Abstract
Purpose
The goal of this study was to compare the rate of systemic inflammatory response syndrome (SIRS) in high-risk patients undergoing percutaneous nephrolithotomy (PCNL) between patients who received 7, 2, or 0 days of preoperative antibiotics.
Materials and Methods
We retrospectively reviewed a series of consecutive PCNLs performed at our institution. Patients with infected preoperative urine cultures were excluded. High-risk patients were defined as those with a history of previous urinary tract infection (UTI), hydronephrosis, or stone size ≥2 cm. Patients were treated with 7, 2, or 0 days of preoperative antibiotic prophylaxis prior to PCNL. All patients received a single preoperative dose of antibiotics within 60 minutes of the start of surgery. Fisher exact test was used to compare the rate of SIRS by preoperative antibiotic length.
Results
Of the 292 patients identified, 138 (47.3%) had sterile urine and met high-risk criteria, of which 27 (19.6%), 39 (28.3%), and 72 (52.2%) received 7, 2, and 0 days of preoperative antibiotics, respectively. The 3 groups were similar in age, sex, and duration of surgery (p>0.05). There was no difference in the rate of SIRS between the groups, with 1 of 27 (3.7%), 2 of 39 (5.1%) and 3 of 72 patients (4.2%) meeting criteria in the 7, 2, and 0 days antibiotic groups (p=~1).
Urolithiasis is one of the most common urologic conditions, and it has recently been estimated that the prevalence of stones in Americans is 8.8% [1]. In 2000, the United States spent in excess of 2 billion dollars treating stone disease [2]. Percutaneous nephrolithotomy (PCNL) is widely accepted as the ideal surgical choice for patients with a large stone burden and is becoming an increasingly common operation. In the United States, the number of PCNLs performed has more than doubled in the last decade, and its use may continue to increase in future years [3].
Urosepsis is a well-known and potentially life-threatening complication following PCNL for staghorn and large renal calculi. While the overall incidence of urosepsis in the reported literature is approximately 1%, the historical mortality rate of post-PCNL sepsis is as high as 66%–80% [45]. More commonly, patients experience less severe symptoms of infection postoperatively, including fever (21%–74%), bacteriuria (10%–37%), and bacteremia (20%–35%) [678]. Due to the prevalence of infection-related complications and potential consequences of severe infection after PCNL, both the American Urological Association (AUA) and European Association of Urology (EAU) clinical practice statements have formulated specific recommendations regarding preoperative antibiotic prophylaxis in this patient population.
The AUA Best Practice Statement regarding antimicrobial prophylaxis recommends that all patients undergoing PCNL receive antibiotic prophylaxis for a duration of 24 hours or less. Similarly, the 2015 guidelines set forth by the EAU confers a grade "A" recommendation for the treatment of all stones >2 cm with PCNL [9]. The EAU guidelines also note that a single preoperative dose appears to be effective. However, recommendations for the empiric perioperative antibiotic treatment of specific populations (e.g., high-risk patients) are not provided. This is due in large part to a paucity of data in the urological literature [1011]. Anecdotally, some urologists may prescribe extended antibiotics in those deemed to be high-risk for developing postoperative infection, such as patients with staghorn calculi or a history of recurrent urinary tract infection (UTI). We sought to evaluate a cohort of high-risk patients undergoing PCNL and compare the rates of systemic inflammatory response syndrome (SIRS) in those who received 7, 2, or 0 days (intraoperative dose only) of preoperative antibiotics.
After Institutional Review Board approval (201304085), data was retrospectively reviewed from a prospectively maintained database of all patients undergoing PCNL by 2 surgeons at our institution from January 2012 to June 2014. All patients at our institution must have a negative preoperative urine culture within 7 days of surgery. Those who had a previous positive urine culture within 30 days prior to surgery were excluded from analysis. High-risk criteria were selected based on previous literature which demonstrated an association between post-PCNL infectious complications and the following preoperative variables: (1) presence of hydronephrosis, (2) stone size in greatest dimension of ≥2 cm, and (3) history of recurrent UTIs [1213]. Patients were considered high-risk for postoperative infectious complications (e.g., SIRS) if they manifested one of these variables. The present study included patients with a history of UTI, which was defined as having symptomatic, culture-proven bacteriuria. Evaluation of hydronephrosis and quantification of stone burden were performed by both the treating urologist and by a fellowship-trained abdominal radiologist. The etiology of the hydronephrosis (i.e., presence of a ureteral stone versus ureteropelvic junction obstruction by a renal pelvic stone) was not distinguished. SIRS criteria were defined as having 2 or more of the following clinical parameters simultaneously during the postoperative hospitalization: (1) temperature ≥38℃ or ≤36℃, (2) heart rate >100 beats/min, (3) respiratory rate >20 breaths/min, and (4) white blood cell count (WBC) >12,000/µL or <4,000/µL [12]. Complications were categorized via the Clavien-Dindo classification system [14].
