daily or nutrients that might adjust mineral or bone metabolism, who had palpable nodules on the digital rectal examination, or who showed a high prostate-specific antigen (PSA) level (>4.0 ng/mL) were not included in our study. Additionally, patients diagnosed with chronic kidney disease were excluded.
All subjects underwent a clinical checking using the IIEF-5 questionnaire translated into Korean. Blood samples were obtained to measure serum PSA, testosterone, and phosphorus between 7:00 AM and 9:00 AM after eight hours fasting. Total PSA was measured by an ABBOTT ARCHITECT i2000 analyzer using the Abbott ARCHITECT Total PSA assay (Abbott Laboratories, Slingo, Ireland). Serum testosterone was calculated by RIA (Parc Marcel Boiteux, Codolet, Cisbio Bioassays Inc., Codolet, France). Serum inorganic phosphorus was determined with a Hitachi 7600-020 (Hitachi Co., Tokyo, Japan) autoanalyzer using HRII Series P-HRII reagent (Wako Pure Cemical Industries Ltd, Osaka, Japan).
Certified version of the IPSS was served to participants to evaluate voiding symptoms. Prostate volume (PV) was measured by transrectal ultrasound (UltraView, BK medical, Copenhagen, Denmark), and digital rectal examination of prostate was also carried out.
Blood pressure was measured over twice (5 minutes apart) in the right arm using a digital blood pressure monitors, were averaged. Waist circumference was measured at the level of uppermost border of hipbones (iliac crest). Records of height and body weight were also collected. Blood was sampled at the same time of day (7:00–9:00 AM) in the 8 hours fasting state. Chemistry tests included measurements of serum glucose, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides. Metabolic syndrome (MetS) was diagnosed in case of three or more of the National Cholesterol Education Program Adult Treatment Panel III for Asians criteria were confirmed [16].
First, one-way analysis of variance tests were assessed to compare the differences in IIEF-5 scores according to other factors, such as age, BMI, testosterone level, PSA, phosphorus, and PV. Chi-square or Fisher exact test were performed to compare the differences in IIEF-5 scores according to the MetS. Second, all subjects were analyzed the simple relationships between IIEF-5 and age, phosphorus, BMI, testosterone, PSA, and PV by the Spearman correlation test. Third, we tested the relationship between IIEF and phosphorus, PV after adjusting for age, testosterone, and MetS using multiple linear regression. Finally, univariate and multivariate logistic regression analyses were underwent to confirm the significance of age, PSA, testosterone, phosphorus, BMI, PV, and MetS as predictors of significant ED (IIEF-5 score ≤11).
The variables were considered statistically significant when p<0.05. We used the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) for statistical analyses.
The clinical characteristics of the 1,899 men are summarized in Table 1. The median value of age, testosterone, and phosphorus were 53.0 years, 4.58 ng/mL, and 3.50 mg/dL, respectively. The median BMI was 24.8 kg/m2, and 33.5% of all patients had MetS. The median IIEF-5 score was 18. To analyze differences in erectile function according to many clinical factors, we divided questionnaire groups into 3 subgroups by the degree of severity (Table 1). In the results, patients with moderate to severe ED had relatively older age, higher phosphorus level, and larger PVs than other two groups (p<0.001, p=0.004, p=0.002, respectively). Other continuous variables were insignificantly different between the three groups. And, moderate to severe ED patients had a higher prevalence of MetS (p=0.021) than other groups.
This findings of the statistical analyses are shown in Table 2. Significant correlation was not found between IIEF-5 and BMI (r=–0.031, p=0.189), testosterone (r=0.033, p=0.148), or PSA (r=–0.007, p=0.769). IIEF-5 was revealed to have a positive correlation with PV (r=–0.065, p=0.004). In addition, age (r=–0.238, p<0.001) and phosphorus level (r=–0.108, p<0.001) were significantly related to IIEF. Serum phosphorus level had the highest correlation with IIEF-5 except age, followed by PV.
However, as shown in Table 3, phosphorus and PV were not significantly correlated with IIEF after adjusting for age. The relationship of IIEF-5 with phosphorus and PV remained insignificant after adjusting for other confounding factors (testosterone and MetS).
Phosphorus, age, and MetS were found to be predictors for moderate to severe ED in the univariate analysis (p=0.007; OR, 1.108; 95% CI, 1.180–1.137; p<0.001; OR, 1.125; 95% CI, 1.093–1.159; and p=0.010; OR, 1.372; 95% CI, 1.078–1.745, respectively). And, testosterone, PSA, BMI, and PV were not predictive factors for ED. Phosphorus, age, and MetS were independent predictive factors for moderate to severe ED (p=0.048; OR, 1.101; 95% CI, 1.076–1.131; p<0.001; OR, 1.119; 95% CI, 1.086–1.153; and p=0.048; OR, 1.283; 95% CI, 1.003–1.641, respectively) in the multivariate analysis (Table 4).
In this study, we demonstrated that phosphorus is significantly related to IIEF. Serum phosphorus level had the highest correlation coefficient with IIEF-5, and the severity of ED was greater in patients with elevated phosphorus levels. In the multivariate analysis, we also found that age, MetS, and phosphorus are independent predictive factors of moderate to severe ED.
The IIEF is, today, one of the most commonly used forms for men presenting with sexual complaints. On the IIEF, ED is classified from mild to severe [17]. To date, this is the first research to study the association between phosphorus and ED. It is also the first study to evaluate that association using IIEF score and a detailed prostate work-up. Even after multivariate logistic regression analysis including traditional ED confounding factors, we revealed that phosphorus is a meaningful predictive factor of severe ED.
In previous in vitro studies, hyperphosphatemia leads a phenotypic converting vascular smooth muscle cells to osteoblast-like cells that generate biochemical markers of bone lineage, for example, Runx2, creating calcification [18]. Furthermore, excessive phosphorus diet has been appeared to induce endothelial dysfunction in young age, and a phosphorus-enriched medium induces bovine aortic endothelial cells to generate greater amounts of reactive oxygen species [19]. One nephrology study group [5] revealed that higher serum phosphorus level, even in the normal range, had independent association with the occurrence of coronary vessel calcification fifteen years later in young adults with normal renal function. Recently, in Korea, one study group demonstrated that a higher phosphorus concentration, even within a normal value, may be related with higher coronary vessel calcification in healthy adults, and the effects did not change given racial or regional difference [20]. Except in cases with CAD, Yao et al. [21] said that high phosphorus level causes calcification in great vessel through the influence of β-catenin in subjects with chronic kidney disease. Recent evidence has proposed that the serum phosphorus is associated with clinical and subclinical CVD in the normal population and it may differ by gender [2223]. In addition, high serum phosphorus levels had an association between carotid intima-media thickness and CVD risks in males, but not in females [2223]. This relationship may be related to declines in endogenous estradiol that occur during the menopausal transition in women. In a large cohort of community-living Italians, Cirillo et al. [24] demonstrated that at the age 45–50 years, there was a significant increase in serum phosphorus and a comparable decrease in urinary phosphorus excretion in females, but not males. And, in a large population of older men, serum estradiol levels and phosphorus levels were inversely correlated, independent of kidney function, vitamin D levels, parathyroid hormone concentration, and bone density [25].
Vascular calcification and endothelial dysfunction are both related to the atherosclerotic process, and obstruction of atherosclerotic sites are closely associated with calcifications of vascular endothelium [26]. There are several hypotheses on the pathophysiology of ED as a sentinel marker of vascular dysfunction. The artery size hypothesis stipulates that ED is an early symptom of systemic atherosclerosis [27]. Assuming that atherosclerosis progresses in all major vascular beds at a relatively similar pace, those authors argued that symptoms will manifest earlier in the smaller arterial branches such as the penile artery rather than in the larger vessels of the heart and limbs, which are able to better tolerate the same degree of atherosclerosis or obstruction [27]. In accordance with this hypothesis, Rogers et al. [28] found that the degree of stenosis in the internal pudendal arteries was similar to that found in the coronary artery (52% to 65%) and that the average diameter of the internal pudendal artery was just slightly smaller than the average diameter of the coronary artery. Hamur et al. [29] reported that CAD may increase as the severity of ED increases. This also implies that the increased atherosclerotic plaque burden in patients with stable CAD is systemic and may be associated with endothelial dysfunction, especially when the fact that patients with severe ED and stable CAD may have high Syntax scores is taken into account. In clinical practice, phosphorus levels in men are not routinely measured prior to a health work-up and treatment. In view of this point, our study underlines the usefulness of serum phosphorus measurement in the health screening process as a predictor of ED.