Formerly, the clinical practice of one author (ACD) included 7-day oral antibiotic administration preoperatively for high-risk PCNL patients. After consultation with infectious disease specialists and pharmacists at our institution, the practice was changed to 2 days of preoperative treatment, as 2 days of treatment suffices to reach therapeutic serum drug levels. The clinical practice of another author (BMB) includes a single, preoperative dose of antibiotics within 60 minutes of the start of the operation. Therefore, 3 groups of patients exist in our institutional experience: those receiving 7, 2, and 0 days of antibiotics before PCNL. All patients received a preoperative dose of antibiotics within 1 hour of the start of the case. Choice of preoperative, intravenous antibiotic was consistent with AUA guidelines (1st/2nd generation cephalosporin or fluoroquinolone as an alternative), with the exception of patients with a history of resistant organisms. Choice of oral antibiotic was ciprofloxacin 500 mg twice daily (adjusted as necessary for renal function), except in the setting of a previous resistant organism.
The indications for PCNL were based on the composite of multiple factors, including stone size, configuration, location, expected (or historical) composition, and patient preference. An external ureteral catheter was placed cystoscopically at the beginning of each procedure. Patients were positioned prone. Energy sources employed for lithotripsy included ultrasonic, pneumatic, and holmium laser. Percutaneous access was established by fellowship-trained interventional radiologists. Nephrostomy tube and ureteral stent were placed at the discretion of the urologist. Routinely, nephrostomy tubes were removed prior to patient discharge from the hospital, while ureteral stents remained in place for 1 to 2 weeks postoperatively. Vital signs were assessed after surgery every 15 minutes for the first hour, every 30 minutes for the second hour, and every 4 hours thereafter. WBC counts were checked at the discretion of the surgeon.
A total of 292 patients underwent PCNL during the study period, of which 138 met inclusion criteria. Twenty-seven, 39, and 72 patients were treated with 7, 2, or 0 days of preoperative antibiotics. There were no significant differences in baseline characteristics, including age, body mass index, sex, duration of surgery, stone size, hydronephrosis, and a history of UTI (p>0.05) (Table 1). The specific signs and overall rates of SIRS for each of the three groups are shown in Table 2. Although there was no statistically significant difference in rates of SIRS between the groups, the number of patients with WBC>12,000/µL or <4,000/µL was significantly higher for the 7 days of antibiotics group (18.5%, vs. 5.1% for 2 days, and 2.8% for 0 days, p=0.02). Two patients required postoperative intensive care unit admission. Urine or blood culture data was available for 5 of 6 patients with SIRS. Table 3 reports the clinical and operative data for each of the patients with SIRS.
In the 7- and 2-day groups, 50 patients (75.7%) received oral ciprofloxacin as their preoperative antibiotic. The remainder of patients received antibiotics tailored to their history of prior positive cultures. Percutaneous access was supracostal in 85 patients (61.6%) and subcostal in 53 patients (38.4%). Mean operative time and blood loss were 127.2±57.4 minutes and 38.1±79.1 mL, respectively. Table 1 details the operative data for the groups that received 7, 2, and 0 days of preoperative antibiotic. There was a significant difference in operative time, with those in the group that received 0 days of antibiotics having a shorter time (p<0.001). Median length of stay was 1 day (range, 1–14 days). Nine patients required a second-look PCNL for residual stone burden. Six patients had a Clavien-Dindo grade II complication manifest by hemorrhage requiring transfusion. Four patients had Clavien-Dindo grade IIIa complications, including pneumothorax (2), hydrothorax (1), and hemothorax (1). Pneumothorax, hydrothorax, and hemothorax were managed with temporary chest tube drainage.