This study has some limitations. First, it has the disadvantages inherent in a retrospective design. Therefore, this study was not including the various factors affecting erectile function in men such as insulin-like growth factor-1, several cytokines, and C-reactive protein. Second, the cross-sectional design rules out the evaluation of causality and may have temporality among the variables. Third, our study cannot rule out the possibility that outcomes were affected by phosphorus intake and, consequently, that personal dietary habits might disrupt the relation between phosphorus levels and morbidity rates. Finally, in this study, we did not observe the vitamin D and parathyroid related parameters.
However, our sample size was relatively large and mostly homogeneous. And it did not include subjects with chronic kidney disease. We also excluded subjects who were taking drugs affecting prostate physiology, who used phosphodiesterase-5 inhibitors daily or nutrients that might adjust mineral or bone metabolism. There have been no reported cross-sectional studies evaluating the role of phosphorus as a predictive factor of ED. We suggest that serum phosphorus level is a nontraditional potential risk factor of ED in the healthy men. In modern society, we tend to intake less of natural meal and more of processed it. Processed foods usually have high-phosphate additives and may affect phosphate intake more than recommended amounts [30]. Known harmful effects of a high-phosphate diet on the body is not enough to be well understood. Given the increasing evidence of relationship between phosphorus and several metabolic diseases, prospective well-designed studies are required. In that study, interventions reducing phosphate intake, such as restriction of dietary phosphorus and adjustment of food additives, have to be included. They can reduce the rates of metabolic diseases including ED in high-risk patients or in the healthy population in the future. Nowadays, there are no established guidelines for serum phosphorus intake in the general population. Managing the causes of increased serum phosphorus and thereby correcting elevated serum phosphorus levels in individuals may be a relevant therapeutic target in preventing the excess risk of ED. Future studies, however, should confirm the causality of the relationship between the simultaneous existence of serum phosphorus and the risk of ED. In addition, basic research into all types of minerals and ED merits further investigation.
Age, MetS, and phosphorus levels are significantly associated with ED. We found that, in clinically stable middle-aged men, serum phosphorus was strongly associated with ED. And, recommended serum phosphorus levels could be different for males than for females. Given this finding, handling of phosphorus in men may have a particular meaning of reducing the risk of ED.
Figures and Tables
Table 1
Patients' characteristics according to IIEF-5 degree (n=1,899)

Table 2
Spearman correlations of IIEF-5 score with age, phosphorus, testosterone, PSA, and PV
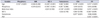
Table 3
Multiple linear regression test of IIEF-5 score with phosphorus level and prostate volume

Table 4
Logistic regression analysis predicting the moderate to severe erectile dysfunction (IIEF-5≤11)

References
1. Bellasi A, Kooienga L, Block GA. Phosphate binders: new products and challenges. Hemodial Int. 2006; 10:225–234.
2. Kumar R. Vitamin D metabolism and mechanisms of calcium transport. J Am Soc Nephrol. 1990; 1:30–42.
3. Lederer E. Regulation of serum phosphate. J Physiol. 2014; 592:3985–3995.
4. Amann K, Törnig J, Kugel B, Gross ML, Tyralla K, El-Shakmak A, et al. Hyperphosphatemia aggravates cardiac fibrosis and microvascular disease in experimental uremia. Kidney Int. 2003; 63:1296–1301.
5. Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA. Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol. 2009; 20:397–404.
6. Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA. Serum phosphate and left ventricular hypertrophy in young adults: the coronary artery risk development in young adults study. Kidney Blood Press Res. 2009; 32:37–44.
7. Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007; 120:151–157.
8. Chiurlia E, D'Amico R, Ratti C, Granata AR, Romagnoli R, Modena MG. Subclinical coronary artery atherosclerosis in patients with erectile dysfunction. J Am Coll Cardiol. 2005; 46:1503–1506.