PCNL is generally safe and effective for the treatment of large renal calculi and is considered first-line treatment for staghorn stones [9151617]. While the risk of development of any postoperative UTI is relatively high (e.g., fever and bacteriuria develop in 21%–74% and 10%–37%, respectively) [678], the risk of a severe infectious complication (i.e., sepsis), is low (0.2%–4.7%) [1518]. Thus, trepidation exists regarding extended perioperative antibiotic use for PCNL, as the sequelae of post-PCNL sepsis can be calamitous [45]. While recent work has established that single-dose antibiotic coverage is adequate for low-risk patients with sterile preoperative urine [6], little is known about preoperative antibiotic prophylaxis in high-risk patients. In the present study, no difference in occurrence of SIRS was found between high-risk patients who received 7, 2, or 0 days of preoperative antibiotics (p=~1).
Infectious complications following PCNL can occur despite sterile preoperative urine culture, making prevention of these complications difficult. Additionally, treating positive preoperative urine cultures does not eliminate the risk of postoperative SIRS [19]. Previous studies regarding antibiotic prophylaxis for PCNL have suggested that extended prophylactic antibiotic therapy prior to the day of surgery may, in fact, reduce the risk of SIRS and infectious complications in high-risk patients with sterile urine. Bag et al. [20] randomized patients to 7 days of prophylaxis with nitrofurantoin versus standard prophylaxis prior to PCNL and noted a reduction in infectious complications: 19% vs. 49%, respectively. Similarly, Mariappan et al. [12] prospectively evaluated 2 groups of high-risk patients undergoing PCNL: those who received 7 days of ciprofloxacin versus those who received standard prophylaxis. The authors also noted a reduction in the incidence of SIRS. The risk of SIRS for those receiving single-dose prophylaxis was approximately 3 times that of those receiving extended prophylaxis (relative risk, 2.9; 95% confidence interval, 1.3–6.3, p=0.004). Despite these findings, the topic of proper antibiotic prophylaxis in high-risk patients undergoing PCNL continues to debated, as evidenced by the Best Practice Statement put forth by the AUA.
The results of the present study conflict with those of the prospective work by Mariappan et al. [12] and Bag et al. [20]. One major difference in our series was the rate of SIRS: 3.7%, 5.1%, and 4.2% in those receiving 7, 2, and 0 days of preoperative antibiotics, whereas Mariappan et al. [12] found rates of SIRS to be 13.5% and 39.1% in the treatment and control arms, respectively. Much of this difference may be attributed to an ascertainment bias, given the retrospective nature of the present study. Furthermore, more complete stone culture data may have been illustrative and would be important in future, prospective studies. Variability in SIRS rates could be validated by differences in positive stone culture rates, as stone cultures are more closely related to the development of sepsis than urine culture alone [2021].
Previously reported rates of SIRS after PCNL demonstrate a wide range: 9.8%–56.7% [2122]. This variability may be attributed to several causes. First, those studies employing prospective, standardized protocols may be more likely to detect clinical signs of SIRS, as opposed to retrospective designs. Second, the criteria for inclusion varies amongst PCNL studies, with some studies excluding high-risk patients, those with worrisome findings at the time of access, and those with positive preoperative urine cultures. The definition of SIRS has also been inconsistent across studies. Further, the antibiotic regimens both pre- and postoperatively have differed in the literature. Although the rates presented herein appear to be lower than those in previous manuscripts, Dogan et al. [23] reported a similar rate of 1.5% in 338 patients.
While the present study investigates the use of preoperative antibiotics, others have evaluated the need for prophylactic antibiotic coverage after PCNL. Recent work by Deshmukh et al. [24] showed that adherence to the AUA's Best Practice recommendations of a single, preoperative dose did not result in a higher post-PCNL infection rate compared to those who received ~6 days of postoperative antibiotics. Similarly, Dogan et al. [25] found no difference in rates of post-PCNL fever in patients who received a single preoperative dose versus a postoperative course extending to nephrostomy tube removal. Seyrek et al. [22] prospectively randomized 198 patients to receive a single postoperative dose, an additional dose at 12 hours post-PCNL, or antibiotics until the time of nephrostomy tube removal. The authors found no difference in rates of SIRS between the groups. Tuzel et al. [26] reported on 73 patients randomized to a single preoperative dose or a regimen to be extended postoperatively until the time of nephrostomy tube removal. They found no difference in either fever or septicemia.
Owing to the potential for severe infectious complications, the anecdotal and surgeon-specific use of an extended course of antibiotics is understandable. Evidence continues to emerge, however, supporting the use of short-course or single intraoperative doses of antibiotics. Moreover, both the AUA and EAU have recommended such prophylaxis. The potential overuse of antibiotics, and the associated increase in highly-resistant organisms, is of paramount concern. Antibiotic stewardship will be vital to the future effective prevention and treatment of UTIs. Cai et al. [27] reported their experience of antibiotic use, infection, and prevalence of drug-resistant uropathogens by comparing 2,619 and 3,529 patients who underwent a urologic procedure before and after the implementation of an antibiotic protocol that was consistent with the EAU's guidelines. During the study period they found a similar rate of infections. There was also a significant decrease in use of antibiotics, decreased cost, and decreased rates of resistance to antibiotics (ciprofloxacin, piperacillin-tazobactam, and gentamicin).
The present study has limitations. First, it is a retrospective review of a single-center experience. Certainly biases such as patient selection for PCNL could be manifest. Furthermore, due to the retrospective collection of data, the availability of postoperative antibiotic administration and complete blood, urine, and stone culture data in each patient is lacking. The clinical outcome of sepsis could not be studied in the present work due to the lack of uniform blood culture data. Ideally, in future prospective studies, blood cultures would be obtained in any patient who meets one SIRS criterion, while urine and stone cultures would be obtained in all patients postoperatively. Differences in the culture collection practices were surgeon-specific; the difference between surgeons also explains the significant difference in operative times (the surgeon for the group that received zero of preoperative antibiotics group had significantly lower operative times than the other surgeon, p<0.001). Additionally, the small number of patients who developed SIRS limits the ability to perform further statistical evaluations such as a multivariate analysis designed to identify predictors of SIRS after PCNL. Also, during the study period, the specific antibiotic was not standardized amongst surgeons, although selection was based on either AUA guidelines or previous positive culture sensitivities. Finally, the use of the terms SIRS and sepsis have become more precise in recent years and are now well-defined [28]. We chose to employ the definition used by Mariappan et al. [12] for simplicity and comparability.
Extended preoperative antibiotic prophylaxis was not found to reduce the risk of SIRS after PCNL in our institutional experience of high-risk patients. For these patients, a single preoperative dose of antibiotics is sufficient, which supports the recommendations made by both the AUA and EAU for preoperative antibiotic therapy before PCNL. Future, large, and prospective studies may address the predictors of SIRS after PCNL, investigating whether extended preoperative antibiotic regimens may be helpful.
Figures and Tables
Table 1
Patient clinical and operative data

Table 2
Signs of SIRS after percutaneous nephrolithotomy in patients receiving different durations of preoperative antibiotics

Table 3
Clinical and operative data of patients with systemic inflammatory response syndrome
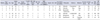
abx, antibiotics; UTI, urinary tract infection; T, temperature; HR, heart rate; RR, respiratory rate; WBC, white blood cell count; ICU, intensive care unit admission; LOS, length of stay; cx, culture; NT, nephrostomy tube; EBL, estimated blood loss; OR, operating room; Y, yes; N, no; NA, not available; Neg, negative; B12, below the 12th rib; A12, above the 12th, but below the 11th rib; A11, above the 11th rib; Coag-neg staph, Coagulase-negative staphylococci; sm, small or minimal
References
1. Scales CD Jr, Smith AC, Hanley JM, Saigal CS. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012; 62:160–165.
2. Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J Urol. 2005; 173:848–857.
3. Jayram G, Matlaga BR. Contemporary practice patterns associated with percutaneous nephrolithotomy among certifying urologists. J Endourol. 2014; 28:1304–1307.
4. O'Keeffe NK, Mortimer AJ, Sambrook PA, Rao PN. Severe sepsis following percutaneous or endoscopic procedures for urinary tract stones. Br J Urol. 1993; 72:277–283.
5. Draga RO, Kok ET, Sorel MR, Bosch RJ, Lock TM. Percutaneous nephrolithotomy: factors associated with fever after the first postoperative day and systemic inflammatory response syndrome. J Endourol. 2009; 23:921–927.