9. Vlachopoulos C, Rokkas K, Ioakeimidis N, Stefanadis C. Inflammation, metabolic syndrome, erectile dysfunction, and coronary artery disease: common links. Eur Urol. 2007; 52:1590–1600.
10. Austoni E, Mirone V, Parazzini F, Fasolo CB, Turchi P, Pescatori ES, et al. Smoking as a risk factor for erectile dysfunction: data from the Andrology Prevention Weeks 2001-2002 a study of the Italian Society of Andrology (s.I.a.). Eur Urol. 2005; 48:810–817.
11. Chen S, Wu R, Huang Y, Zheng F, Ou Y, Tu X, et al. Insulin resistance is an independent determinate of ED in young adult men. PLoS One. 2013; 8:e83951.
12. Chew KK, Bremner A, Jamrozik K, Earle C, Stuckey B. Male erectile dysfunction and cardiovascular disease: is there an intimate nexus? J Sex Med. 2008; 5:928–934.
13. Corona G, Monami M, Boddi V, Balzi D, Melani C, Federico N, et al. Is obesity a further cardiovascular risk factor in patients with erectile dysfunction? J Sex Med. 2010; 7:2538–2546.
14. Corona G, Monami M, Boddi V, Cameron-Smith M, Lotti F, de Vita G, et al. Male sexuality and cardiovascular risk. A cohort study in patients with erectile dysfunction. J Sex Med. 2010; 7:1918–1927.
15. Krane RJ, Goldstein I, Saenz de Tejada I. Impotence. N Engl J Med. 1989; 321:1648–1659.
16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752.
17. Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999; 11:319–326.
18. Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000; 87:E10–E17.
19. Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, et al. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol. 2009; 20:1504–1512.
20. Park KS, Park J, Choi SH, Ann SH, Singh GB, Shin ES, et al. Serum phosphorus concentration and coronary artery calcification in subjects without renal dysfunction. PLoS One. 2016; 11:e0151007.
21. Yao L, Sun YT, Sun W, Xu TH, Ren C, Fan X, et al. High phosphorus level leads to aortic calcification via β-catenin in chronic kidney disease. Am J Nephrol. 2015; 41:28–36.
22. Onufrak SJ, Bellasi A, Cardarelli F, Vaccarino V, Muntner P, Shaw LJ, et al. Investigation of gender heterogeneity in the associations of serum phosphorus with incident coronary artery disease and all-cause mortality. Am J Epidemiol. 2009; 169:67–77.
23. Onufrak SJ, Bellasi A, Shaw LJ, Herzog CA, Cardarelli F, Wilson PW, et al. Phosphorus levels are associated with subclinical atherosclerosis in the general population. Atherosclerosis. 2008; 199:424–431.
24. Cirillo M, Ciacci C, De Santo NG. Age, renal tubular phosphate reabsorption, and serum phosphate levels in adults. N Engl J Med. 2008; 359:864–866.
25. Meng J, Ohlsson C, Laughlin GA, Chonchol M, Wassel CL, Ljunggren O, et al. Associations of estradiol and testosterone with serum phosphorus in older men: the Osteoporotic Fractures in Men study. Kidney Int. 2010; 78:415–422.
26. Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998; 31:126–133.
27. Montorsi P, Ravagnani PM, Galli S, Rotatori F, Briganti A, Salonia A, et al. The artery size hypothesis: a macrovascular link between erectile dysfunction and coronary artery disease. Am J Cardiol. 2005; 96(12B):19M–23M.
28. Rogers JH, Karimi H, Kao J, Link D, Javidan J, Yamasaki DS, et al. Internal pudendal artery stenoses and erectile dysfunction: correlation with angiographic coronary artery disease. Catheter Cardiovasc Interv. 2010; 76:882–887.
29. Hamur H, Duman H, Keskin E, Inci S, Kucuksu Z, Degirmenci H, et al. The relation between erectile dysfunction and extent of coronary artery disease in the patients with stable coronary artery disease. Int J Clin Exp Med. 2015; 8:21295–21302.
30. Calvo MS, Park YK. Changing phosphorus content of the U.S. diet: potential for adverse effects on bone. J Nutr. 1996; 126:4 Suppl. 1168S–1180S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download