6. Gravas S, Montanari E, Geavlete P, Onal B, Skolarikos A, Pearle M, et al. Postoperative infection rates in low risk patients undergoing percutaneous nephrolithotomy with and without antibiotic prophylaxis: a matched case control study. J Urol. 2012; 188:843–847.
7. Kumar S, Bag S, Ganesamoni R, Mandal AK, Taneja N, Singh SK. Risk factors for urosepsis following percutaneous nephrolithotomy: role of 1 week of nitrofurantoin in reducing the risk of urosepsis. Urol Res. 2012; 40:79–86.
8. Bootsma AM, Laguna Pes MP, Geerlings SE, Goossens A. Antibiotic prophylaxis in urologic procedures: a systematic review. Eur Urol. 2008; 54:1270–1286.
9. Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016; 69:475–482.
10. Wolf JS Jr, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008; 179:1379–1390.
11. Grabe M, Bjerklund-Johansen TE, Botto H, Çek M, Naber KG, Tenke P, et al. Guidelines on urological infections [Internet]. Arnhem: European Association of Urology;2010. cited 2016 Feb 12. Available from: http://uroweb.org/wp-content/uploads/Urological-Infections-2010.pdf.
12. Mariappan P, Smith G, Moussa SA, Tolley DA. One week of ciprofloxacin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. BJU Int. 2006; 98:1075–1079.
13. Koras O, Bozkurt IH, Yonguc T, Degirmenci T, Arslan B, Gunlusoy B, et al. Risk factors for postoperative infectious complications following percutaneous nephrolithotomy: a prospective clinical study. Urolithiasis. 2015; 43:55–60.
14. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
15. Kreydin EI, Eisner BH. Risk factors for sepsis after percutaneous renal stone surgery. Nat Rev Urol. 2013; 10:598–605.
16. de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, et al. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011; 25:11–17.
17. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS Jr, et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005; 173:1991–2000.
18. Labate G, Modi P, Timoney A, Cormio L, Zhang X, Louie M, et al. The percutaneous nephrolithotomy global study: classification of complications. J Endourol. 2011; 25:1275–1280.
19. Erdil T, Bostanci Y, Ozden E, Atac F, Yakupoglu YK, Yilmaz AF, et al. Risk factors for systemic inflammatory response syndrome following percutaneous nephrolithotomy. Urolithiasis. 2013; 41:395–401.
20. Bag S, Kumar S, Taneja N, Sharma V, Mandal AK, Singh SK. One week of nitrofurantoin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. Urology. 2011; 77:45–49.
21. Korets R, Graversen JA, Kates M, Mues AC, Gupta M. Postpercutaneous nephrolithotomy systemic inflammatory response: a prospective analysis of preoperative urine, renal pelvic urine and stone cultures. J Urol. 2011; 186:1899–1903.
22. Seyrek M, Binbay M, Yuruk E, Akman T, Aslan R, Yazici O, et al. Perioperative prophylaxis for percutaneous nephrolithotomy: randomized study concerning the drug and dosage. J Endourol. 2012; 26:1431–1436.
23. Dogan HS, Guliyev F, Cetinkaya YS, Sofikerim M, Ozden E, Sahin A. Importance of microbiological evaluation in management of infectious complications following percutaneous nephrolithotomy. Int Urol Nephrol. 2007; 39:737–742.
24. Deshmukh S, Sternberg K, Hernandez N, Eisner BH. Compliance with American Urological Association guidelines for post-percutaneous nephrolithotomy antibiotics does not appear to increase rates of infection. J Urol. 2015; 194:992–996.
25. Doğan HS, Sahin A, Cetinkaya Y, Akdoğan B, Ozden E, Kendi S. Antibiotic prophylaxis in percutaneous nephrolithotomy: prospective study in 81 patients. J Endourol. 2002; 16:649–653.
26. Tuzel E, Aktepe OC, Akdogan B. Prospective comparative study of two protocols of antibiotic prophylaxis in percutaneous nephrolithotomy. J Endourol. 2013; 27:172–176.
27. Cai T, Verze P, Brugnolli A, Tiscione D, Luciani LG, Eccher C, et al. Adherence to European Association of Urology Guidelines on Prophylactic Antibiotics: An Important Step in Antimicrobial Stewardship. Eur Urol. 2016; 69:276–283.
28. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003; 29:530–538.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download